How to Diagnose and Treat Thyroid Eye Disease
TED is an autoimmune disease in which the eye muscles and fatty tissue behind the eye become inflamed. This inflammation can push the eyes forward (“staring” or “bulging”) or cause the eyes and eyelids to become red and swollen.
In some individuals, the inflammation may involve the eye muscles, causing the eyes to become out of line, leading to double vision. In rare cases, TED can cause blindness from pressure on the nerve in the back of the eye or ulcers that form on the front of the eye (cornea).
TED is an autoimmune disease, meaning that the inflammation and scarring are caused by an attack from the body’s immune system.
TED is primarily associated with an over-active thyroid gland due to Graves’ disease, although it can rarely occur in patients with an under-active or normally functioning thyroid gland.
About a quarter of patients with Graves’ disease develop TED before, during or after the diagnosis of a thyroid disorder. TED is also known as Graves’ orbitopathy (GO) or Graves’ eye disease (GED). Smokers are two to eight times more likely to develop TED.
The emergence of novel monoclonal antibodies is changing our management of complex ophthalmic conditions. One example is thyroid eye disease (TED). It is important to recognize if a patient has TED to elicit a focused, detailed clinical history and determine the appropriate diagnostic testing required.
This includes carefully checking for a relative afferent pupillary defect, assessing motility, stereopsis, and obtaining a static visual field. Here, we discuss the latest in our understanding of how to diagnose and treat TED.
TED is the most common cause of proptosis and eyelid retraction in adults. It affects approximately 25% to 40% of patients with thyroid dysfunction. Each year, approximately 6 million people are diagnosed with TED.
These patients suffer from significant facial disfigurement and visual disability, which inadvertently affects nearly every aspect of their lives. TED patients have nearly double the rates of anxiety and depression as compared to the general population.
Studies assessing quality of life in this group have consistently found an overall negative impact on daily quality of life, their social and occupational lives. This is particularly so for patients who suffer from diplopia.
There is both temporary and permanent occupational disability associated with this condition. The activation of orbital fibroblasts by autoantibodies in TED patients results in the production and release of chemical signals and biological materials, which trigger swelling and congestion in the orbit.
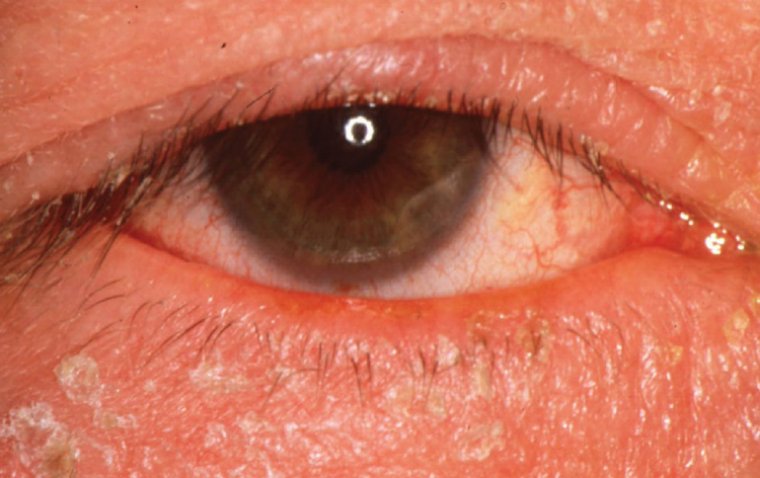
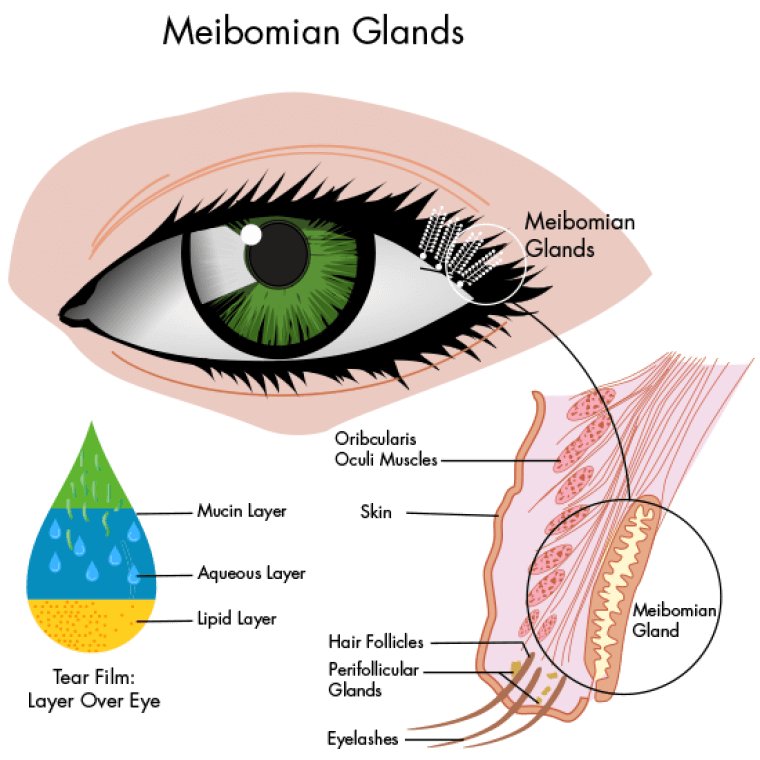
In the initial stages, TED causes eyelid changes that include retraction, lateral fl are, periorbital edema, and incomplete eyelid closure (lagophthalmos), which can give rise to ocular dryness and significant discomfort.
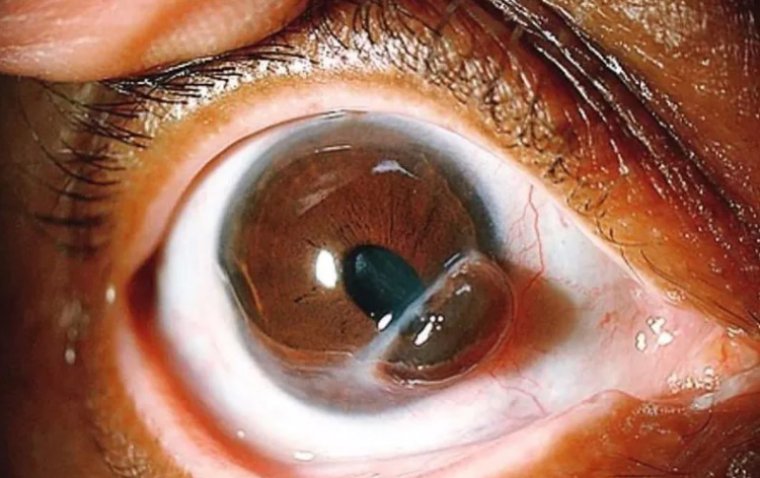
Patients can also experience a more debilitating form of TED where there is significant enlargement of extraocular muscles and orbital fat leading to proptosis and diplopia.
In extreme causes, the enlargement of the extraocular muscles at the apex is significant enough to cause optic nerve compromise resulting in permanent visual loss.
Women are five to six times more likely to develop TED. Cigarette smokers are at significantly increased risk of developing TED, often having a more severe and prolonged activity course that threatens vision.
Diagnosis and imaging TED has an active phase that involves acute exacerbation of inflammation and worsening ocular signs that can last from 6-36 months. A chronic inactive phase follows, in which scar tissue and fibrosis of tissues occur.
Due to its widespread availability and rapid image acquisition, computed topography (CT) of the orbits is an ideal choice for imaging. Bilateral enlargement of the extraocular muscle bellies with sparing of the tendinous insertions is characteristically seen.
The extraocular muscles affected by TED in decreasing order of frequency is captured by the mnemonic I’M SLOw (Inferior rectus, Medial rectus, Superior rectus, Lateral rectus and Oblique muscles).
Therapy Conventional therapy for active TED has included weekly methylprednisolone (Solu-MEDROL, Pfizer) intravenous infusions for a 12-week duration and/or orbital radiation, both of which are associated with substantial risks.
Steroids can lead to worsening diabetes, cardiovascular disease, glaucoma, increased risk of osteoporosis, development of avascular hip necrosis, weight gain, mood changes, and lowered resistance to infections.
Orbital radiation has been known to cause premature development of cataracts, radiation retinopathy, and the theoretical concern for tumorigenesis. Orbital decompression is a primary treatment of proptosis.
This surgical procedure enlarges the existing space in the orbits by partially removing the bony walls of the orbit (typically the orbital floor, medial and lateral walls). To correct large-angle diplopia, strabismus surgery is considered following the orbital decompression and after the muscle alignment is stable for months.
Eyelid retraction surgery and tarsorrhaphy is done as a final stage to address persisting eyelid issues or resolve exposure keratitis. This lengthy process involves multiple staged procedures and requires patients to be out of the workforce for extensive periods of time, negatively impacting their employment.
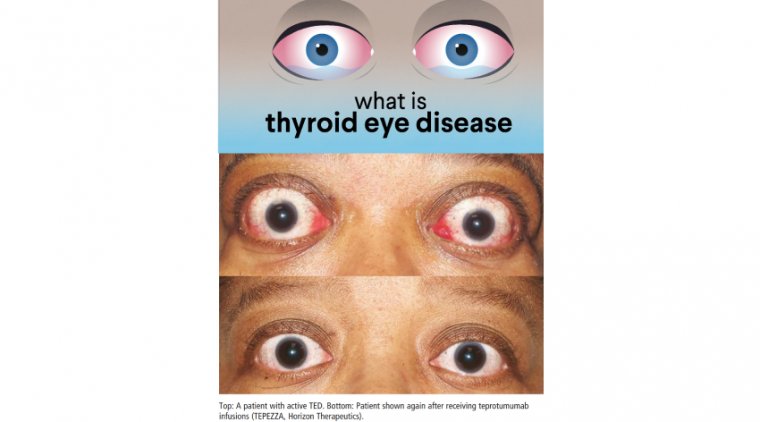
It also contributes to increases in health-care utilization. TEPEZZA - A newer option for treatment is teprotumumab (TEPEZZA, Horizon Therapeutics), the first FDA-approved drug for TED. TEPEZZA is a human monoclonal antibody against the insulin-like growth factor type I receptor (IGF-IR).
In a multicenter randomized clinical trial for active thyroid-associated ophthalmopathy, teprotumumab was found to be more effective than placebo and subsequently received FDA approval for treatment of moderate-to-severe active TED.
Patients treated with teprotumumab demonstrated improvement in their measured proptosis and Clinical Activity Score, which measures symptoms such as pain, swelling, and inflammation.
Subjective diplopia and quality of life were reported as significantly better in clinical trials.
TEPEZZA exhibited an overall favorable safety profile. Most common adverse events were mild to moderate, with none leading to discontinuation. These included hyperglycemia, muscle cramps, and transient auditory side effects.
Patients undergo a TEPEZZA infusion every 3 weeks (doses begin at 10mg/kg and go up to 20mg/kg) for a total of eight infusions. The first two doses are administered over 90 minutes, and subsequent doses are given over 60 minutes.
Also, it’s important to note that insurance coverage for TEPEZZA can sometimes take up to 75 days to process. Regardless of this, TEPEZZA appears to have promising outcomes for active TED, providing results that would have generally taken months or years to achieve with conventional therapies, if at all.
Few studies have started to explore its efficacy in treating chronic TED. This would undoubtedly change our outlook for what has long been a disfiguring and disabling condition.
While long-term data and safety profile is needed for TEPEZZA, the clinical studies thus far have shown promising outcomes. The availability and advances in monoclonal antibodies are changing the way in which we manage TED patients for the better.
(1).jpg)