Idiopathic Multifocal Choroiditis: A Review of Epidemiology and Risk Factors
What Is Idiopathic Multifocal Choroiditis?
Idiopathic Multifocal Choroiditis (IMFC) is a rare eye condition that primarily affects the choroid, a vascular layer situated between the retina and the sclera (the white part of the eye). The condition is characterized by the presence of multiple inflamed lesions or spots in the choroid, which can lead to vision disturbances and, in severe cases, loss of vision. The term 'idiopathic' denotes that the exact cause of the condition is unknown, making it distinct from choroiditis resulting from known factors like infections or systemic diseases.
One of the unique characteristics of IMFC is its tendency to affect younger adults and its propensity for bilateral occurrence—meaning it often impacts both eyes. Unlike more common eye conditions such as macular degeneration or diabetic retinopathy, IMFC doesn't have a well-understood cause or risk factors, making it challenging to predict and manage. Its symptoms can also be like those of other eye conditions, but its pathology and manifestations in the choroid make it distinct.
Causes of Idiopathic Multifocal Choroiditis
As the name suggests, Idiopathic Multifocal Choroiditis (IMFC) is idiopathic in nature, meaning the root cause of the condition is still not fully understood. Research is ongoing, and several theories propose that autoimmunity, inflammatory responses, or a yet-to-be-identified trigger could play a role in the onset of this disorder.
Risk Factors
Although the cause of IMFC is unclear, certain risk factors have been identified that may increase the likelihood of developing the condition:
1. Age: IMFC is more commonly seen in younger adults, unlike other eye conditions that are often associated with aging.
2. Gender: Some studies suggest a slight female preponderance, although the condition can affect both genders.
3. Family History: While there is no definitive evidence to link genetics and IMFC, having a family history of ocular or autoimmune diseases could potentially increase the risk.
4. Systemic Inflammatory Conditions: Individuals with other systemic inflammatory or autoimmune diseases might be at an increased risk, although concrete evidence is lacking.
5. Environmental Triggers: Though not confirmed, some researchers are investigating whether environmental factors like toxins or infections could contribute to the onset of IMFC.
Symptoms and Diagnosis of Idiopathic Multifocal Choroiditis
Idiopathic Multifocal Choroiditis (IMFC) is often characterized by a range of symptoms that can vary in severity from mild to significant. The common symptoms include:
● Vision Changes: Individuals may experience blurred vision or the presence of dark spots in their field of vision, often referred to as "floaters."
● Photopsia: Brief flashes of light or other photic phenomena may be noticed.
● Eye Discomfort: Though less common, some individuals report mild discomfort, itching, or a sensation of having a foreign body in the eye.
● Distorted Vision: In more severe cases, individuals might notice distorted vision, including the bending of straight lines.
● Sudden Loss of Vision: In extreme cases, IMFC can lead to a rapid decline in visual acuity, warranting immediate medical attention.
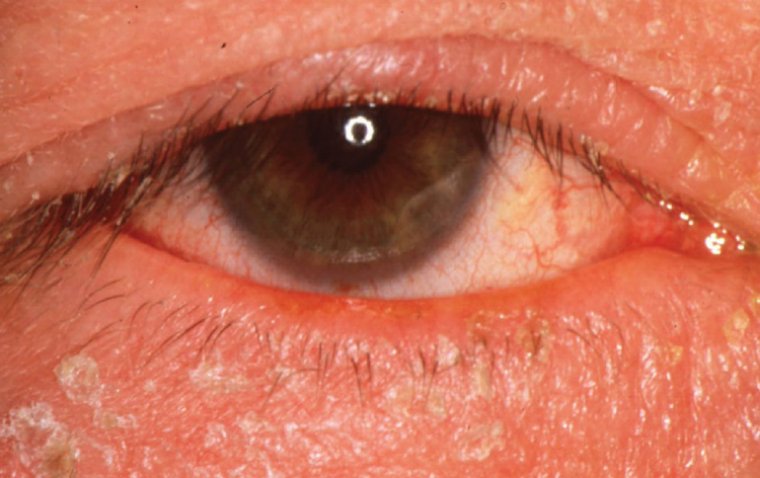
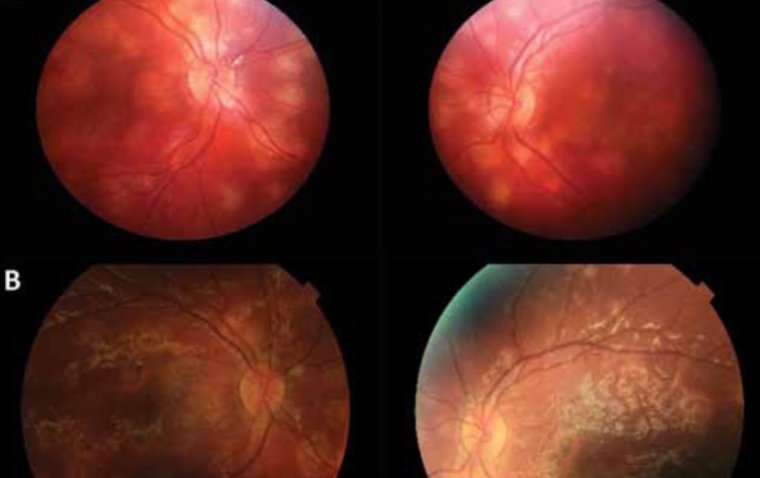
Credit: Research Gate
How to Diagnose
Diagnosing IMFC involves a multi-faceted approach, often starting with a comprehensive eye examination that could include:
● Clinical Assessment: A detailed history is taken to understand the patient’s symptoms, any precipitating factors, and family medical history.
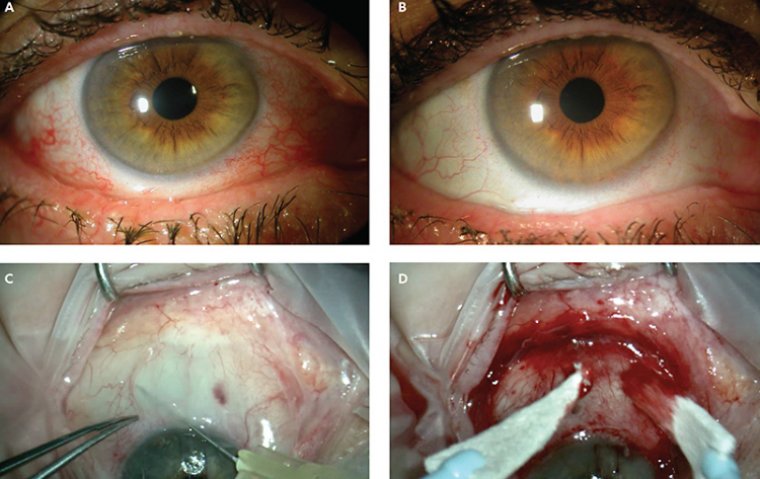
● Slit-lamp Examination: This allows the ophthalmologist to examine the front and back portions of the eye in detail.
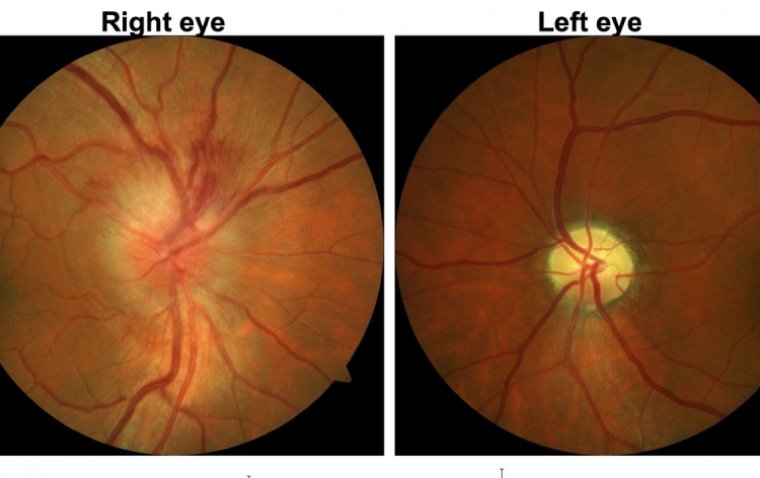
● Fundus Examination: To examine the back of the eye, including the retina and choroid.
● Optical Coherence Tomography (OCT): This imaging technique provides cross-sectional images of the retina, helping to identify any inflammation or abnormalities in the choroid layer.
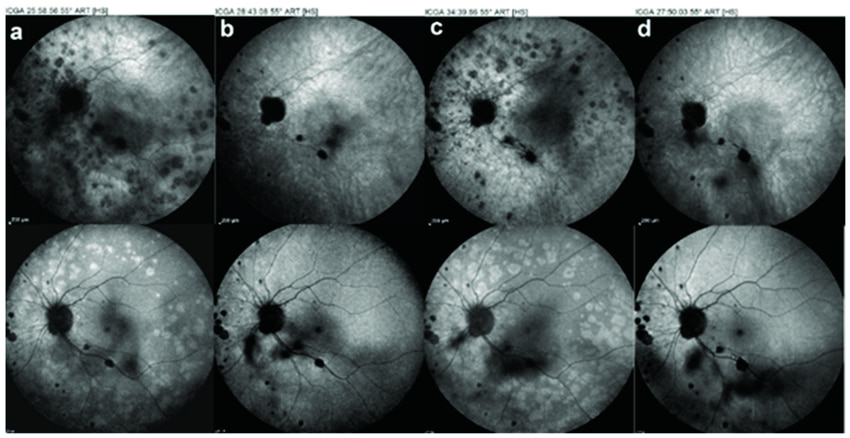
● Fluorescein Angiography: This involves injecting a dye into the bloodstream and taking images as the dye passes through the blood vessels in the retina, aiding in the identification of inflammatory sites.
● Indocyanine Green Angiography: Similar to fluorescein angiography but utilizes indocyanine green dye to visualize blood flow in the choroid, the layer of blood vessels under the retina.
Can Idiopathic Multifocal Choroiditis Be Cured?
There is no definitive cure for Idiopathic Multifocal Choroiditis (IMFC), but several treatment options are available to manage symptoms and slow the progression of the disease. The emphasis is often on early intervention and a personalized approach to care.
Treatment Options
1. Corticosteroids: These are commonly used to control inflammation and can be administered through eye drops, oral medications, or injections.
2. Immunomodulatory Therapy: For cases that don't respond well to corticosteroids or for long-term management, immunosuppressive medications like methotrexate or azathioprine may be considered.
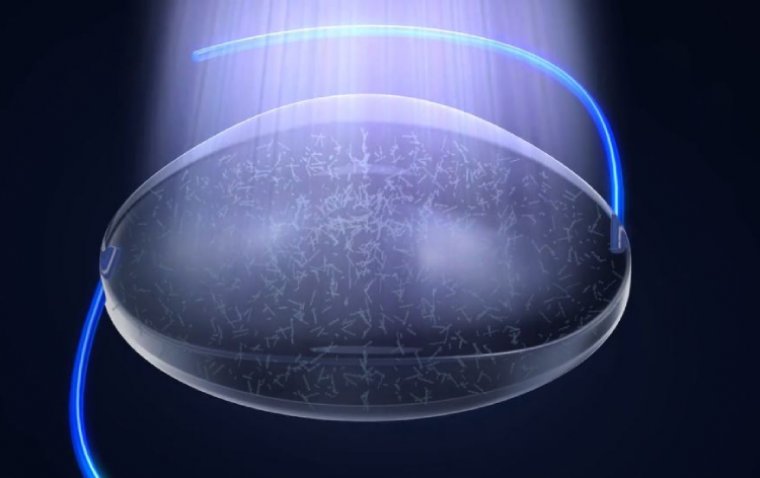
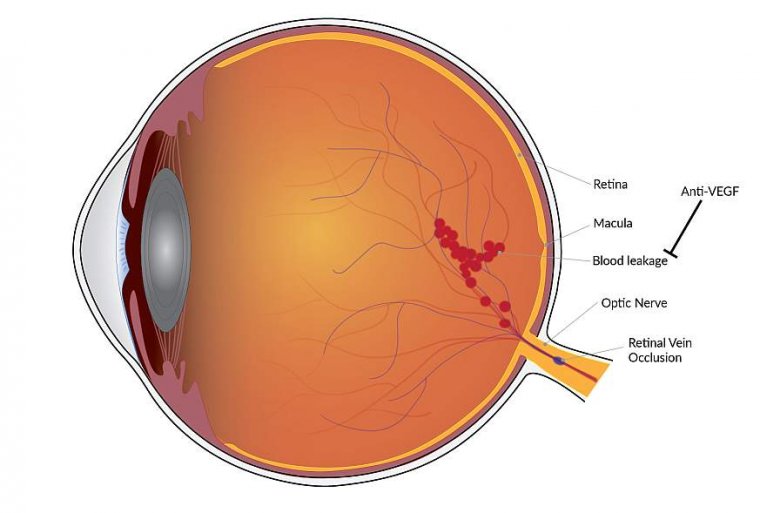
3. Anti-VEGF Therapy: Drugs that inhibit Vascular Endothelial Growth Factor (VEGF) may be used in cases where neovascularization (new blood vessel growth) has occurred, leading to wet macular degeneration.
4. Laser Photocoagulation: This treatment is less commonly used but might be considered for sealing leaking blood vessels in the eye.
5. Pars Plana Vitrectomy: In advanced or complicated cases, a surgical procedure to remove some of the vitreous humor from the eye may be considered.
Importance of Early Intervention
Catching IMFC in its early stages offers the best chance for effective management. Earlier treatment can prevent more significant vision loss and complications. It's important to have a tailored treatment plan, developed in collaboration with your healthcare providers, to manage IMFC symptoms effectively.
What Is the Prognosis for Idiopathic Multifocal Choroiditis?
The prognosis for Idiopathic Multifocal Choroiditis (IMFC) varies widely among individuals and is influenced by several factors such as the severity of the condition at the time of diagnosis, the effectiveness of the treatment regimen, and the patient's overall health. Due to the unpredictable nature of the disease, it's challenging to provide a one-size-fits-all prognosis.
Key Influencing Factors
Severity at Diagnosis: Earlier diagnosis generally allows for a more optimistic outcome, as timely treatment can often slow the disease's progression and mitigate symptoms.
Response to Treatment: Individuals who respond well to corticosteroids or other immunomodulatory medications often have a better prognosis than those who do not.
Associated Complications: The presence of complications such as macular edema or choroidal neovascularization can negatively affect the prognosis.
Comorbidities: Other health conditions, especially those that impact the immune system, can also influence the prognosis.
Lifestyle Factors: Smoking, poor diet, and lack of regular eye check-ups can adversely affect the long-term outlook for patients with IMFC.
Monitoring and Regular Check-ups
Given the variable nature of IMFC, regular monitoring is essential. Patients should maintain frequent follow-up appointments with their ophthalmologist to adapt their treatment plan as necessary. New imaging techniques and treatment modalities are continually being researched, offering hope for better management strategies in the future.
Can multifocal Choroiditis Cause Blindness?
Multifocal Choroiditis (MFC) is a condition that can potentially have severe implications for vision, including the possibility of blindness if left untreated or inadequately managed. However, it's crucial to emphasize that not all cases of MFC lead to blindness. The risk is often dependent on several factors such as the severity of the disease, the effectiveness of the treatment, and the presence of complications.
Factors Contributing to Vision Loss
1. Severity and Extent of Lesions: The choroidal lesions typical of MFC can occur in various parts of the retina. If these lesions affect the macula or other critical vision areas, the risk of significant vision loss or blindness is higher.
2. Associated Complications: Complications like macular edema, choroidal neovascularization, or retinal scarring can exacerbate vision problems and, in worst-case scenarios, lead to blindness.
3. Delayed Diagnosis and Treatment: A late diagnosis and delayed treatment can result in irreversible damage to the retina and choroid, increasing the risk of vision loss.
4. Ineffectiveness of Treatment: In some cases, the condition might not respond well to typical treatment options like corticosteroids or immunosuppressive medications, leading to a poor prognosis for vision.
5. Cumulative Damage: Recurrent episodes without adequate treatment can cause cumulative damage to the eye, contributing to vision loss over time.
Importance of Early Detection and Treatment
Early detection and appropriate treatment are key to minimizing the risk of severe vision loss or blindness. Regular eye check-ups, especially for individuals at higher risk, can be crucial for early diagnosis. Treatment usually involves anti-inflammatory medications, and in some instances, laser therapy or injections into the eye may be required. The effectiveness of these treatments can differ among individuals, so a personalized treatment plan is essential.
Summary
Idiopathic Multifocal Choroiditis (IMFC) is a complex and not fully understood eye condition that can significantly impact one's vision and overall eye health. The disease presents with symptoms such as vision changes and eye discomfort, and it requires specialized diagnostic techniques for proper identification.
While there is currently no cure for IMFC, early intervention and a personalized treatment plan can go a long way in managing symptoms and slowing down the disease's progression. The prognosis can vary widely among individuals, and although severe cases can result in significant vision loss, timely treatment can often prevent the most devastating outcomes.
The stakes are high when it comes to eye health; therefore, if you experience any eye-related symptoms, it is imperative to consult a healthcare professional as soon as possible. Proper diagnosis and prompt treatment are critical factors in managing IMFC and other eye conditions effectively. Taking proactive steps can make all the difference in maintaining your vision and overall eye health.
FAQ
The exact cause of IMC is unknown, hence the term idiopathic. It is believed to have an autoimmune component, where the body's immune system mistakenly attacks the eye's tissues.
(1).jpg)