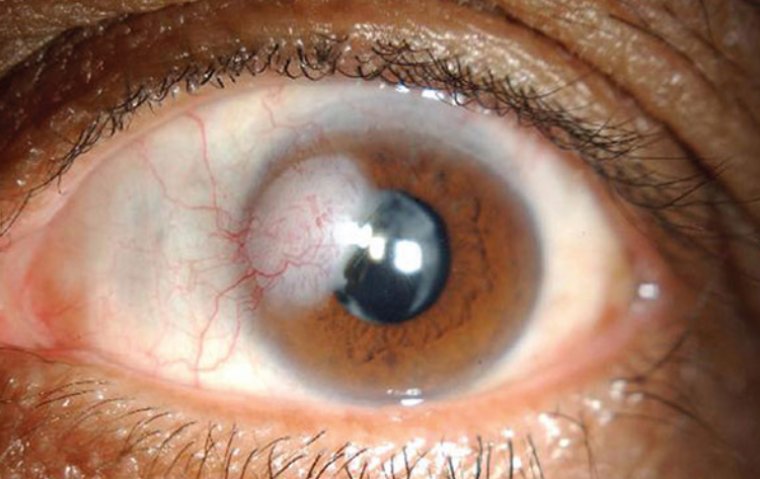
Corneal Opacity: Symptoms and Signs to Watch Out For
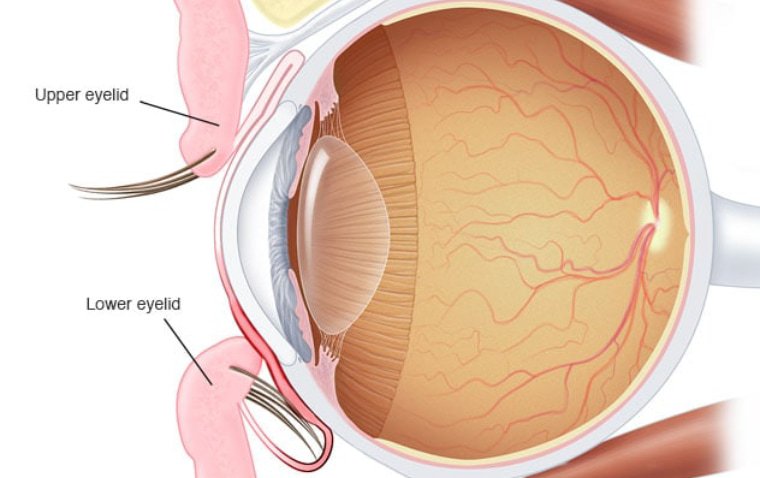
Corneal opacity refers to the clouding or loss of transparency in the cornea, the clear, dome-shaped front part of the eye. It can significantly impair vision and lead to various visual disturbances.
This comprehensive article aims to provide a detailed overview of corneal opacity, including its causes, symptoms, diagnosis, and available treatment options. Understanding these aspects is crucial for accurate diagnosis, timely intervention, and improved outcomes for individuals affected by corneal opacity.
How Does Corneal Opacity Occur?
The cornea plays a vital role in vision by refracting light and focusing it onto the retina. When the cornea becomes opaque, it interferes with light transmission, resulting in visual impairment. Corneal opacity can occur due to various factors, including injury, infection, genetic disorders, and degenerative conditions.
Causes of Corneal Opacity
1. Traumatic Causes: Corneal injuries, chemical burns, foreign body penetration, or surgical complications can result in corneal opacity.
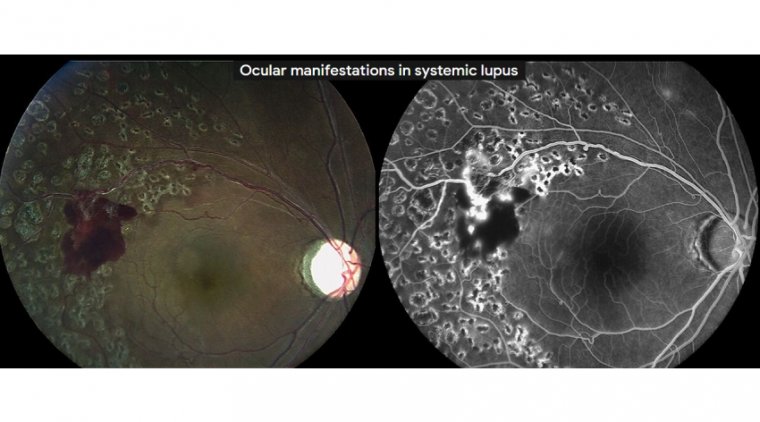
2. Inflammatory Causes: Conditions such as keratitis, uveitis, and aut immüne diseases can cause corneal inflammation and opacity.
3. Infectious Causes: Bacterial, viral, fungal, or parasitic infections can lead to corneal opacity.
4. Genetic Causes: Various genetic disorders like congenital corneal dystrophies and metabolic disorders may result in corneal opacity.
5. Degenerative Causes: Age-related changes, corneal degenerations, and certain systemic diseases can contribute to corneal opacity.
Symptoms of Corneal Opacity
Symptoms of corneal opacity can vary depending on the severity and underlying cause of the condition. Here are some common symptoms associated with corneal opacity:
● Blurred or cloudy vision
● Sensitivity to light
● Eye redness
● Eye pain or discomfort
● Excessive tearing
How to Diagnose Corneal Opacity
Clinical Evaluation: An ophthalmologist examines the eye using a slit lamp biomicroscope to assess corneal opacity, its location, and associated findings.
Visual Acuity Testing: Measurement of visual acuity helps determine the extent of visual impairment. Corneal Topography: Corneal mapping helps identify irregularities and evaluate the corneal shape.
Imaging Techniques: Optical coherence tomography (OCT) and confocal microscopy provide detailed cross-sectional images of the cornea, aiding in diagnosis and treatment planning.
Treatment Options for Corneal Opacity
● Medications: Depending on the underlying cause, topical or systemic medications may be prescribed to manage inflammation, infection, or underlying systemic conditions.
● Contact Lenses: Specialty contact lenses, such as scleral lenses or bandage lenses, can improve vision by creating a smooth refractive surface.
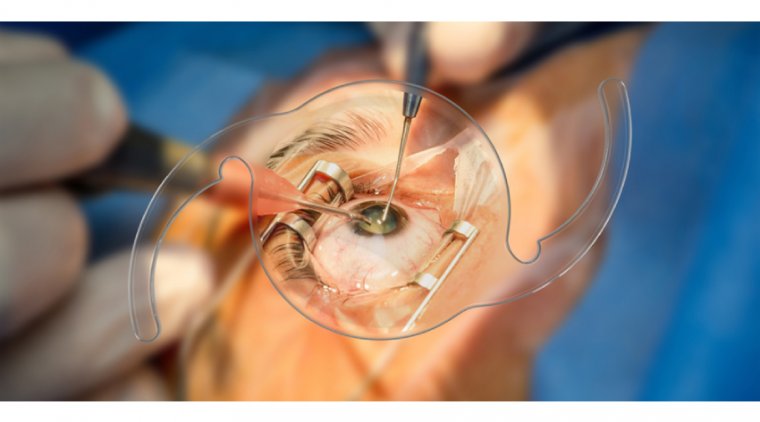
● Corneal Transplantation: In cases where corneal opacity is severe and vision cannot be adequately restored, corneal transplantation, including full-thickness or partial-thickness grafts, may be necessary.
● Advanced Therapies: Emerging treatments such as corneal collagen cross-linking, amniotic membrane transplantation, and artificial corneas show promise in specific cases of corneal opacity.
5 Tips to Reduce the Risk of Corneal Opacity
1. Protect your eyes from trauma: Wear appropriate eye protection, such as safety goggles or glasses, during activities that pose a risk of eye injury, such as sports, construction work, or handling hazardous materials.
2. Protect your eyes from UV radiation: Wear sunglasses that provide 100% UV protection when outdoors, as long-term exposure to UV radiation can increase the risk of corneal disorders.
3. Avoid rubbing your eyes: Rubbing your eyes excessively can increase the risk of corneal injury or damage. If your eyes feel irritated, use lubricating eye drops recommended by your eye care professional instead.
4. Regular eye examinations: Schedule routine eye examinations with an eye care professional. Regular check-ups can help detect any early signs of corneal abnormalities or other eye conditions.
5. Manage underlying health conditions: If you have systemic conditions like diabetes or autoimmune diseases, work closely with your healthcare provider to manage them effectively. Proper management of underlying health conditions can help reduce the risk of corneal opacity.
Summary
Corneal opacity is a significant cause of visual impairment worldwide. Understanding the types, causes, diagnosis, and treatment options associated with corneal opacity is essential for accurate diagnosis and effective management. Ophthalmologists and healthcare providers should collaborate to provide timely interventions and improve the visual outcomes for individuals affected by corneal opacity. Further research and advancements in treatment modalities will continue to enhance the quality of care for patients with corneal opacity.
(1).jpg)