Corneal Neovascularization: Causes and Emerging Treatments
What is Corneal Neovascularization?
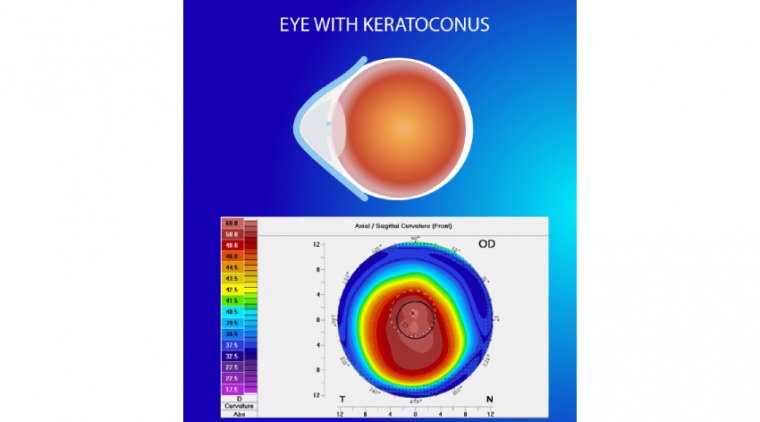
Corneal neovascularization refers to the abnormal growth of blood vessels in the cornea, which is the clear, dome-shaped surface at the front of the eye. The cornea is responsible for protecting the eye and allowing light to enter, ultimately playing a crucial role in clear vision. Under normal circumstances, the cornea remains avascular, meaning it is devoid of blood vessels. This avascularity is essential for maintaining corneal transparency and optimal visual acuity.
However, in some cases, blood vessels from the limbus (the border between the cornea and the sclera) can begin to grow into the cornea, leading to corneal neovascularization. This growth may occur in response to various factors such as inflammation, infection, trauma, or hypoxia (a lack of oxygen). The presence of blood vessels in the cornea can compromise its transparency, potentially leading to reduced vision and other complications.
The Science of Corneal Neovascularization: How It Affects the Cornea
Corneal neovascularization occurs when the balance between pro-angiogenic (blood vessel-promoting) and anti-angiogenic (blood vessel-inhibiting) factors in the cornea is disrupted, leading to the growth of new blood vessels. The process of blood vessel formation, or angiogenesis, is a complex cascade of events that involves various signaling molecules, growth factors, and cellular interactions.
One of the key players in corneal neovascularization is vascular endothelial growth factor (VEGF), a potent pro-angiogenic factor that stimulates the proliferation and migration of endothelial cells to form new blood vessels. In response to injury, inflammation, or hypoxia, the levels of VEGF and other pro-angiogenic factors increase, leading to the initiation of angiogenesis.
The presence of blood vessels within the cornea can have several detrimental effects on vision and overall eye health:
1. Loss of corneal transparency: The growth of blood vessels in the cornea can disrupt its organized structure, resulting in a loss of transparency and consequently, reduced visual acuity.
2. Edema and scarring: Neovascularization can compromise the integrity of the corneal epithelium, leading to fluid accumulation (edema) and the development of scar tissue. These changes can further impair vision and may cause discomfort or pain.
3. Increased risk of infection: The formation of new blood vessels can introduce inflammatory cells and other mediators into the cornea, increasing the risk of infections and potentially leading to more severe complications, such as corneal ulcers.
4. Impaired corneal function: The presence of blood vessels in the cornea can interfere with the proper function of the corneal endothelium, which is responsible for maintaining corneal hydration and clarity. This can result in corneal swelling and vision loss.
Understanding the science of corneal neovascularization and its impact on the cornea is crucial for developing effective treatment strategies and managing this condition to minimize its effect on vision and eye health.
Causes of Corneal Neovascularization
Corneal neovascularization can occur due to various factors that disrupt the balance between pro-angiogenic and anti-angiogenic factors in the cornea. Some of the most common causes of corneal neovascularization include:
1. Inflammation: Inflammatory eye conditions, such as keratitis, scleritis, or uveitis, can trigger the release of pro-angiogenic factors, leading to the growth of blood vessels in the cornea.
2. Infection: Bacterial, viral, fungal, or parasitic infections can cause corneal inflammation and damage, stimulating neovascularization. For example, herpes simplex keratitis, a viral infection, is a common cause of corneal neovascularization.
3. Trauma: Mechanical or chemical injuries to the cornea can induce an inflammatory response and stimulate the formation of new blood vessels.
4. Hypoxia: Insufficient oxygen supply to the cornea can result from extended contact lens wear or other conditions that reduce oxygen availability. Hypoxia triggers the production of pro-angiogenic factors, such as VEGF, leading to neovascularization.
5. Corneal transplant rejection: In some cases, the immune system may react to a corneal graft, causing inflammation and promoting neovascularization in the transplanted tissue.
6. Corneal degeneration and dystrophies: Certain corneal disorders, such as pterygium or lipid keratopathy, can cause corneal neovascularization as a result of chronic inflammation or tissue damage.
7. Tumors: Benign or malignant ocular tumors can stimulate the growth of blood vessels in the cornea due to their high metabolic demand or the release of angiogenic factors.
Signs and Symptoms of Corneal Neovascularization
The signs and symptoms of corneal neovascularization can vary depending on the severity and extent of the blood vessel growth, as well as the underlying cause. Some common signs and symptoms associated with corneal neovascularization include:
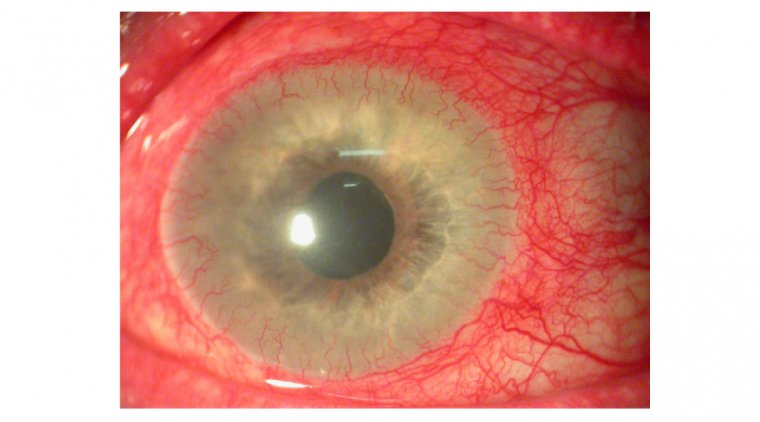
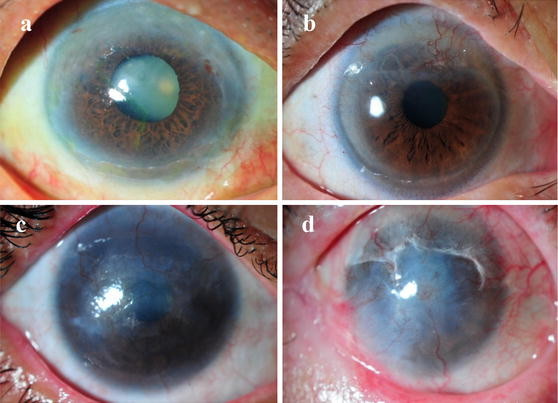
● Visible blood vessels: In some cases, individuals with corneal neovascularization may notice the appearance of new blood vessels in their cornea, especially when the growth is extensive. The vessels may appear as fine red lines or branching patterns.
● Redness: Corneal inflammation, which often accompanies neovascularization, can lead to redness in the affected eye.
● Pain or discomfort: Depending on the underlying cause, corneal neovascularization may be associated with pain, discomfort, or a foreign body sensation in the eye.
● Blurred vision: The presence of blood vessels in the cornea can disrupt its transparency, leading to blurred or reduced vision.
● Sensitivity to light: Corneal inflammation or damage caused by neovascularization may result in increased sensitivity to light, known as photophobia.
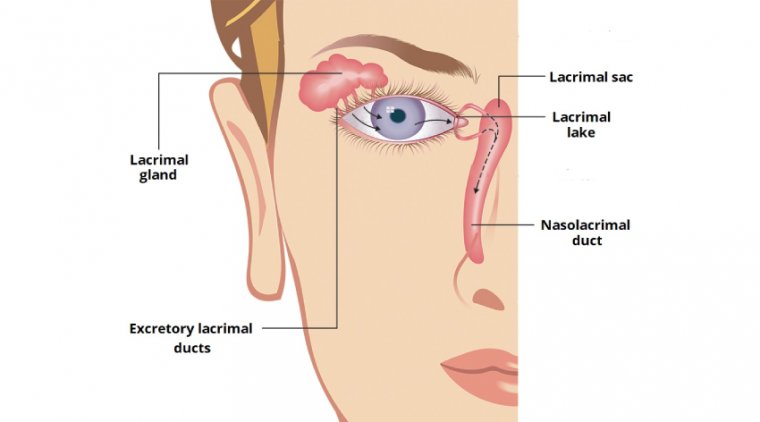
● Tearing: Excessive tearing or eye watering may occur in response to irritation or inflammation in the eye.
● Swelling: In some cases, corneal neovascularization can lead to corneal edema or swelling, which may be visible as a hazy or cloudy appearance in the cornea.
Impaired Vision and Eye Irritation
Corneal neovascularization can have a significant impact on vision and overall eye comfort due to the presence of blood vessels within the cornea and the accompanying inflammation. The effects of corneal neovascularization on vision and eye irritation include:
1. Impaired vision: The growth of blood vessels into the cornea can disrupt its organized structure, resulting in a loss of transparency. This can lead to blurry or hazy vision, making it difficult for individuals to see clearly and affecting their daily activities.
2. Astigmatism: Irregular blood vessel growth within the cornea can alter its shape, resulting in astigmatism. This condition causes light to refract unevenly, leading to distorted or blurred vision.
3. Light sensitivity: Inflammation and irritation associated with corneal neovascularization can cause increased sensitivity to light, known as photophobia. This can make it uncomfortable for individuals to spend time in bright environments or expose their eyes to sunlight.
4. Eye discomfort: The presence of blood vessels in the cornea, along with the underlying causes of neovascularization, can lead to various forms of eye discomfort, such as pain, a foreign body sensation, or a gritty feeling in the eye.
5. Dryness and tearing: Corneal neovascularization can interfere with the normal tear film, causing the eyes to feel dry and irritated. In response to this discomfort, the eyes may produce excessive tears in an attempt to soothe the irritation.
Management of Corneal Neovascularization
Effective management of corneal neovascularization involves addressing the underlying cause, alleviating symptoms, and preserving vision. Treatment options depend on the severity of the condition and the specific factors contributing to blood vessel growth. Some common management strategies include:
Medical treatments: Topical or oral medications can be used to treat the underlying causes of corneal neovascularization, such as infections, inflammation, or autoimmune conditions. Corticosteroids, antibiotics, or antiviral medications may be prescribed to reduce inflammation and manage the primary cause.
Anti-angiogenic therapy: To directly target the blood vessel growth, anti-angiogenic medications like anti-VEGF drugs can be used. These medications help inhibit the formation of new blood vessels and may be administered through eye drops, injections, or implants.
Contact lens management: In cases where contact lens-induced hypoxia is the primary cause, the individual may need to change their contact lens habits, switch to more breathable lenses, or temporarily discontinue contact lens use to allow the cornea to recover.
Laser therapy: Photodynamic therapy (PDT) or laser photocoagulation can be used to selectively target and close abnormal blood vessels in the cornea, thereby reducing neovascularization and associated symptoms.
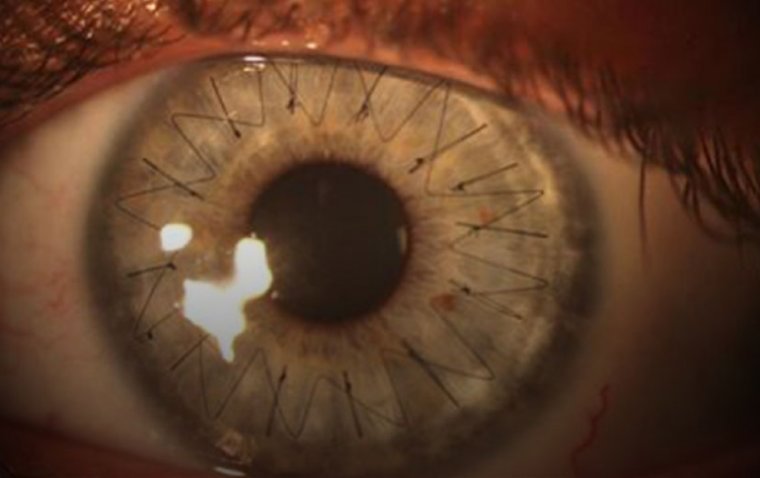
Surgical intervention: In severe cases where the cornea has been significantly damaged, a corneal transplant may be required to restore vision. However, this procedure carries the risk of graft rejection and the recurrence of neovascularization.
Monitoring and follow-up: Regular eye examinations and monitoring by an eye care professional are essential to track the progression of corneal neovascularization and adjust treatment strategies accordingly.
Nonsurgical and Surgical Management Options
Corneal neovascularization can be managed through a combination of nonsurgical and surgical interventions, depending on the severity and cause of the condition. Here is an overview of both types of management options:
Nonsurgical Management:
1. Medical treatments: Topical or oral medications, such as corticosteroids, antibiotics, or antiviral drugs, can help treat the underlying causes of corneal neovascularization, such as infections, inflammation, or autoimmune conditions.
2. Anti-angiogenic therapy: Anti-VEGF drugs can be used to directly inhibit the formation of new blood vessels. These medications may be administered as eye drops, injections, or implants, depending on the severity of the condition and the patient's needs.
3. Contact lens management: For cases caused by contact lens-induced hypoxia, adjustments in contact lens habits, switching to more breathable lenses, or temporarily discontinuing contact lens use may be necessary.
4. Lubricating eye drops: Artificial tears or lubricating eye drops can help alleviate dryness and irritation associated with corneal neovascularization.
Surgical Management:
1. Laser therapy: Photodynamic therapy (PDT) or laser photocoagulation can be employed to selectively target and close abnormal blood vessels in the cornea, reducing neovascularization and its associated symptoms.
2. Corneal transplant: In severe cases where the cornea has sustained significant damage, a corneal transplant may be required to restore vision. This procedure involves replacing the damaged corneal tissue with healthy donor tissue. However, it carries the risk of graft rejection and the recurrence of neovascularization.
3. Amniotic membrane transplantation: In some cases, amniotic membrane transplantation may be used to promote corneal healing and suppress neovascularization. This procedure involves placing a thin layer of amniotic membrane over the affected cornea to reduce inflammation and promote healing.
Preventing Corneal Neovascularization
While not all cases of corneal neovascularization can be prevented, there are steps individuals can take to reduce their risk and maintain good eye health. Some key prevention strategies include:
● Regular eye checkups: Regular eye examinations by an eye care professional can help detect early signs of corneal neovascularization and other eye conditions, enabling prompt treatment and minimizing the risk of complications.
● Proper contact lens care: For contact lens wearers, it is essential to follow proper hygiene practices, such as cleaning and storing lenses correctly, replacing them as recommended, and avoiding wearing them for extended periods. Ensuring adequate oxygen supply to the cornea by using breathable lenses can also help prevent corneal neovascularization.
● Eye protection: Wearing protective eyewear when engaging in activities that pose a risk of eye injury, such as sports or certain occupations, can help prevent corneal trauma that could potentially lead to neovascularization.
● Managing underlying conditions: Timely diagnosis and treatment of underlying medical conditions, such as autoimmune diseases or infections, can help reduce the risk of corneal neovascularization.
● Avoiding excessive UV exposure: Prolonged exposure to ultraviolet (UV) radiation can damage the cornea and contribute to neovascularization. Wearing UV-protective sunglasses and hats when outdoors can help minimize the risk.
● Maintaining a healthy lifestyle: A balanced diet, regular exercise, and good overall health can contribute to better eye health and lower the risk of developing various eye conditions, including corneal neovascularization.
While these preventive measures cannot guarantee that corneal neovascularization will not occur, they can significantly reduce the risk and help maintain optimal eye health.
Emerging Treatments and Advancements in the Field
Recent advancements in the field of ophthalmology have brought forth promising new treatment options and strategies for managing corneal neovascularization. Some of these emerging treatments and advancements include:
1. Targeted drug delivery systems: Researchers are exploring novel drug delivery systems, such as nanoparticles and hydrogels, to enhance the efficacy of anti-angiogenic medications and minimize potential side effects.
2. Gene therapy: Gene therapy aims to target the underlying genetic factors that contribute to corneal neovascularization. By modifying or silencing specific genes involved in blood vessel growth, this approach has the potential to prevent or reverse the progression of the condition.
3. Stem cell therapy: Regenerative medicine, particularly the use of stem cells, offers a promising avenue for repairing corneal tissue damaged by neovascularization. Preclinical studies have shown that certain types of stem cells can help reduce inflammation, promote healing, and inhibit the growth of abnormal blood vessels in the cornea.
4. Bioengineered corneas: Researchers are developing bioengineered corneas using a combination of biomaterials and living cells to create a functional corneal replacement for patients with severe corneal damage. This approach may offer an alternative to traditional corneal transplantation and reduce the risk of graft rejection or recurrence of neovascularization.
5. Anti-inflammatory treatments: Newer anti-inflammatory medications are being developed to better target and suppress the inflammation that contributes to corneal neovascularization. These advancements may lead to more effective treatments with fewer side effects.
6. Advanced imaging techniques: The development of sophisticated imaging technologies, such as optical coherence tomography angiography (OCTA), enables eye care professionals to visualize and monitor corneal neovascularization in greater detail. This enhanced diagnostic capability can lead to earlier detection and more precise treatment planning.
These emerging treatments and advancements hold significant promise for improving the management of corneal neovascularization and enhancing the quality of life for affected individuals. As research progresses, it is expected that these novel approaches will continue to evolve, offering more effective and targeted interventions for this challenging eye condition.
To conclude...
Corneal neovascularization is a complex eye condition that can significantly impact an individual's vision and overall quality of life. With a variety of potential causes, it is crucial to understand the signs and symptoms, as well as the importance of early detection and prompt treatment. By exploring emerging treatments and advancements in the field, there is hope for more effective management and even prevention of corneal neovascularization in the future.
In the meantime, adopting lifestyle changes and protective measures can help reduce the risk of developing this condition and maintain optimal eye health. Regular eye checkups, proper eye care, and addressing any underlying medical conditions are essential for safeguarding one's vision. As research continues to unveil new insights and treatment options, it is vital to stay informed and consult with eye care professionals to ensure the best possible outcomes for those affected by corneal neovascularization.
(1).jpg)