Retinal Vasculitis: A Closer Look at Inflammatory Eye Diseases
What Is Retinal Vasculitis?
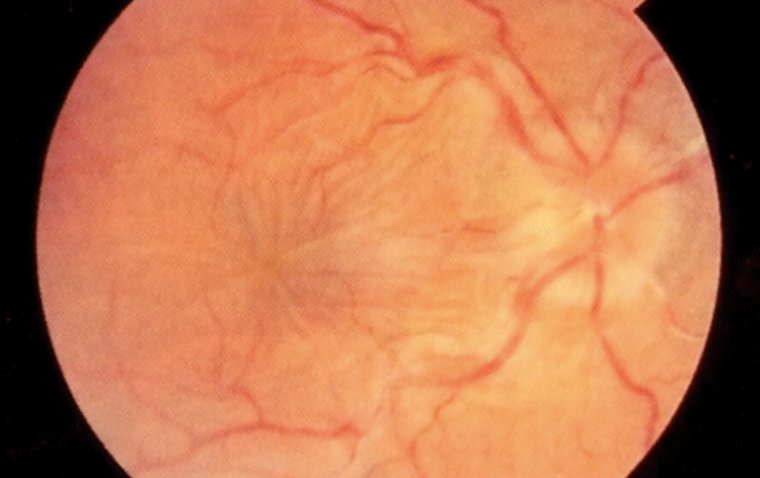
Retinal vasculitis is an inflammatory condition affecting the blood vessels of the retina. This inflammation can disrupt the normal blood flow, leading to complications that may compromise visual function.
Pathophysiology
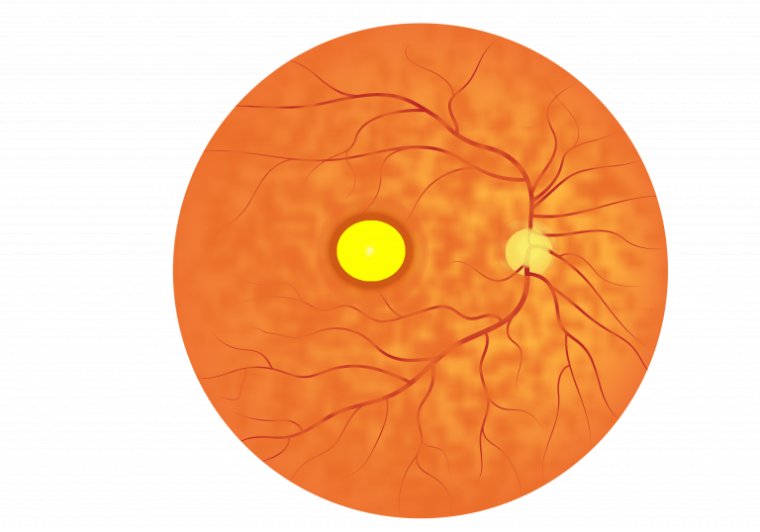
In retinal vasculitis, inflammatory cells such as neutrophils, macrophages, and lymphocytes infiltrate the vascular endothelium of the retinal blood vessels. This leads to a cascade of inflammatory responses, including the production of cytokines, that induce vessel wall inflammation. As a result, the permeability of the blood-retinal barrier is compromised, which can lead to macular edema and hemorrhage.
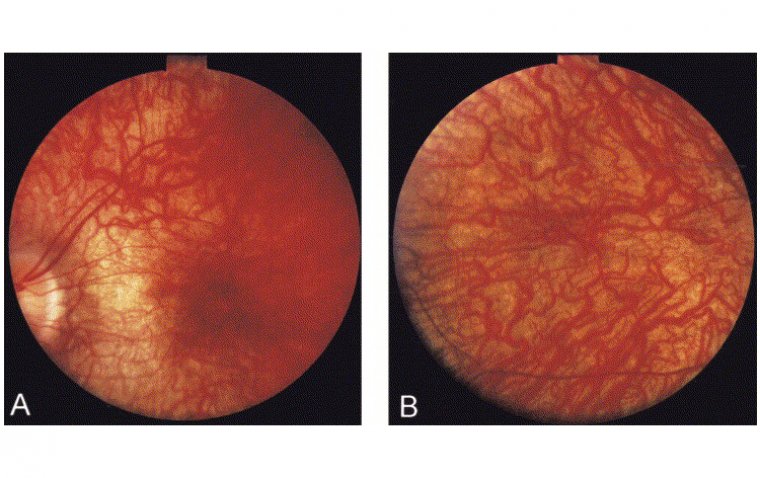
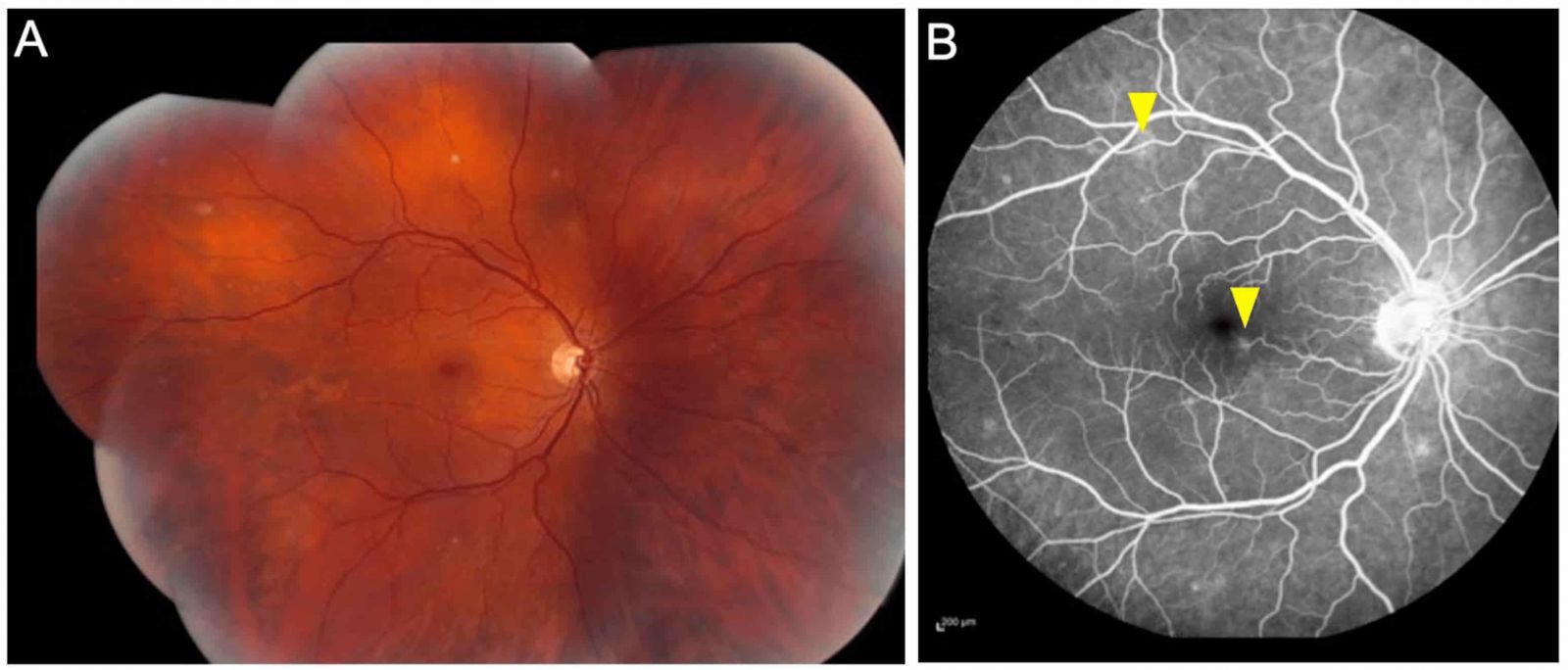
The clinical manifestations can vary widely but generally include blurry vision, floaters, and sometimes a decrease in visual field. In severe cases, complications such as retinal ischemia, neovascularization, and even retinal detachment may occur. Diagnosis is generally made through fundus examination and imaging studies like fluorescein angiography and optical coherence tomography (OCT).
Causes and Mechanisms Leading to Inflammation
● Autoimmune Conditions
Conditions like Behcet's disease, systemic lupus erythematosus, and sarcoidosis can lead to retinal vasculitis. In these cases, autoantibodies target vascular endothelial cells, leading to inflammation.
● Infectious Causes
Infections like tuberculosis, syphilis, and toxoplasmosis can cause a localized infection in the retinal vessels. The body’s immune response to fight off the infection inadvertently damages the retinal blood vessels.
● Hypersensitivity Reactions
Drug-induced retinal vasculitis is also a possibility. Here, an allergic reaction to certain medications can induce an inflammatory cascade that affects retinal vasculature.
● Idiopathic
In a significant number of cases, the cause of retinal vasculitis remains unknown. These are usually categorized as "idiopathic" and may require long-term immunosuppressive therapy.
Mechanisms
1. Inflammatory Cascade: Activation of immune cells leads to the release of inflammatory mediators like cytokines and chemokines.
2. Endothelial Dysfunction: Inflammation directly impairs the vascular endothelium, increasing its permeability and leading to fluid leakage into the retina.
3. Ischemia: Severe inflammation can compromise blood flow, leading to ischemic areas that trigger further complications like neovascularization.
4. Thrombus Formation: Inflammation can also induce a pro-thrombotic state, which could lead to the formation of a thrombus, further worsening blood flow.
Retinal Vasculitis Causes
1. Genetic Predisposition
Though not fully understood, a genetic predisposition can make individuals more susceptible to autoimmune diseases that can, in turn, lead to retinal vasculitis.
2. Environmental Factors
Exposure to certain infectious agents or environmental toxins may serve as triggers in genetically predisposed individuals.
3. Autoimmune Diseases
● Behcet's Disease: One of the most common causes, especially in Middle Eastern populations. Inflammation typically involves both arteries and veins and can be quite severe.
● Systemic Lupus Erythematosus (SLE): Vasculitis is a common feature in SLE and can extend to the retinal vasculature.
● Sarcoidosis: Known for its non-caseating granulomas, sarcoidosis can also involve the retina, leading to vasculitis.
● Rheumatoid Arthritis: Though more commonly affecting the joints, RA can also cause inflammation of the retinal vessels.
● Multiple Sclerosis: Rarely, MS can be associated with retinal vasculitis, mainly as an extension of optic neuritis.
● Inflammatory Bowel Diseases: Conditions like Crohn’s disease and ulcerative colitis have been associated with retinal vasculitis, although rarely.
4. Infections
● Tuberculosis: A chronic infection that can involve almost any organ system, including the eyes. Retinal vasculitis can be a manifestation of ocular TB.
● Syphilis: Known as the 'great imitator,' syphilis can cause a wide range of ocular manifestations, including retinal vasculitis.
● Toxoplasmosis: This protozoan infection can lead to localized inflammation of the retina and surrounding vessels.
● Herpes Viruses: Both HSV and CMV can cause retinitis and secondary retinal vasculitis, particularly in immunocompromised individuals.
● HIV: Patients with late-stage HIV can develop retinal vasculitis, usually secondary to opportunistic infections.
Systemic Associations
● Hypercoagulable States: Conditions like antiphospholipid syndrome can cause a pro-thrombotic environment, increasing the risk of vessel occlusion and subsequent vasculitis.
● Drug Reactions: Some medications, such as bisphosphonates and interferons, have been implicated in drug-induced retinal vasculitis.
● Idiopathic: Despite extensive investigation, some cases remain idiopathic. These might require empirical treatment with immunosuppressive drugs.
Signs and Symptoms of Retinal Vasculitis
Visual Changes
Blurred Vision: One of the earliest and most common symptoms, often described as looking through a "fog" or "haze."
Floaters: Patients may notice dark spots or "cobwebs" floating in their field of vision, particularly against bright backgrounds.
Reduced Visual Acuity: A decline in sharpness of vision can be gradual or sudden, affecting reading and other activities that require detailed vision.
Photopsia: Flashes of light or shimmering can occur and are often more noticeable in dim light conditions.
Peripheral Vision Loss: Initially, patients may report difficulty in seeing objects in their peripheral vision, which may progress to involve the central vision in advanced cases.
Color Vision Changes: Reduced ability to perceive colors, especially blues and yellows, may be noted.
Physical Discomfort
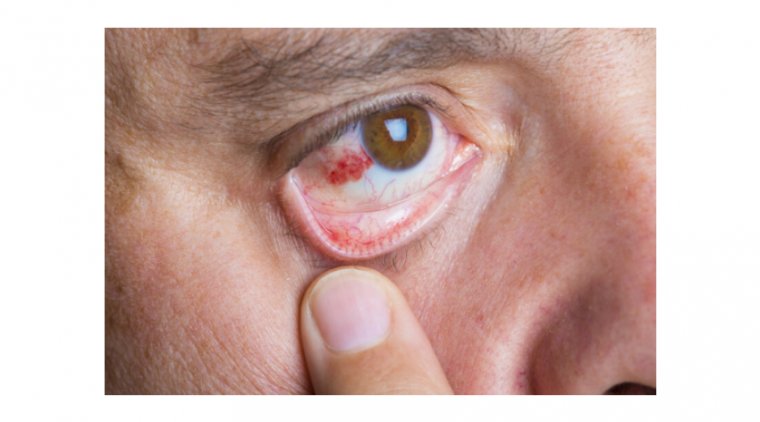
Red Eye: Although not as common, inflammation can extend to other parts of the eye, causing visible redness.
Pain: Generally uncommon but can occur, usually mild to moderate in intensity, worsening with eye movement in some cases.
Tearing: Excessive watering of the eyes may occur but is generally non-specific.
Sensitivity to Light: Known as photophobia, this is a less common symptom but can cause considerable discomfort.
The impact of retinal vasculitis on vision can be significant and life-altering. Persistent inflammation, if left untreated, can lead to permanent vision loss or even complete blindness. This reduced visual acuity can profoundly affect a patient's ability to perform daily activities, including driving, reading, and recognizing faces. As such, the condition can have a severe negative influence on the patient's overall quality of life. Therefore, early detection and prompt treatment are crucial to prevent long-term complications and mitigate the impact on vision.
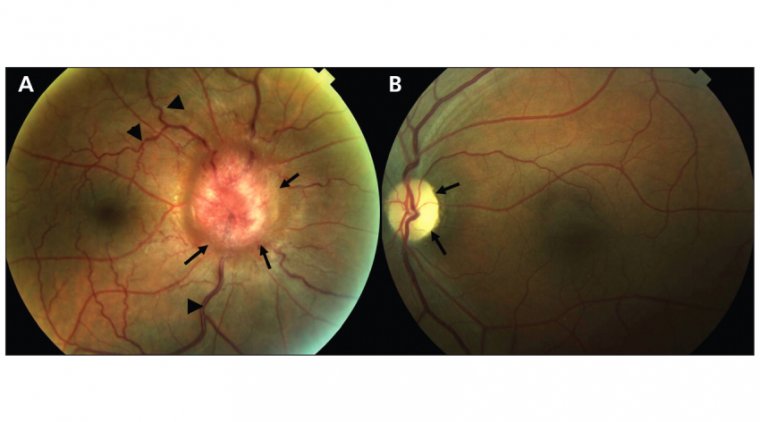
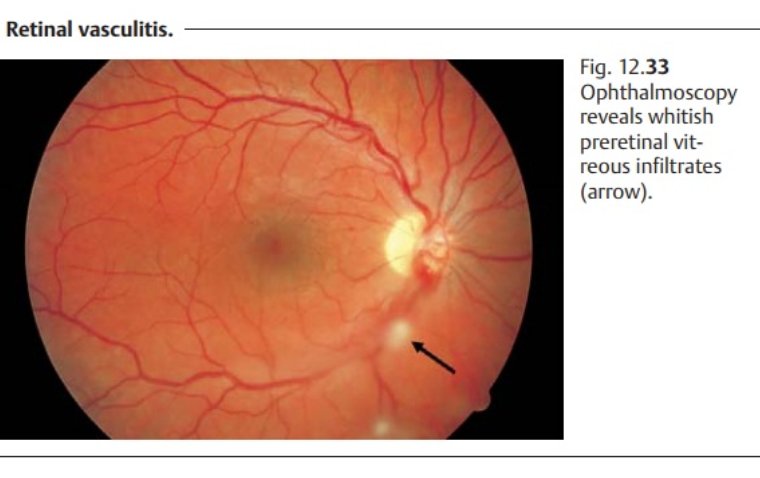
How to Diagnose and Assess Retinal Vasculitis
The diagnosis and assessment of retinal vasculitis are multi-faceted and require a comprehensive approach by eye care professionals. Initially, a thorough ocular examination is conducted, which may include visual acuity tests, slit-lamp biomicroscopy, and ophthalmoscopy to assess the retina and its blood vessels. Further evaluation often involves advanced imaging techniques such as fluorescein angiography and optical coherence tomography (OCT) to get a detailed view of the retinal layers and to identify any vascular changes or abnormalities. Additionally, laboratory tests may be ordered to rule out systemic conditions that could be triggering the inflammation. These could include blood tests for markers of inflammation, as well as tests for underlying autoimmune conditions or infections. Together, these diagnostic measures provide a comprehensive assessment of the condition, facilitating early and targeted intervention to prevent vision loss.
Treatment Options for Retinal Vasculitis
Treatment options for retinal vasculitis are designed to address both the symptoms and the underlying causes of the condition. Medication is often the first line of therapy and can include corticosteroids to rapidly reduce inflammation. However, prolonged use of steroids may lead to other ocular complications like glaucoma or cataract formation, so their use is typically carefully managed. Immunosuppressive medications such as cyclosporine, azathioprine, or methotrexate may also be employed to control chronic inflammation and are often used in conjunction with corticosteroids to achieve a synergistic effect.
Biologic agents like anti-TNF medications may also be considered in cases that do not respond to traditional immunosuppressive therapies. These options are particularly useful in treating retinal vasculitis associated with certain systemic conditions like Behçet's disease or sarcoidosis.
Lifestyle adjustments can also play a role in managing retinal vasculitis. Patients may be advised to quit smoking and to control other systemic conditions like diabetes and hypertension, as these can exacerbate ocular inflammation. Nutritional supplements rich in antioxidants may also be recommended, although the evidence supporting their effectiveness is still limited.
For more severe or unresponsive cases, surgical interventions like vitrectomy may be considered to remove the vitreous gel, which may contain inflammatory debris that could further damage the retina. The treatment plan is generally tailored to the individual patient's needs and the underlying cause of the retinal vasculitis, and it typically involves regular follow-ups to monitor therapeutic effectiveness and to adjust treatment as necessary.
Complications and Prognosis
Untreated or severe retinal vasculitis can lead to a host of complications, many of which can have a lasting impact on vision and overall ocular health. Among the most concerning complications are retinal detachment, macular edema, and neovascularization, which may ultimately result in severe vision loss or even blindness. Additionally, persistent inflammation can increase the risk for secondary glaucoma, cataract formation, and uveitis, further exacerbating vision problems and complicating the overall treatment plan. In severe cases, retinal vasculitis may also cause irreversible damage to the optic nerve, with catastrophic consequences for vision.
The prognosis for retinal vasculitis largely hinges on early diagnosis and timely intervention. Aggressive treatment at the onset can often arrest the inflammation and mitigate the risk of these severe complications. Moreover, if retinal vasculitis is a manifestation of an underlying systemic condition, treating the root cause is paramount for long-term ocular health. Regular follow-ups with eye care professionals for monitoring and possible treatment adjustments are critical.
How to Prevent Retinal Vasculitis
● Regular Eye Check-Ups: Schedule regular appointments with an eye care professional for a comprehensive eye exam to catch any early signs of inflammation or other abnormalities.
● Manage Underlying Conditions: If you have systemic conditions like lupus, sarcoidosis, or multiple sclerosis that could potentially cause retinal vasculitis, work closely with your healthcare team to manage these diseases effectively.
● Follow Treatment Plans: Adherence to prescribed medication and treatment regimens for existing eye conditions or systemic diseases is crucial to prevent complications like retinal vasculitis.
● Avoid Smoking: Smoking is a risk factor for numerous eye conditions and can exacerbate inflammation. Quitting can help promote overall eye health.
● Nutritional Support: A diet rich in antioxidants, omega-3 fatty acids, and vitamins like A and C can support eye health.
● Good Hygiene: Practicing good eye hygiene, such as not touching the eyes with dirty hands and properly cleaning contact lenses, can help prevent infections that may trigger retinal vasculitis.
● Be Aware of Symptoms: Familiarize yourself with the early symptoms of retinal vasculitis, such as blurry vision, floaters, or eye pain. Seek immediate medical attention if you experience these.
● Regular Exercise: Exercise can improve blood circulation, including in the retinal vessels, potentially reducing the risk of inflammatory conditions.
● Sun Protection: Wearing sunglasses with UV protection can protect the eyes from harmful rays, reducing the risk of inflammatory conditions.
Summary
In summary, retinal vasculitis is an inflammatory condition affecting the blood vessels of the retina, with potential causes ranging from autoimmune diseases to systemic infections. Its symptoms often include vision disturbances and ocular discomfort, requiring prompt diagnostic tests like ocular examinations, imaging, and laboratory assessments for accurate diagnosis. The treatment approach usually involves medications and immunosuppressive therapies tailored to the underlying cause, and lifestyle adjustments may also be recommended.
Given the serious complications that can arise from untreated or severe cases, such as permanent vision loss, the importance of early detection and timely treatment cannot be overstated. Regular eye check-ups, proper management of systemic conditions, and overall health maintenance can aid in early identification and better prognosis. Therefore, a proactive approach to eye care, including awareness of the symptoms and risk factors, is crucial for optimal eye health.
(1).jpg)