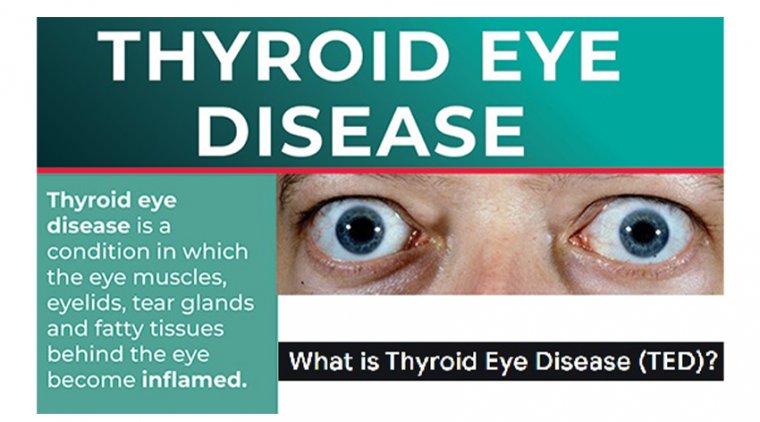
Thyroid Eye Disease (TED)
TED is an autoimmune disease in which the eye muscles and fatty tissue behind the eye become inflamed. This inflammation can push the eyes forward (“staring” or “bulging”) or cause the eyes and eyelids to become red and swollen.
In some individuals, the inflammation may involve the eye muscles, causing the eyes to become out of line, leading to double vision. In rare cases, TED can cause blindness from pressure on the nerve in the back of the eye or ulcers that form on the front of the eye (cornea).
TED is an autoimmune disease, meaning that the inflammation and scarring are caused by an attack from the body’s immune system.
TED is primarily associated with an over-active thyroid gland due to Graves’ disease, although it can rarely occur in patients with an under-active or normally functioning thyroid gland.
About a quarter of patients with Graves’ disease develop TED before, during or after the diagnosis of a thyroid disorder. TED is also known as Graves’ orbitopathy (GO) or Graves’ eye disease (GED). Smokers are two to eight times more likely to develop TED.
Thyroid eye disease (TED) is vision-threatening, making its identification all the more important, according to Gary Lelli, MD, vice chair of ophthalmology at Weill Cornell Medical College in New York, New York.
Although this association is recognized, TED and Graves disease are 2 separate entities. “The TED component,” Lelli said, “can occur in up to 50% of patients with Graves disease, but also in hypothyroid and normal thyroid levels.”
In addition, TED occurs much more often in women—that is, as much as 5 times more often—and more so in the fourth decade of life.
A second peak can occur in older patients in their sixth decade of life. Smokers are also much more likely to develop TED and have a longer period of inflammation from TED as well as a more severe disease course.
The inflammation that develops in TED around the eye and eye socket can cause progressive changes, resulting in functional vision disorders, patient discomfort, and changes in patient appearance over relatively short periods of weeks to months, Lelli explained.
A menu of symptoms accompanies TED, such as severe dry eye, ocular redness and irritation, ocular bulging, eyelid retraction, and blurry vision. The characteristic inflammation associated with TED can impact the ocular muscles, resulting in diplopia and a detrimental effect on daily activities, such as reading and driving.
In the most severe cases, inflammation can cause compression of the optic nerve, resulting in visual loss. This most severe result can occur in approximately 2% to 5% of patients. Inflammation also can affect the normal fat behind the eyes and cause hypertrophy.
This scenario is involved with ocular bulging. Swelling that is related to the fat hypertrophy can be apparent in the lower and upper eyelids. The TED team Lelli emphasized that an evaluation conducted by the appropriate specialist is the most important factor in diagnosing and managing this patient population.
A history of any thyroid imbalance, especially a history of Graves disease, should signal an evaluation by an oculoplastic surgeon or a neuro-ophthalmologist.
Early treatment and putting a team of clinicians in place that includes an oculoplastic surgeon, a neuro-ophthalmologist, an endocrinologist, a strabismus specialist, and in some cases a psychiatrist or psychologist to assist with the emotional problems that accompany drastic changes in appearance, are most beneficial, Lelli advised.
Early treatment steps Because TED has a variety of presentations, the first step is categorization of the patient regarding the disease stage, degree of inflammation, specific ocular symptoms, and presence of any aesthetic changes.
Establishing this base of information then leads to determination of the appropriate treatment, Lelli said. Treatment ranges from addressing symptoms with dry eye drops, for example; antioxidants to decrease inflammation; oral or intravenous anti-inflammatories; and surgery to relieve ocular bulging, eyelid retraction, and diplopia.
“There is a wide range of treatment options, but they hinge on assembling the right team of clinicians who can properly diagnose and categorize patients,” he said. Although there currently is no cure for TED, Lelli reported that more targeted treatments are in the offing.
“A lot of the disease and orbital inflammation occur at the level of the orbital fibroblasts, receptors that are targeted by the autoimmune process to create inflammation. We have ways to target those and more research is being done.
We can make the disease substantially more tolerable for patients,” he said. TED awareness In 2021, the second TED Awareness Week was held in November, focusing on the dissemination of information about TED to patients and clinicians alike.
A small percentage of patients with TED (ie, 5%-10%) have hypothyroidism, and a baseline examination is warranted.
The goal is to provide information to patients, ophthalmologists, and other eye care clinicians to raise their awareness of TED signs and symptoms in patients who have a history of thyroid disease, Lelli explained.
A referral to an oculoplastic surgeon or neuro-ophthalmologist may catch the disease early in the process. Lelli advises that clinicians who have patients with Graves disease or a thyroid condition should look for the signs and symptoms of TED.
If a clinician is suspicious that a patient may have TED, speed is of the essence. An early evaluation by specialists can help get the patients on the right treatment path if warranted.
Lelli suggested the website, focusonted.com, to provide useful information about the disease for patients and doctors as well as specialists listed by ZIP code.
(1).jpg)