Demodex Blepharitis: Symptoms, Causes, and Effective Treatment Options
Demodex blepharitis is an inflammatory condition of the eyelids, caused by an overpopulation of Demodex mites, that affects millions worldwide, including an estimated 25 million Americans. This condition highlights the critical intersection between common parasitic infestations and ocular health, underscoring the importance of timely and effective management strategies.
What Are Demodex Mites?
Demodex mites, tiny arachnids residing in the hair follicles and sebaceous glands of most humans, are generally harmless but can cause significant issues when their population on the eyelids becomes excessive. This section explores the biology and behavior of Demodex mites, illustrating how their presence is a normal part of the human skin's ecosystem but can lead to inflammatory conditions like blepharitis when their numbers increase beyond a certain threshold. The relationship between Demodex mites and humans is usually symbiotic, yet it can swiftly turn problematic, triggering inflammation and contributing to the development of blepharitis.
The contribution of Demodex mites to the pathogenesis of blepharitis is complex and multifaceted. These mites not only cause mechanical damage to the eyelid but also serve as vectors for bacterial infections, further exacerbating inflammatory responses.

Causes and Risk Factors of Demodex Blepharitis
The etiology of Demodex blepharitis is influenced by a combination of factors, including age, underlying health conditions such as rosacea and diabetes, and possibly genetic predisposition. Demodex blepharitis is primarily caused by the overpopulation of Demodex mites on the eyelids and lashes, specifically two types of mites: Demodex folliculorum and Demodex brevis. These mites are part of the normal skin microbiome and are usually harmless in small numbers. However, under certain conditions, their numbers can increase significantly, leading to the symptoms of blepharitis.
Several factors contribute to the proliferation of Demodex mites, leading to blepharitis:
• Age: The prevalence of Demodex mites increases with age, making older adults more susceptible to Demodex blepharitis. This is possibly due to changes in skin texture, reduced immune surveillance, or alterations in sebum composition that make the skin more hospitable to mites.
• Compromised Immune System: Individuals with weakened immune systems, whether due to medical conditions, such as diabetes or HIV/AIDS, or the use of immunosuppressive medications, are at a higher risk. A reduced immune response may not adequately control the mite population.
• Skin Conditions: People with certain skin conditions, particularly rosacea and seborrheic dermatitis, are more likely to develop Demodex blepharitis. These conditions may alter the skin's environment, making it more conducive for mite survival and reproduction.
• Poor Eyelid Hygiene: Inadequate eyelid hygiene can provide a favorable environment for Demodex proliferation. Makeup residue, skin oils, and dead skin cells can accumulate, feeding the mites and encouraging their growth.
• Contact Lens Wear: Wearing contact lenses, especially if not cleaned properly, can increase the risk of Demodex blepharitis. Contact lenses can trap bacteria and create a protective niche for mites close to the eyelid surface.
• Environmental Factors: Humid environments may also support the growth of Demodex populations by creating a more suitable microclimate for mites on the skin surface.Demodex blepharitis's prevalence underscores the need for targeted awareness and education efforts, aiming to inform both the public and healthcare professionals about the condition's risk factors and early signs. Such knowledge is crucial for early detection and intervention, potentially mitigating the disease's impact on patients' lives.
Symptoms and Diagnosis
Symptoms of Demodex blepharitis are multifaceted and can significantly impact the quality of life for those affected. The condition is characterized by chronic inflammation of the eyelid margins, leading to a variety of ocular symptoms that can range from mild to severe. The hallmark symptoms include persistent eyelid redness and swelling, accompanied by an itchy or burning sensation. Patients often report feeling like there is something gritty or foreign in their eyes, a sensation that can be particularly bothersome and persistent.
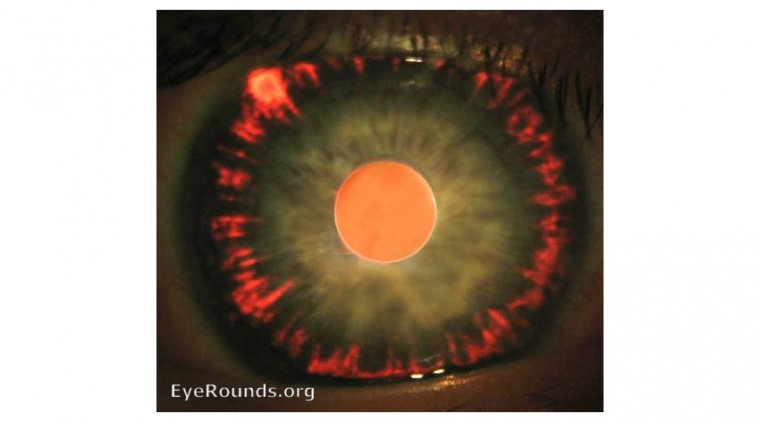
Another distinctive symptom of Demodex blepharitis is the presence of collarettes, which are cylindrical dandruff-like scales that cling to the base of the eyelashes. These are not seen in other forms of blepharitis and are considered pathognomonic for Demodex infestation. The eyelashes may also appear crusted, and in more severe cases, patients may experience eyelash loss or misdirection, a condition known as trichiasis.
In addition to these local symptoms, individuals with Demodex blepharitis may also experience blurred vision due to the disturbance of the tear film and secondary dry eye syndrome. This can result from the inflammation extending to the ocular surface, affecting the stability of the tear film and leading to visual fluctuations.
The diagnosis of Demodex blepharitis involves a combination of clinical examination and specific diagnostic techniques. A key diagnostic method is the examination of eyelash samples under a microscope. This allows for the direct visualization of Demodex mites attached to the eyelashes or embedded within the cylindrical dandruff, providing a definitive diagnosis. The process typically involves epilating a few eyelashes and examining them for the presence of mites.
Additionally, healthcare professionals may use slit-lamp biomicroscopy to closely inspect the eyelids and lashes for signs of inflammation, collarettes, and other indicative features of Demodex blepharitis. This examination can reveal the characteristic cylindrical dandruff at the base of the eyelashes, even before the mites are directly observed.
In cases where the diagnosis is uncertain, or to confirm the extent of the infestation, more advanced diagnostic tools, such as in vivo confocal microscopy, may be employed. This technique provides high-resolution images of the eyelid margin, hair follicles, and meibomian glands, allowing for detailed observation of mite activity and the associated inflammatory response.
Given the chronic nature of Demodex blepharitis and its potential to mimic or coexist with other ocular conditions, a thorough and comprehensive diagnostic approach is essential for accurate diagnosis and effective management.
Treatment Options
Tea Tree Oil Applications
Tea tree oil (TTO) stands out as a primary treatment for Demodex blepharitis, thanks to its acaricidal capabilities that effectively diminish Demodex mite populations. It is available in various concentrations and formulations, including commercially prepared solutions and wipes specifically designed for ocular application. To avoid irritation to the sensitive eyelid area and ocular surface, it is recommended to commence treatment with lower concentrations of TTO, gradually adjusting based on tolerance and effectiveness.
Enhanced Eyelid Hygiene
A cornerstone of managing Demodex blepharitis is maintaining rigorous eyelid hygiene. This involves the daily cleansing of eyelids and lashes with gentle, ocular-specific cleansers that do not irritate the eyes. Regular cleaning helps eliminate mite-supportive biofilm, excess oils, and debris, thereby reducing irritation and mitigating inflammation.
Antibiotics for Inflammation and Infection
In cases where Demodex blepharitis leads to significant inflammation or secondary bacterial infection, antibiotics may be prescribed. Medications such as doxycycline are favored for their anti-inflammatory properties in addition to their antibacterial action. These can be administered topically or orally to address both the symptoms and underlying causes of inflammation.
Emerging Medications and Treatments
The treatment landscape for Demodex blepharitis is evolving with the introduction of new medications targeting Demodex mites. Ivermectin, an anti-parasitic agent, has shown efficacy in reducing mite density when used as a topical cream or oral medication. Another innovative approach is the Tarsus Pharmaceuticals' XDEMVY (lotilaner ophthalmic solution) 0.25% which recently became the first and only FDA-approved treatment for the Demodex Blepharitis.
Addressing Associated Conditions
Treatment plans for Demodex blepharitis often include strategies to manage related conditions, such as dry eye syndrome. Artificial tears and other interventions can be employed to enhance tear film stability and improve the overall health of the ocular surface.
Prevention and Management
Preventing and managing Demodex blepharitis involves a combination of rigorous eyelid hygiene and lifestyle modifications. Regular cleaning of the eyelid margin with gentle, non-irritating cleansers or commercially available eyelid wipes designed to combat Demodex mites is crucial. This not only helps reduce the mite population but also removes debris and secretions that can exacerbate the condition. Additionally, avoiding eye makeup and facial products that can irritate the eyelids is recommended.
Implementing changes such as washing pillowcases and towels in hot water can also minimize re-infestation. For individuals diagnosed with Demodex blepharitis, consistent adherence to the treatment regimen prescribed by an eye care professional is essential for managing symptoms and preventing flare-ups. This may include the use of tea tree oil products, medicated cleansers, and, in some cases, prescription medications to control mite populations and address inflammation.
Complications and Comorbidities
The complications associated with Demodex blepharitis can progress due to several factors inherent to the condition and its management.
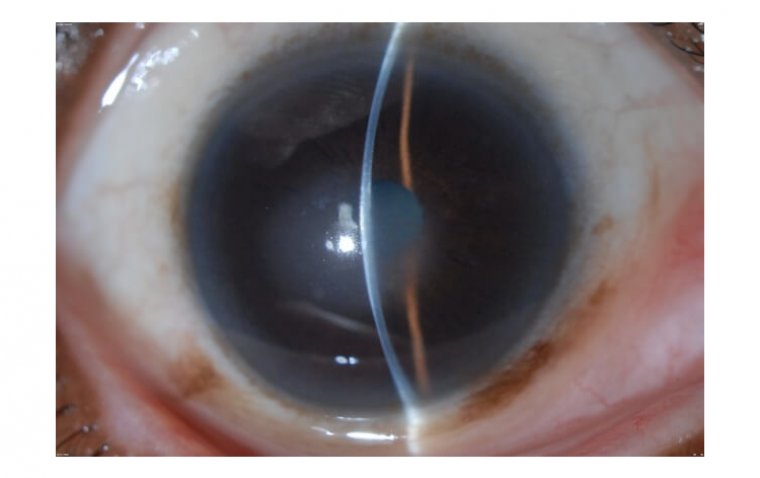
• Keratitis may develop when inflammation from the eyelid spreads to the cornea, often exacerbated by the mechanical irritation of rubbing the eyes or by the presence of mites and bacteria infiltrating the corneal surface.
• Chalazia form as a result of the blockage of the Meibomian glands due to inflammation and mite debris, leading to the retention of glandular secretions and cyst formation.
• Styes (Hordeolum) occur when bacterial infections take advantage of the compromised eyelid environment, infecting the eyelash follicles or Meibomian glands.
• Ocular Rosacea's comorbidity with Demodex blepharitis may be due to shared inflammatory pathways and triggers, causing both conditions to exacerbate each other.
• Dry Eye Syndrome can be a direct result of the disruption of the eyelid's oil glands by Demodex mites, affecting the tear film's stability and leading to increased tear evaporation.
• Corneal Ulcers may form from advanced keratitis, where persistent inflammation and infection damage the corneal surface, creating ulcers.
• Conjunctivitis can arise from the spread of inflammation from the eyelids to the conjunctiva, further irritated by mites or secondary infections.
• Eyelash Abnormalities, such as madarosis, trichiasis, or abnormal growth, occur due to the direct damage to hair follicles by the mites or as a result of chronic inflammation.
• Eyelid Skin Changes like hyperpigmentation, thickening, or scarring are responses to prolonged inflammation and irritation caused by the mites and their waste products.
• Secondary Bacterial Infections can become more likely as the skin's normal barrier is compromised by the ongoing inflammation and disruption caused by Demodex infestations, allowing bacteria to invade more easily.
Understanding related conditions, such as blepharoconjunctivitis and its causes and treatment, can also provide valuable insights into managing ocular health effectively.
Recent Research and Developments
Recent research and developments in the field of Demodex blepharitis have been focused on understanding the condition's pathophysiology, improving diagnostic methods, and exploring new treatment options. Studies have increasingly highlighted the significance of Demodex mites in various ocular surface diseases, emphasizing the need for accurate diagnosis and effective management strategies.
One of the notable advancements is the investigation into the efficacy of various concentrations of tea tree oil (TTO) and its components for treating Demodex blepharitis. Research has demonstrated that TTO can effectively reduce Demodex mite populations, with ongoing studies aiming to optimize formulations to maximize efficacy while minimizing potential irritation to the ocular surface.
In terms of diagnostics, advancements in imaging technologies such as in vivo confocal microscopy have improved the ability of clinicians to visualize Demodex mites on the eyelids and ocular surface. This technology allows for a more accurate diagnosis and aids in monitoring the response to treatment.
Emerging treatments include the development of new medications specifically targeting the Demodex mites. For example, the use of ivermectin, both topically and orally, has shown promise in reducing mite populations and alleviating symptoms of blepharitis. Another significant development is the first and only FDA-approved Tarsus Pharmaceuticals' XDEMVY (lotilaner ophthalmic solution) 0.25%.
For those interested in the latest advancements in ophthalmic treatments, reviewing the top 12 ophthalmic drugs that received FDA approval in 2023 can provide a broader perspective on the evolving treatment landscape.
Conclusion
Recognizing and addressing Demodex blepharitis is essential for maintaining eye health and ensuring the well-being of those affected. With continued research, improved treatments, and increased awareness, individuals can manage this condition more effectively, leading to better outcomes and quality of life. Seeking professional diagnosis and adhering to prescribed treatment regimens are key to controlling this challenging yet manageable condition.
Reference:
(1).jpg)