White Dot Syndrome in Focus: Types, Symptoms, and Treatment
What Is White Dot Syndrome?
White dot syndrome refers to a group of eye disorders characterized by the presence of white or yellowish lesions on the retina, a sensitive tissue at the back of the eye responsible for vision. These syndromes are significant in eye health as they can cause visual disturbances and potentially lead to vision loss if left untreated.
White dot syndromes are considered a spectrum of diseases, and they are named based on their clinical features and the appearance of the lesions. These syndromes typically affect the macula, the central part of the retina responsible for sharp, detailed vision, making early diagnosis and management crucial for preserving visual acuity.
Types of White Dot Syndromes
White dot syndromes encompass several distinct eye conditions, each with its own set of features and characteristics. Some of the common types include:
1. Birdshot Retinochoroidopathy (BSRC): BSRC is characterized by small, hypopigmented lesions scattered across the retina. It primarily affects the choroid, a layer of blood vessels beneath the retina. BSRC is often chronic and can lead to vision impairment.
2. Multifocal Choroiditis and Panuveitis (MCP): MCP is known for multiple, discrete yellow-white lesions in the retina. These lesions can cause inflammation throughout the uvea, which is the middle layer of the eye. MCP can result in blurred or distorted vision.
3. Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE): This syndrome presents with sudden-onset, large yellow-white lesions that primarily affect the outermost layer of the retina, the pigment epithelium. It is often self-limiting and can cause temporary vision impairment.
4. Punctate Inner Choroidopathy (PIC): PIC involves small, punctate lesions that develop in the choroid and can lead to inflammation in the retina. It predominantly affects young, myopic individuals and can result in central vision loss.
5. Serpiginous Choroiditis: This syndrome is characterized by progressive, serpentine-shaped lesions that extend from the outer retina to the choroid. It often leads to scarring and can cause significant visual impairment.
6. Acute Zonal Occult Outer Retinopathy (AZOOR): AZOOR leads to visual field defects, with lesions typically affecting the outer retinal layers. It's known for its sudden onset and may cause photopsia (flashing lights) and vision loss.
7. White Spot Syndromes: This is a more general term used to describe syndromes with characteristic white spots on the retina. It includes multiple conditions like AMN (Acute Macular Neuroretinopathy), MEWDS (Multiple Evanescent White Dot Syndrome), and others.
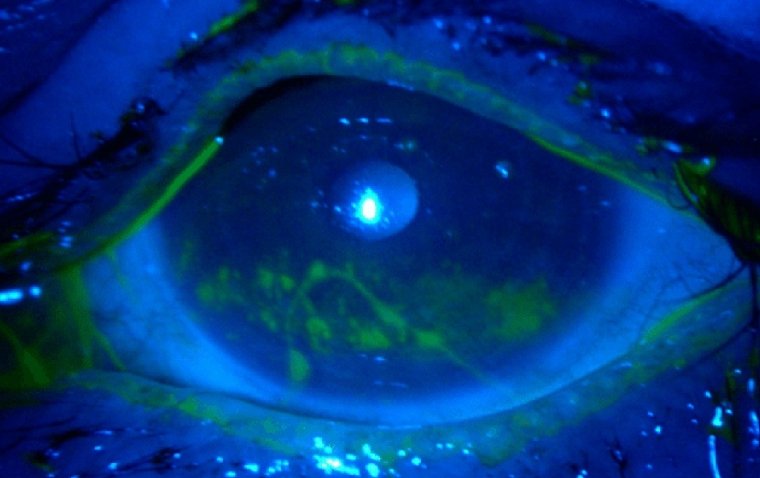
.jpg)
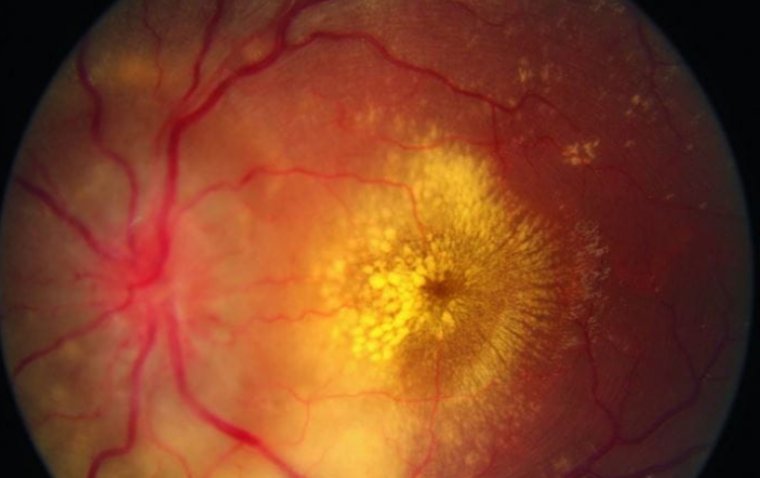
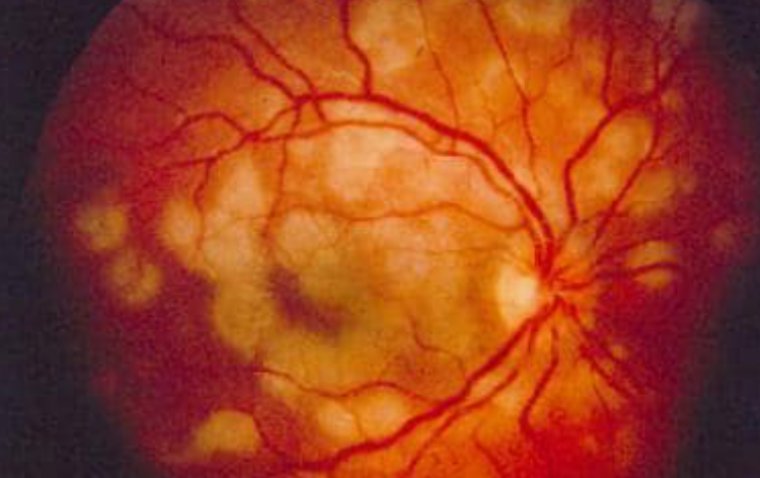
Colour fundus photographs of the left eye showing a hyperaemic, swollen optic disc and multiple white dots of the posterior pole.
Credit: Retina Associates
What Causes White Dot Syndrome?
The exact causes of white dot syndromes are not always clear, and they can vary depending on the specific type of syndrome. However, several factors and risk factors have been associated with the development of these syndromes:
● Autoimmune Factors: Many white dot syndromes are believed to have an autoimmune component, where the body's immune system mistakenly targets and attacks the retina or choroid. This immune response can lead to the formation of white lesions.
● Genetic Predisposition: Some individuals may have a genetic predisposition to developing certain White Dot Syndromes. Research has identified specific genetic markers associated with these conditions.
● Viral Infections: In some cases, viral infections may trigger an immune response that leads to White Dot Syndromes. However, this is more commonly seen in other types of uveitis.
● Environmental Factors: Environmental factors, such as exposure to toxins or infectious agents, may play a role in the development of these syndromes, although the precise mechanisms are not well understood.
● Stress and Systemic Illnesses: High levels of stress and certain systemic illnesses, such as Lyme disease and tuberculosis, have been associated with the onset or exacerbation of some White Dot Syndromes.
● Heredity: There is evidence to suggest that some White Dot Syndromes may run in families, indicating a hereditary component.
● Age and Gender: Some syndromes, like Birdshot Retinochoroidopathy, tend to affect individuals in middle age and are more common in women.
Signs and Symptoms of White Dot Syndrome
The signs and symptoms of white dot syndromes can vary depending on the specific type of syndrome. However, there are some common features that individuals with these syndromes may experience. Here are some typical signs and symptoms:
● Vision Changes: Many white dot syndromes can lead to vision problems, such as blurred vision, decreased visual acuity, and difficulty with night vision.
● Floaters: Floaters are small, dark spots or lines that appear to "float" in your field of vision. They can be a common symptom of White Dot Syndromes.
● Photopsia: Some individuals may experience photopsia, which is the perception of flashing lights or bright spots in their vision.
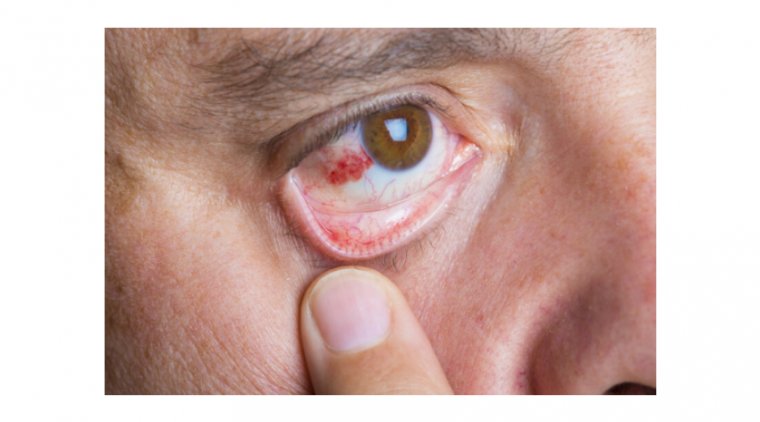
● Eye Pain or Discomfort: Eye pain, redness, or discomfort can occur in some cases, particularly when the uvea (the middle layer of the eye) is inflamed.
● Scotomas: Scotomas are areas of decreased or lost vision within the visual field. These blind spots can be a hallmark of certain White Dot Syndromes.
● Photophobia: Sensitivity to light, known as photophobia, is another common symptom seen in some White Dot Syndromes. Bright lights can cause discomfort and glare.
● Color Vision Changes: Some individuals may notice changes in their ability to perceive colors, often described as a desaturation of colors or difficulty distinguishing certain hues.
● Amsler Grid Distortions: Distortions when looking at an Amsler grid (a grid of straight lines used for self-monitoring of vision) can be indicative of certain White Dot Syndromes.
● Peripheral Vision Loss: In some cases, peripheral vision loss may occur, affecting your ability to see objects or movement at the edges of your visual field.
● Bilateral Involvement: Many white dot syndromes tend to affect both eyes, although the severity can differ between the eyes.
How is White Dot Syndrome Treated?
The treatment of white dot syndromes varies depending on the specific syndrome, its severity, and the patient's individual factors. Here is an overview of the treatment methods commonly employed:
1. Observation: In some cases, particularly in milder forms of WDS like multifocal choroiditis, no active treatment may be necessary. The condition may resolve on its own over time. However, close monitoring by an eye care specialist is crucial to track changes and intervene if needed.
2. Corticosteroids: These anti-inflammatory medications are often the first line of treatment for many WDS. They can be administered in various forms, including oral steroids, steroid eye drops, or intravitreal injections. Corticosteroids help reduce inflammation and manage symptoms.
3. Immunosuppressive Therapy: For severe or chronic WDS cases, immunosuppressive medications may be prescribed. These drugs help suppress the immune system's abnormal response that triggers inflammation in the eye. Methotrexate, mycophenolate, and azathioprine are examples of such medications.
4. Biologic Agents: In some cases, biologic agents such as tumor necrosis factor (TNF) inhibitors may be used to modulate the immune response. These are often reserved for refractory cases or when corticosteroids pose risks due to prolonged use.
5. Photodynamic Therapy (PDT): PDT involves the administration of a light-activated medication followed by the application of a laser to target abnormal blood vessels in the eye. This approach is used in specific WDS where abnormal blood vessel growth is a concern.
6. Surgical Intervention: In rare cases, surgical procedures may be required. This could include interventions like vitrectomy to remove vitreous gel or repair retinal detachments that may occur as complications of WDS.
7. Lifestyle and Dietary Modifications: Some patients may benefit from lifestyle changes such as adopting a diet rich in antioxidants and omega-3 fatty acids, which can support eye health. Smoking cessation is also strongly advised as it can exacerbate WDS.
8. Regular Monitoring: Regardless of the treatment chosen, regular follow-up appointments with an eye care specialist are essential. WDS is a complex condition that may require ongoing management, and monitoring helps track progress and adjust treatment plans as needed.
Preventing White Dot Syndrome
Preventing white dot syndromes (WDS) primarily involves adopting a few general measures to maintain overall eye health and potentially reduce the risk of these rare conditions. While there are no foolproof methods for preventing WDS, these strategies can help:
Regular Eye Check-ups: Schedule routine eye examinations with an ophthalmologist. Early detection of any eye issues, including WDS, can lead to prompt treatment and better outcomes.
Eye Protection: Use appropriate eye protection when engaging in activities that could put your eyes at risk of injury. This includes wearing safety goggles when working with hazardous materials or participating in sports where eye injuries are possible.
Healthy Lifestyle: Maintain a healthy lifestyle that includes a balanced diet rich in antioxidants and omega-3 fatty acids. These nutrients are beneficial for eye health. Staying hydrated is also important.
Smoking Cessation: If you smoke, quitting is highly advisable. Smoking is linked to various eye conditions, including those associated with WDS.
Manage Underlying Health Conditions: If you have autoimmune diseases or conditions like diabetes, work closely with your healthcare provider to manage them effectively. Controlling underlying health issues can sometimes reduce the risk of eye-related complications.
Eye Hygiene: Practice good eye hygiene by ensuring clean contact lenses and proper lens care if you wear them. Avoid rubbing your eyes excessively, as this can potentially irritate them.
Manage Allergies: Allergies can sometimes trigger inflammation in the eyes. If you have allergies, follow your allergist's advice for managing them.
UV Protection: Wear sunglasses that provide adequate UV protection when outdoors. Prolonged UV exposure can contribute to eye issues.
Summary
In summary, white dot syndromes encompass a group of rare but significant eye conditions that can affect individuals of various ages. These syndromes are characterized by the presence of white or yellowish lesions on the retina, which can lead to vision disturbances and discomfort.
Understanding the different types of WDS and their unique characteristics is essential for both healthcare professionals and individuals to identify and manage these conditions effectively. While the exact causes of WDS are not always clear, factors like genetics, autoimmune responses, and infections may play a role.
Recognizing the signs and symptoms of WDS, which can include blurred vision, blind spots, and visual distortions, is crucial. Early diagnosis through specialized eye evaluations is key to initiating appropriate treatment promptly. Treatment options for WDS may vary depending on the specific syndrome but can include medications, laser therapy, and other surgical interventions.
While it's challenging to prevent WDS outright, maintaining overall eye health through regular check-ups, protective measures, a healthy lifestyle, and managing underlying health conditions can help reduce the risk. Additionally, seeking professional medical advice for any concerning eye symptoms is paramount.
(1).jpg)