Pars Plana Vitrectomy (PPV) & Patients Education
Pars plana vitrectomy (PPV) is a surgical procedure introduced by Robert Machemer that provides access to the posterior segment of the eye, allowing for the treatment of various vitreoretinal diseases. This technique has revolutionized ophthalmic surgery by enabling the management of conditions that were once considered untreatable, thereby significantly improving patient outcomes and quality of life.
Understanding Pars Plana Vitrectomy
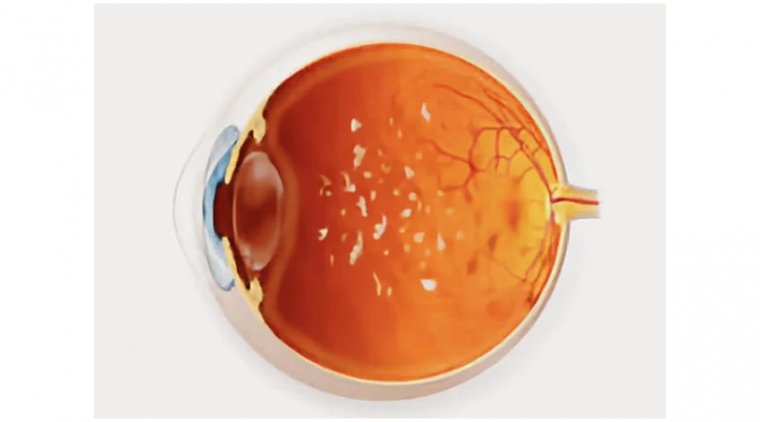
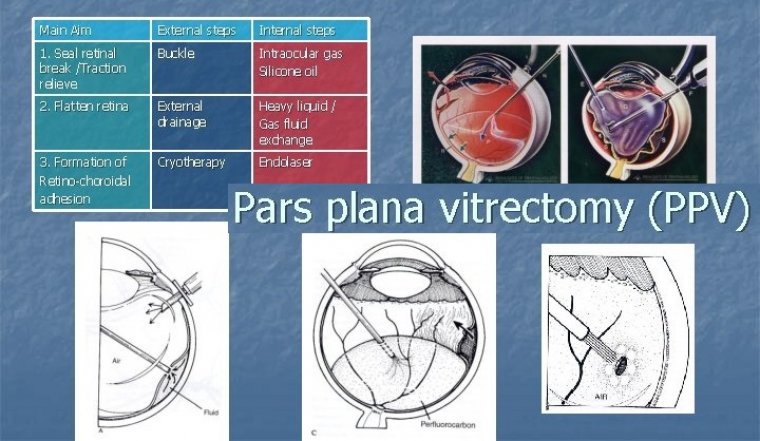
PPV involves the removal of the vitreous gel—a clear, jelly-like substance filling the eye's interior—to address disorders affecting the retina and vitreous. By accessing the vitreous cavity and retina, surgeons can treat a wide range of conditions, including retinal detachments, macular holes, epiretinal membranes, vitreous hemorrhages, and intraocular tumors.
Importance of Technical Skill and Knowledge
Performing a PPV requires a high level of technical skill and comprehensive knowledge of ocular anatomy and pathology. Surgeons must be proficient with specialized instruments and techniques to minimize risks and ensure optimal visual outcomes. The delicate nature of retinal tissues demands precision and expertise to prevent complications such as retinal tears or infections.
Balancing Benefits and Complications
While PPV can restore vision and alleviate symptoms, it carries potential risks like any surgical procedure. Complications may include infection, bleeding, cataract formation, increased intraocular pressure, and retinal detachment. Therefore, a thorough understanding of the procedure and meticulous post-operative care are essential to maximize benefits and minimize risks.
Indications for Pars Plana Vitrectomy
PPV is indicated for various vitreoretinal conditions:
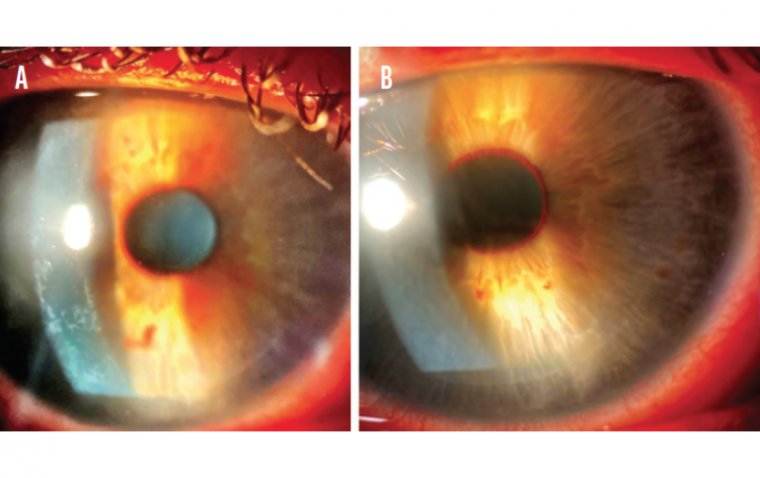
• Vitreous Opacification: Non-clearing vitreous hemorrhage caused by proliferative diabetic retinopathy, trauma, or retinal vascular diseases can obscure vision. PPV removes the opacified vitreous, restoring visual clarity.
• Retinal Detachments: PPV allows for reattachment of the retina by removing tractional forces and applying laser therapy or gas tamponade to seal retinal breaks.
• Macular Disorders: Conditions like macular holes and epiretinal membranes can be treated by removing the vitreous and peeling away abnormal tissues to improve central vision.
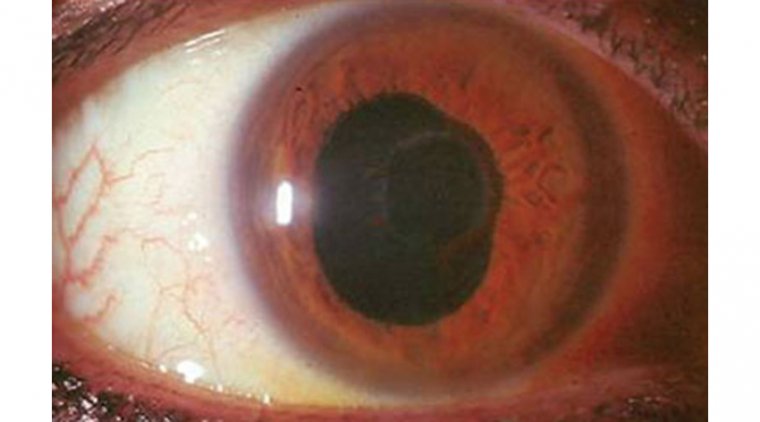
• Intraocular Infections and Inflammations: Severe cases of endophthalmitis or uveitis may require PPV to remove infectious agents and inflammatory debris.
• Intraocular Foreign Bodies: PPV facilitates the safe removal of foreign materials lodged within the eye due to injury.
Advances in Vitrectomy Techniques
Since the development of the modern three-port vitrectomy system by Conor O’Malley and Ralph Heintz in 1974, significant advancements have enhanced the safety and efficacy of PPV:
• Smaller Gauge Instruments: Transitioning from 20-gauge to 23, 25, and even 27-gauge instruments has led to minimally invasive procedures with smaller incisions, reduced trauma, and faster recovery times.
• Enhanced Vitrectomy Machines: Modern machines offer higher cut rates and maintain stable intraocular pressures, reducing the risk of complications like retinal tears.
• Improved Visualization Systems: Innovations such as "heads-up" three-dimensional viewing systems with 3D glasses provide surgeons with superior visualization of the retinal structures, enhancing surgical precision.
Patient Education and Informed Consent
Educating patients is a critical component of preoperative preparation. Patients should be fully informed about:
• The Procedure: Understanding what PPV entails and why it is necessary for their specific condition.
• Risks and Benefits: A candid discussion about potential complications and the expected outcomes helps patients make informed decisions.
• Alternative Treatments: Exploring other therapeutic options, if available, ensures patients are aware of all possible interventions.
• Preoperative Instructions: Guidance on medication adjustments, fasting requirements, and arrival times for surgery.
Obtaining informed consent not only fulfills ethical and legal obligations but also fosters trust and collaboration between the patient and healthcare team.
Preparing for Surgery
Preoperative Considerations
Patients should receive clear instructions regarding:
• Attire: Wearing comfortable clothing and removing accessories like jewelry or contact lenses.
• Dietary Restrictions: Following fasting guidelines if sedation or general anesthesia is planned.
• Medication Management: Adjusting or discontinuing medications that may affect bleeding or interact with anesthesia.
• Anesthesia Options: Discussing the use of local anesthesia with sedation versus general anesthesia based on the patient's health status and anxiety levels.
Importance of Anesthesia and Eye Immobilization
To ensure patient comfort and surgical precision, a retrobulbar block is often administered. This local anesthetic technique achieves akinesia (loss of movement) and anesthesia of the eye, minimizing discomfort and preventing involuntary eye movements during the delicate procedure.
The Surgical Procedure
PPV surgery involves several key steps:
- Gaining Access: The surgeon creates small incisions (sclerotomies) in the pars plana region to insert specialized instruments, including a light source, infusion line, and vitreous cutter.
- Performing the Vitrectomy: The vitreous gel is carefully removed using the vitreous cutter, which simultaneously cuts and aspirates the gel.
- Addressing the Pathology: Depending on the condition, the surgeon may perform additional procedures such as membrane peeling, laser photocoagulation to seal retinal breaks, or injecting intraocular medications.
- Closing the Incisions: The small incisions often self-seal due to the tiny instrument size, but sutures may be placed if necessary to ensure wound closure.
Postoperative Care and Recovery
Aftercare Instructions
Proper postoperative care is essential for healing and includes:
• Head Positioning: If a gas or air bubble is placed in the eye to tamponade retinal breaks, specific head positioning is required to keep the bubble in contact with the affected area. The surgeon will provide detailed instructions based on the location of the retinal pathology.
• Activity Restrictions: Patients should avoid strenuous activities, heavy lifting, and any actions that may increase intraocular pressure.
• Medication Adherence: Prescribed eye drops, including antibiotics and anti-inflammatory agents, should be used as directed to prevent infection and control inflammation.
• Protective Eyewear: Wearing an eye shield, especially while sleeping, protects the eye from accidental trauma.
• Follow-Up Appointments: Attending all scheduled visits allows the surgeon to monitor healing progress and manage any complications promptly.
Recovery Expectations
• Visual Recovery: Vision may be blurred or distorted initially. Gradual improvement is expected over several weeks to months, depending on the underlying condition and the extent of surgery.
• Possible Symptoms: Mild discomfort, redness, and sensitivity to light are common. Severe pain, sudden vision loss, increased redness, or discharge should be reported immediately.
Potential Risks and Complications
While PPV is generally safe, patients should be aware of possible complications:
• Infection (Endophthalmitis): Although rare, it is a serious condition that requires immediate treatment to prevent vision loss.
• Bleeding: Intraoperative or postoperative hemorrhage can affect visual outcomes and may necessitate additional interventions.
• Cataract Formation: The development or progression of cataracts is common after PPV, particularly in older adults, potentially requiring cataract surgery later on.
• Retinal Detachment: New or recurrent detachments may occur, which might need further surgical repair.
• Elevated Intraocular Pressure: Increased pressure can lead to glaucoma; monitoring and managing intraocular pressure is crucial during follow-up.
The Impact of Modern Retina Surgery
Advancements in PPV have transformed the management of vitreoretinal diseases. Procedures that were once high-risk with limited success are now performed routinely with favorable outcomes. Early intervention with PPV can preserve vision, enhance visual acuity, and significantly improve patients' quality of life.
(1).jpg)