The Dangers of Plaquenil: Understanding Retinal Toxicity
What Is Plaquenil Retinal Toxicity?
Plaquenil (hydroxychloroquine) is a medication used to treat autoimmune diseases such as lupus and rheumatoid arthritis. However, in rare cases, it can cause damage to the retina, a layer of tissue at the back of the eye responsible for transmitting visual information to the brain. This is known as Plaquenil retinal toxicity.
The toxicity is believed to be related to the medication's accumulation in the retina over time, causing damage to the retinal cells. Symptoms of Plaquenil retinal toxicity may include blurred or distorted vision, difficulty seeing in dim light, and changes in color vision. Sometimes, the damage may be irreversible, leading to permanent vision loss.
What Causes Plaquenil Retinal Toxicity?
The exact mechanism of Plaquenil retinal toxicity is not fully understood. However, it is believed to be related to the medication's ability to accumulate in the retina over time. Plaquenil is taken up by the pigmented cells in the retina, which act as a storage reservoir for the drug.
Plaquenil is also known to interfere with the metabolism of the retina's cells, including the photoreceptor cells and the retinal pigment epithelium (RPE) cells. The RPE cells are responsible for maintaining the health and function of the retina's photoreceptor cells.
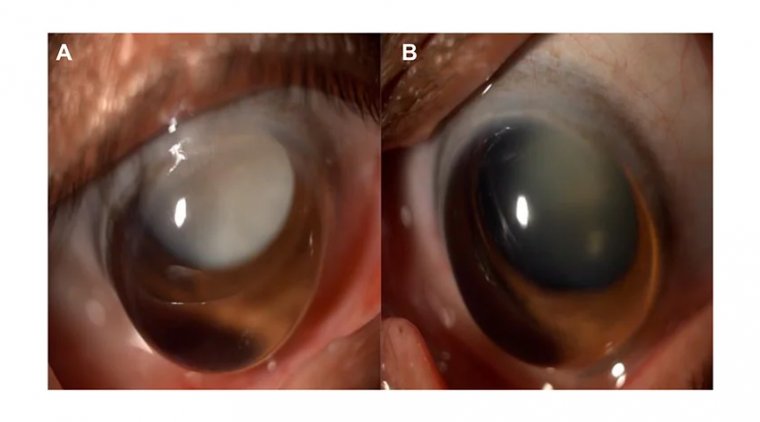
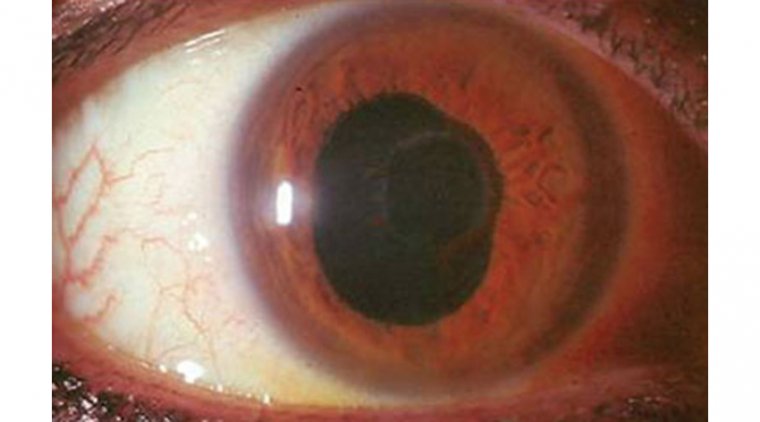
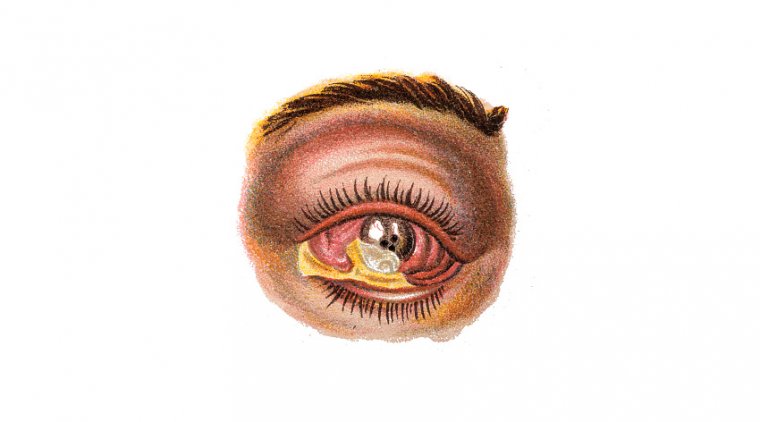
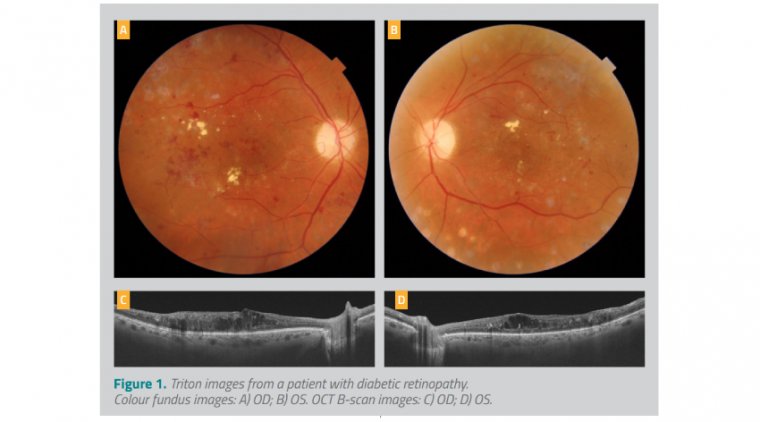
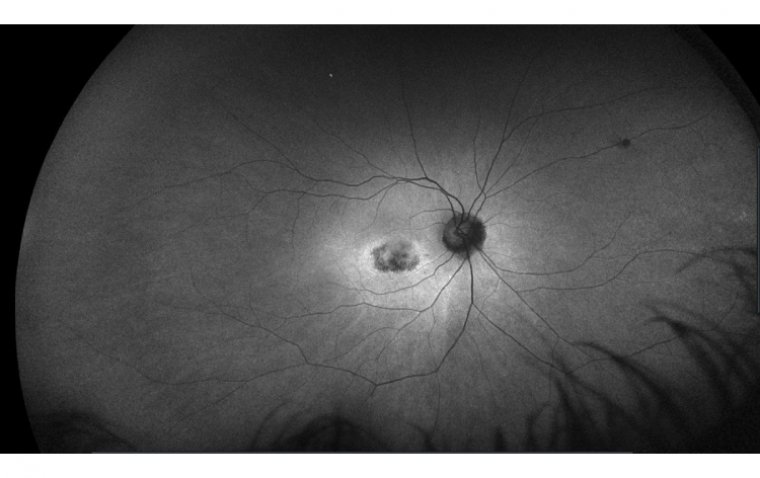
The accumulation of Plaquenil in the RPE cells and the photoreceptor cells can lead to cellular damage and death, which can cause visual symptoms. The damage can also result in the formation of deposits in the retina known as "bull's eye maculopathy" or "flying saucer sign." These deposits can be seen on an eye exam and are a hallmark sign of Plaquenil retinal toxicity.
The risk of Plaquenil retinal toxicity is related to the duration and dose of the medication. The longer a patient takes Plaquenil and the higher the dose, the greater the risk of developing retinal toxicity. Other factors that may increase the risk of toxicity include pre-existing retinal disease, kidney or liver dysfunction, and age over 60.
What Are the Symptoms of Plaquenil Retinal Toxicity?
The symptoms of Plaquenil retinal toxicity can be variable and may not be noticeable in the early stages. Some of the symptoms of Plaquenil retinal toxicity include:
● Blurred or distorted vision
● Difficulty seeing in dim light
● Changes in color vision, such as difficulty distinguishing between colors
● Difficulty reading or performing tasks that require fine vision
● Loss of central vision or blind spots in the visual field
These symptoms may be mild or severe and can progress over time if Plaquenil is not discontinued. It is important to note that other conditions can also cause these symptoms, so it is essential to consult an ophthalmologist for a proper diagnosis if any of these symptoms are experienced.
Plaquenil retinal toxicity may be asymptomatic in some cases, meaning there are no noticeable symptoms. This is why regular eye exams are so important for patients taking Plaquenil. Eye exams can detect early signs of toxicity before symptoms develop, allowing for early intervention to prevent further damage to the retina.
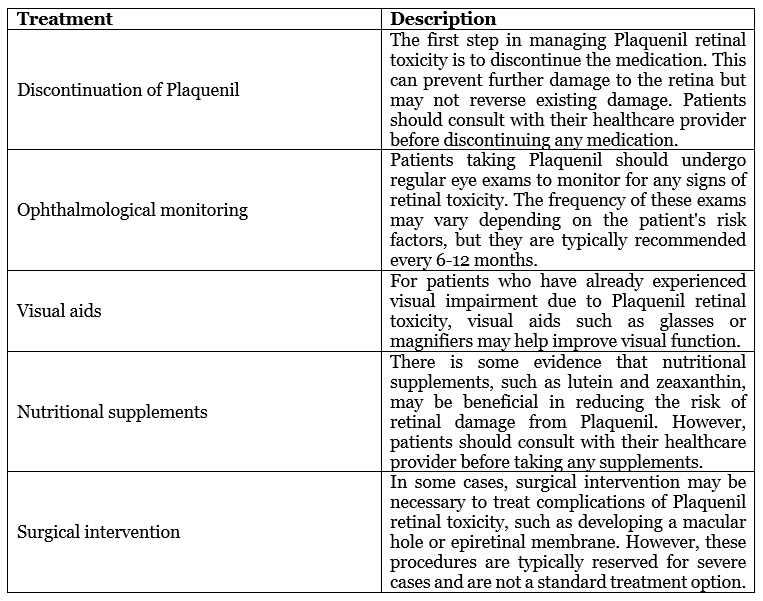
How Is Plaquenil Retinal Toxicity Treated?
The treatment of Plaquenil retinal toxicity depends on the severity of the damage and the stage at which it is detected. Sometimes, the damage may be irreversible, leading to permanent vision loss. Here are some of the ways Plaquenil retinal toxicity is treated:
Can Plaquenil Retinal Toxicity Be Prevented?
Plaquenil retinal toxicity can be prevented or minimized through appropriate monitoring and management. Here are some of the ways Plaquenil retinal toxicity can be prevented:
1. Regular eye exams: Patients taking Plaquenil should undergo regular eye exams to monitor for any signs of retinal toxicity. The frequency of these exams may vary depending on the patient's risk factors, but they are typically recommended every 6-12 months.
2. Dose adjustment: Plaquenil dosage should be adjusted according to the patient's body weight to ensure the dosage does not exceed recommended limits. Dose reduction may be necessary for patients with renal or hepatic impairment.
3. Screening for risk factors: Patients with pre-existing retinal disease or other risk factors for retinal toxicity, such as kidney or liver dysfunction, should be carefully screened before starting Plaquenil therapy.
4. Duration of therapy: Plaquenil therapy should be limited to the shortest duration possible, as prolonged use increases the risk of retinal toxicity.
5. Patient education: Patients taking Plaquenil should be educated about the signs and symptoms of retinal toxicity and instructed to report any visual changes to their healthcare provider.
6. Nutritional supplements: Some studies have suggested that nutritional supplements, such as lutein and zeaxanthin, may help reduce the risk of retinal damage from Plaquenil. However, patients should consult with their healthcare provider before taking any supplements.
Is Plaquenil Retinal Toxicity Reversible?
The reversibility of Plaquenil retinal toxicity depends on the extent and severity of the damage to the retina. Sometimes, the damage may be irreversible, leading to permanent vision loss. Therefore, prevention and early detection are vital in managing Plaquenil retinal toxicity.
However, if retinal toxicity is detected early, discontinuing the medication may prevent further damage to the retina and, in some cases, may allow for some degree of recovery of visual function. In such cases, visual aids such as glasses or magnifiers may help improve visual function. In addition, some patients may benefit from nutritional supplements, such as lutein and zeaxanthin, which may help support retinal health.
It is important to note that the reversibility of Plaquenil retinal toxicity is not guaranteed and can vary from person to person. Regular eye exams and appropriate monitoring of Plaquenil therapy are critical for the early detection of retinal toxicity and for preventing or minimizing the risk of permanent visual impairment. Patients taking Plaquenil should work closely with their healthcare provider to ensure they receive appropriate monitoring and management of their medication therapy.
What Are the Long-Term Effects of Plaquenil Retinal Toxicity?
The long-term effects of Plaquenil retinal toxicity can vary depending on the extent and severity of the damage to the retina. In some cases, the damage may be irreversible, leading to permanent vision loss or blindness. Therefore, prevention and early detection are vital in managing Plaquenil retinal toxicity.
Some of the long-term effects of Plaquenil retinal toxicity may include:
1. Loss of visual acuity: Retinal toxicity from Plaquenil can cause a loss of visual acuity or sharpness of vision. This can affect a person's ability to see clearly and perform daily activities such as reading, driving, and recognizing faces.
2. Loss of visual field: Plaquenil retinal toxicity can cause blind spots or a loss of visual field, affecting a person's ability to perceive their surroundings.
3. Changes in color vision: Plaquenil retinal toxicity can cause changes in color vision, including difficulty distinguishing between colors or seeing colors as faded or washed out.
4. Macular damage: Retinal toxicity from Plaquenil can cause damage to the macula, the central part of the retina responsible for detailed vision. This can affect a person's ability to read, drive, or perform tasks that require good vision.
5. Permanent vision loss: In severe cases, Plaquenil retinal toxicity can lead to permanent vision loss or blindness.
Conclusion
In conclusion, Plaquenil retinal toxicity is a rare but severe side effect of Plaquenil, a medication used to treat autoimmune diseases such as lupus and rheumatoid arthritis. The toxicity is caused by the medication's accumulation in the retina over time, which can damage the cells responsible for detecting light and transmitting visual signals to the brain.
Symptoms of Plaquenil retinal toxicity can include blurred or distorted vision, difficulty seeing in dim light, and changes in color vision. However, the damage may be asymptomatic in some cases, making regular eye exams critical for early detection and intervention.
The risk of Plaquenil retinal toxicity can be minimized through appropriate monitoring and management, including regular eye exams, dose adjustment, screening for risk factors, limiting the duration of therapy, and patient education. Nutritional supplements such as lutein and zeaxanthin may also help reduce the risk of retinal damage.
If retinal toxicity is detected early, discontinuing the medication may prevent further damage to the retina and may allow for some degree of recovery of visual function. However, the damage may be irreversible in some cases, leading to permanent vision loss.
Therefore, patients taking Plaquenil should work closely with their healthcare provider to ensure appropriate monitoring and management of their medication therapy, prevent or minimize the risk of retinal toxicity, and preserve visual function.
Author: Dr. Muhammad Saad, Resident Ophthalmologist at Alshifa Trust Eye Hospital in Rawalpindi, Pakistan
(1).jpg)