Nocturnal Lagophthalmos
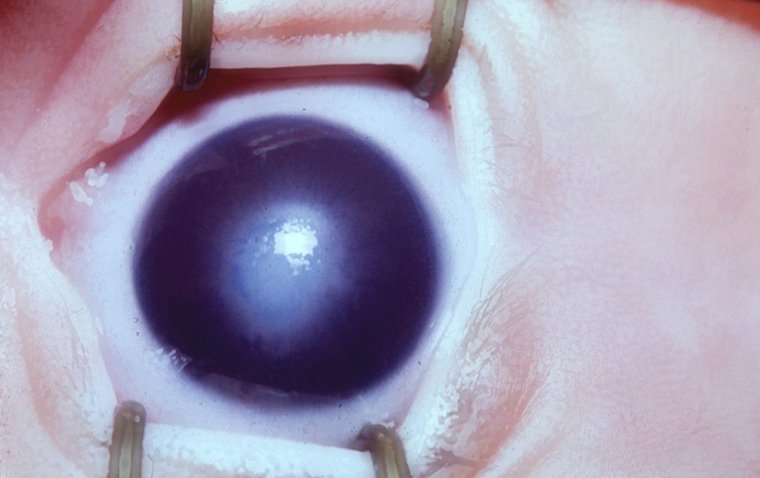
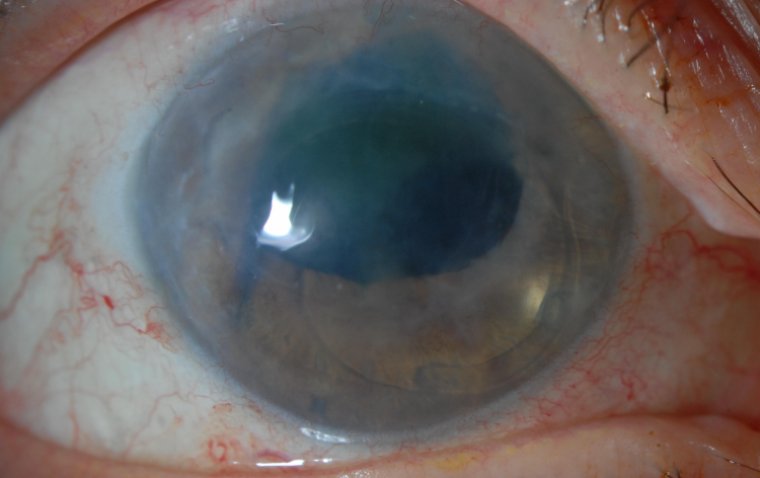
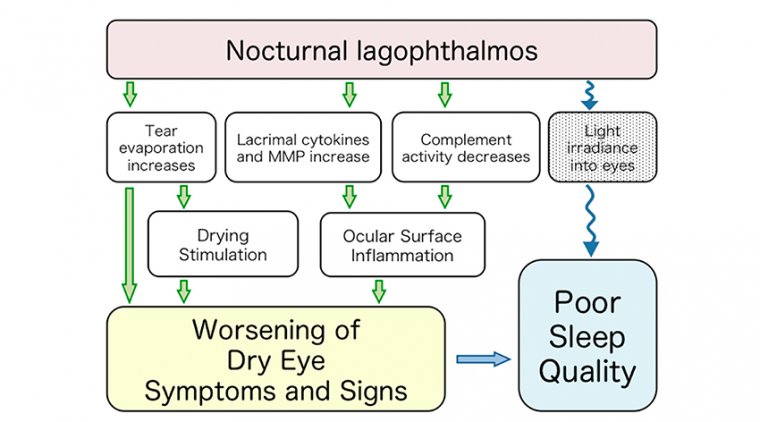
Nocturnal lagophthalmos is the inability to close the eyelids while sleeping. This can result in a range of conditions from mild epithelial changes to severe exposure ulcers (Katz and Kaufman, 1977).
Lagophthalmos is associated with exposure keratopathy, poor sleep, and persistent exposure-related symptoms.
There are a variety of causes of lagophthalmos, grouped as proptosis/eye exposure etiologies and palpebral insufficiency etiologies.
Although obvious lagophthalmos is usually detected, it is sometimes difficult to recognize obscure lagophthalmos, due either to eyelash obstruction or overhang of the upper lid anterior and inferior to the most superior portion of the lower lid in a closed position.
Although obvious lagophthalmos is usually detected, it is sometimes difficult to recognize obscure lagophthalmos, due either to eyelash obstruction or overhang of the upper lid anterior and inferior to the most superior portion of the lower lid in a closed position.
A diagnosis can usually be made with a focused history and slit lamp examination. Treatment is multipronged and may include minor procedures or ocular surgery to correct the lid malposition; natural, topical or oral agents; and punctal plugs to manage ocular surface effects.
Correct and timely diagnosis allows greater opportunity for relief of patient suffering and prevention of severe ocular surface pathology, as well as educated planning for future ocular surgical procedures.
While severe cases can usually be readily diagnosed, we may find it challenging to diagnose the more subtle cases, which can masquerade as dry eye disease.
Challenges with Diagnosing Mild Cases
Unless patients have been told by others, quite often they may suffer from nocturnal lagophthalmos and not be aware of it.
Subtle cases are not easily identified in our exam lane either, because many of these patients can have normal voluntary lid closure during evaluation (Tsai et al, 2009).
In addition, symptoms typically are not terribly helpful. When a patient presents with symptoms of foreign body sensation, hyperemia, and reduced acuity, practitioners are not likely to routinely jump to a diagnosis of lagophthalmos.
In reality, these are symptoms of almost every dry eye patient. Clinically, we can also encounter challenges.
We can identify lagophthalmos from inferior superficial punctate keratitis; but, if patients have only a mild case and their appointment time is late afternoon or evening, those corneal finding may no longer be present.
To accurately identify these patients, practitioners need to do more. When you have a suspicion of nocturnal lagophthalmos that a pacurs at night, some of the best strategies would be implemented at that time.
Addressing the environment in which patients sleep can be helpful, such as using a humidifier. Taping the eyelids closed at night or using commercially available eyelid weights can go a long way in addressing exposure keratitis secondary to lagophthalmos. Both options should be done under a practitioner’s supervision.
While both artificial tears and ointment assist with lubricating the ocular surface, ointments may prove to be more effective, especially when used in conjunction with eyelid taping or with eyelid weights.
Practitioners definitely have options to offer to patients who have nocturnal lagophthalmos, but the key is identifying the problem. As always, an effective case history in connection with a problem-focused exam can help uncover those subtle diagnoses.
Start by asking the right questions. Ask patients: Do you notice a substantial difference in symptoms in the morning as opposed to in the evening? Are there differences between the days that you wear contact lenses and the days that you do not?
Can you come in for a morning appointment? Practitioners can also try to simulate sleeping in the office by asking patients to gently close their eyes. A slit lamp or transilluminator evaluation of the intrapalpebral area will be able to help determine whether lagophthalmos is present.
Treatment Options
Once we determine that a patients has lagophthalmos, there are a few options for contact lens patients. Because the condition occurs at night, some of the best strategies would be implemented at that time.
Addressing the environment in which patients sleep can be helpful, such as using a humidifier. Taping the eyelids closed at night or using commercially available eyelid weights can go a long way in addressing exposure keratitis secondary to lagophthalmos.
Both options should be done under a practitioner’s supervision. While both artificial tears and ointment assist with lubricating the ocular surface, ointments may prove to be more effective, especially when used in conjunction with eyelid taping or with eyelid weights.
Practitioners definitely have options to offer to patients who have nocturnal lagophthalmos, but the key is identifying the problem. As always, an effective case history in connection with a problem-focused exam can help uncover those subtle diagnoses.
(1).jpg)