Iris Prolapse: A Comprehensive Review of Causes, Diagnosis, and Management
What is Iris Prolapse?
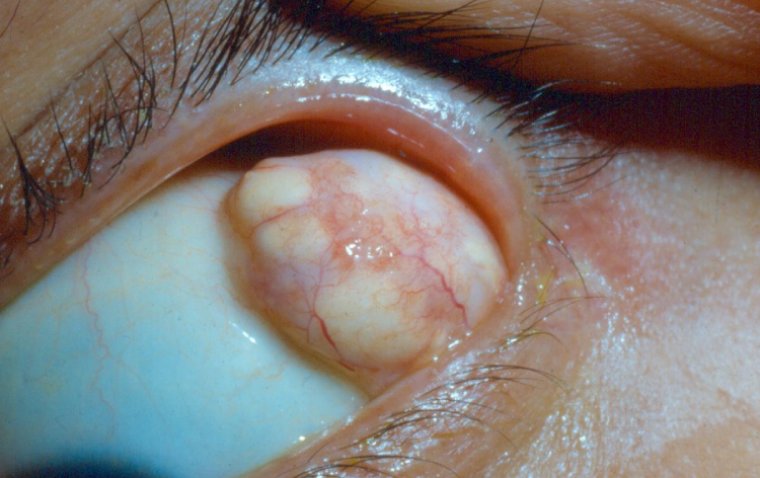
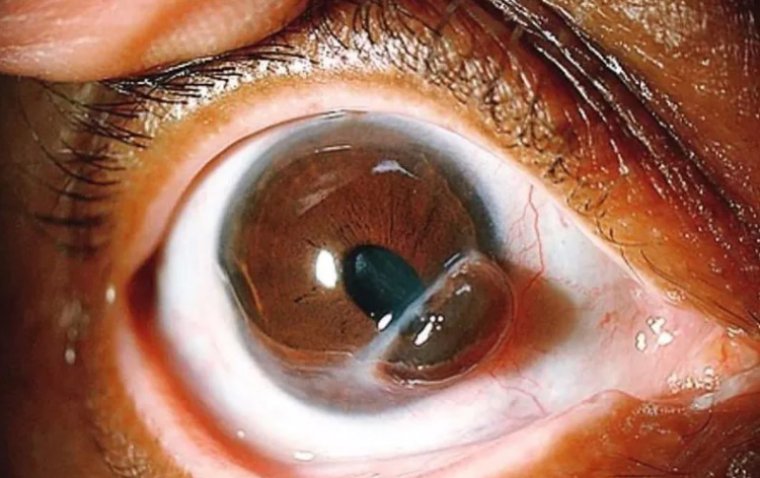
Iris prolapse is a condition wherein the iris, the colored part of the eye responsible for controlling the amount of light entering the eye, protrudes out through a surgical wound or a traumatic wound in the cornea or sclera. This condition often arises as a complication during or after intraocular surgery, or following a traumatic injury to the eye.
The anatomy of the eye is complex, and the iris plays a pivotal role in vision by adjusting the size of the pupil to regulate the amount of light that reaches the retina. It is situated between the cornea (the clear, front surface of the eye) and the lens. The cornea, which is the outermost layer, serves as a barrier protecting the internal structures of the eye, including the iris. The sclera, the white part of the eye, provides structural integrity to the eye.
When there is a breach in the cornea or sclera due to a surgical incision or a traumatic injury, and if the wound is not sealed properly or reopens due to some reason, the iris can prolapse, or herniate, through this opening. This can lead to a range of complications including increased risk of infection, further injury to the iris or other intraocular structures, and potential vision loss if not promptly and properly managed.
Iris prolapse is considered a surgical emergency, and immediate measures should be taken to reposition the iris and close the wound to prevent further complications and preserve the eye's structural integrity and function. The occurrence of iris prolapse underscores the importance of meticulous surgical technique, proper wound closure, and prompt management of ocular trauma.

How Rare is Iris Prolapse?
Iris prolapse is described as an uncommon occurrence, typically arising as a complication during or after intraocular surgery such as cataract surgery, glaucoma surgery, or corneal transplantation. It can also occur due to acute degenerative processes, infections, or penetrating injuries to the eye. In a specific study reviewing a 12-month period, out of 1408 routine manual extracapsular cataract extractions, 29 eyes (2.06%) experienced an iris prolapse.
The rarity of iris prolapse underscores the importance of taking precautions during intraocular surgeries or in situations where the eye might be exposed to traumatic injuries. Though it may be rare, its occurrence is considered a surgical emergency due to its potential impact on vision and the structural integrity of the eye.
Causes of Iris Prolapse
The emergence of iris prolapse is often a result of a combination of factors such as trauma, surgical interventions, and certain underlying medical conditions. Understanding these causative factors is critical for prevention and management. Here’s a breakdown of common causes under the specified subheadings:
1. Trauma: Trauma to the eye can lead to iris prolapse if the integrity of the cornea or sclera is compromised. This can happen due to:
● Penetrating Injuries: Sharp objects or high-speed particles can penetrate the eye, creating a pathway for the iris to prolapse.
● Blunt Force Trauma: Severe blunt force can cause a rupture or tear in the cornea or sclera, predisposing to iris prolapse.
● Chemical Burns: Severe chemical burns can cause extensive damage to the eye's structural integrity leading to complications like iris prolapse.
2. Eye Surgery: Surgical interventions on the eye, particularly intraocular surgeries, can inadvertently cause iris prolapse. Common surgeries associated include:
● Cataract Surgery: Iris prolapse can occur as an intraoperative or postoperative complication.
● Glaucoma Surgery: Procedures to alleviate intraocular pressure may sometimes lead to iris prolapse.
● Corneal Transplantation: Surgical manipulation during corneal transplantation can also cause iris prolapse if the wound is not sealed properly.
3. Underlying Medical Conditions: Certain medical conditions can predispose an individual to iris prolapse, either by weakening the tissues of the eye or by making the eye more susceptible to injury. These include:
● Inflammatory Eye Diseases: Conditions like uveitis can alter the structural integrity of the eye.
● Degenerative Eye Conditions: Diseases leading to degeneration of eye tissues may increase the risk of iris prolapse.
● Infections: Severe infections can lead to a weakened corneal or scleral surface, making the eye more prone to iris prolapse.
Symptoms of Iris Prolapse
The symptoms of iris prolapse can range from subtle to more noticeable, depending on the extent of the prolapse and the underlying cause. Here are the common and less common symptoms associated with iris prolapse:
● Visual Disturbances
● Physical Changes
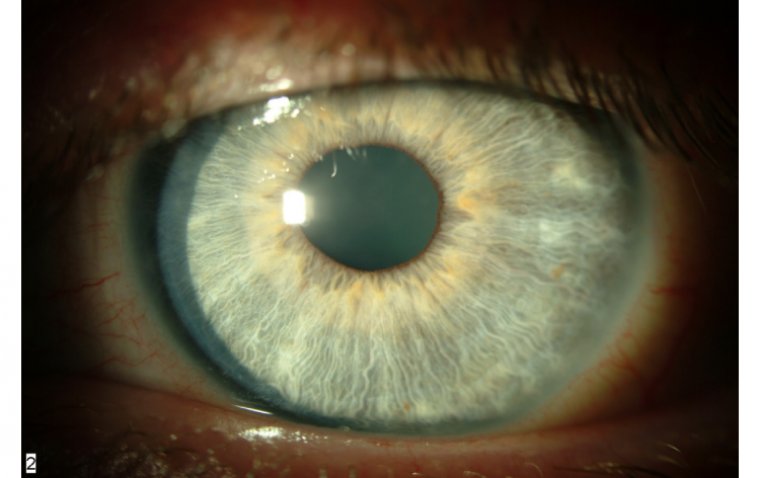
Abnormal Pupil Shape: The pupil may appear distorted or irregular in shape due to the prolapsed iris.
Visible Iris Tissue: In severe cases, iris tissue may be visibly protruding from the wound.
● Discomfort or Pain
● Eye Redness
● Increased Sensitivity
● Tearing: Excessive tearing may occur as a reflex to irritation or foreign body sensation.
● Eye Swelling: In associated inflammatory conditions, the eye may appear swollen.
Less Common Symptoms
● Halos Around Lights: Some individuals may see halos around lights due to refractive changes caused by the prolapsed iris.
● Change in Eye Color: In very rare cases, there might be a change in eye color if there is extensive damage to the iris tissue.
Diagnosis and Medical Evaluation of Iris Prolapse
The diagnosis and medical evaluation of iris prolapse are crucial steps towards understanding the extent of the condition and planning an effective treatment strategy. Here's how the diagnostic process for iris prolapse is typically carried out:
1. Ophthalmologist Examination: An examination by an ophthalmologist is the primary method for diagnosing iris prolapse. The examination may include the following:
2. Slit-Lamp Examination: This is a key diagnostic test where a microscope with a bright light is used to examine the front part of the eye, including the iris, to identify any abnormalities.
3. Pupillary Response Testing: Evaluating the response of the pupil to light can help assess the function of the iris and identify prolapse.
4. Visual Acuity Testing: This test assesses the impact of the iris prolapse on vision.
5. Intraocular Pressure Measurement: Measuring the pressure inside the eye can provide information about the overall health of the eye and identify other potential issues.
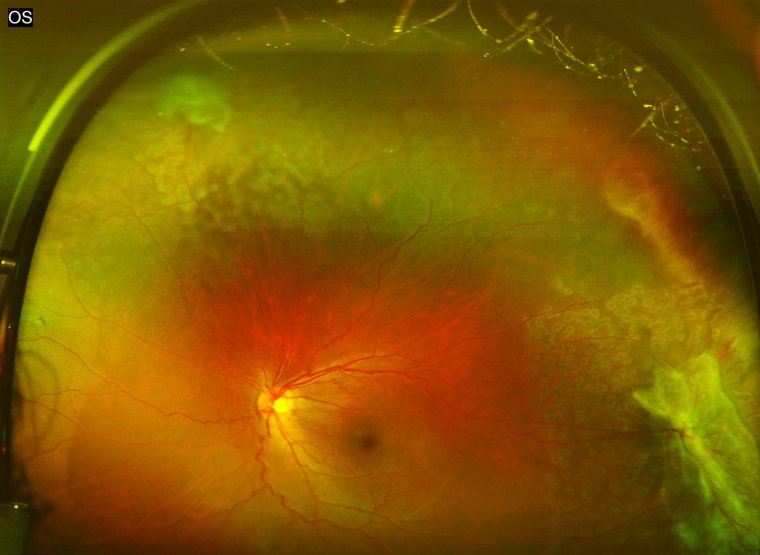
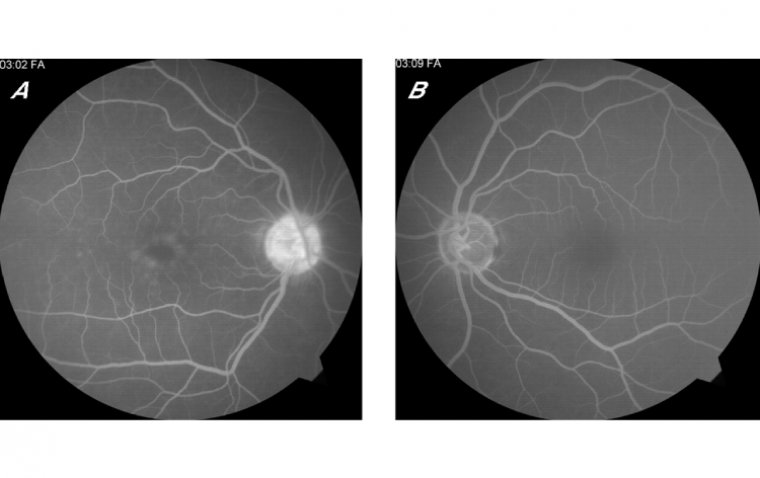
6. Imaging Tests: Imaging tests can provide a more detailed view of the eye's structure and help confirm the diagnosis of iris prolapse:
● Ultrasound Biomicroscopy (UBM): This test uses high-frequency ultrasound to produce detailed images of the front part of the eye, helping to identify iris prolapse and any associated abnormalities.
● Anterior Segment Optical Coherence Tomography (AS-OCT): AS-OCT provides high-resolution images of the anterior segment of the eye, aiding in the diagnosis of iris prolapse.
How Do You Treat Iris Prolapse?
The treatment of iris prolapse necessitates a tailored approach based on the extent of the prolapse, the cause, and the overall health of the eye. Below are the various treatment approaches categorized under surgical interventions, medical management, and conservative measures:
1. Surgical Interventions
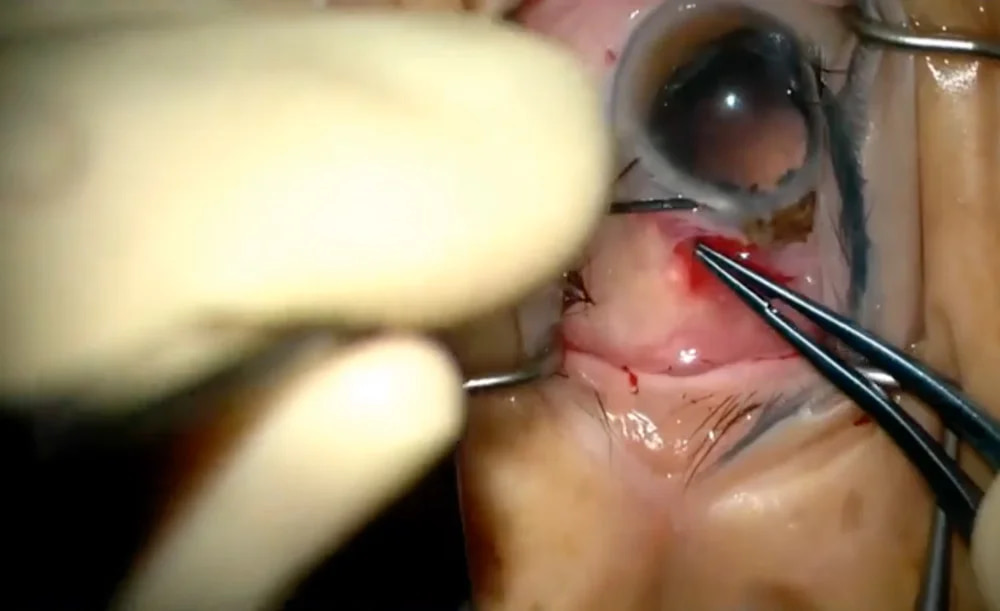
Surgical interventions are often required to manage iris prolapse, particularly if it's caused by trauma or surgical complications:
● Repositioning of the Iris: This is a primary surgical intervention where the prolapsed iris tissue is gently repositioned back into its correct place within the eye.
● Wound Repair and Closure: Ensuring that the wound through which the iris has prolapsed is adequately repaired and sealed to prevent further prolapse.
● Suture Placement: Placing sutures to ensure the stability of the wound and prevent recurrence of prolapse.
● Iridectomy: In cases where the iris tissue is damaged beyond repair, a portion of the iris may be removed to prevent further complications.
2. Medical Management
Medical management often accompanies surgical interventions to treat associated symptoms and prevent infection:
● Topical Antibiotics: To prevent or treat infections at the site of the wound or prolapse.
● Anti-inflammatory Medications: To reduce inflammation and discomfort in the eye.
● Cycloplegic Agents: These agents can help relax the muscles of the eye, reducing discomfort and aiding in the healing process.
3. Conservative Measures
In some minor cases of iris prolapse, conservative management may be considered:
● Observation: Monitoring the eye for any changes or worsening of the condition.
● Eye Shields or Patches: Protecting the eye to prevent further injury and aid in the healing process.
4. Recent Advancements or Emerging Treatments
Recent advancements in ophthalmic surgical techniques and equipment have significantly enhanced the management of iris prolapse:
● Advanced Imaging Technologies: Technologies like Anterior Segment Optical Coherence Tomography (AS-OCT) and Ultrasound Biomicroscopy (UBM) provide better visualization and understanding of the extent of iris prolapse, aiding in more precise surgical interventions.
● Microsurgical Instruments: The development of microsurgical instruments has allowed for more delicate and precise surgical interventions, reducing the risk of further injury and improving outcomes.
Prevention of Iris Prolapse
Preventing iris prolapse is crucial, especially for individuals who have undergone intraocular surgery or have a predisposition due to certain systemic or ocular conditions. Below are preventive measures categorized under post-surgery care, eye protection, and lifestyle changes:
1. Post-Surgery Care: Proper care post-surgery is paramount in preventing complications such as iris prolapse:
● Follow-Up Appointments: Attend all scheduled follow-up appointments to ensure the eye is healing properly and to catch any complications early.
● Medication Adherence: Adhere to prescribed topical medications like antibiotics or anti-inflammatory eye drops to prevent infection and control inflammation.
● Avoid Eye Rubbing: Refrain from rubbing the eye to prevent disrupting the surgical wound, which could lead to iris prolapse.
● Wear Eye Protection: Use a protective shield or eyewear as directed by your ophthalmologist, especially while sleeping, to avoid accidental rubbing or pressure on the eye.
2. Lifestyle Changes: Certain lifestyle modifications can contribute to eye health and reduce the risk of iris prolapse:
● Maintain a Healthy Lifestyle: A balanced diet and regular exercise can contribute to overall health, including eye health.
● Control Systemic Conditions: Manage systemic conditions like diabetes and hypertension that can potentially affect eye health.
3. Regular Eye Check-ups: Regular eye examinations are a cornerstone of preventing ocular complications including iris prolapse:
● Routine Eye Examinations: Regular check-ups with an ophthalmologist can help detect and address any eye abnormalities or potential risks before they lead to serious complications.
● Early Intervention: If you experience any eye discomfort, visual changes, or other eye-related symptoms, seek medical attention promptly for an accurate diagnosis and timely intervention.
Summary
Iris prolapse is a concerning ocular condition wherein the iris protrudes through a wound in the cornea or sclera, often occurring as a complication of eye surgery or trauma. The symptoms vary from visual disturbances, such as blurred or double vision, to physical changes like an abnormal pupil shape or visible iris tissue. It's diagnosed through a thorough examination by an ophthalmologist, supplemented by imaging tests like Ultrasound Biomicroscopy or Anterior Segment Optical Coherence Tomography.
Treatment usually entails surgical interventions to reposition the iris and repair the wound, alongside medical management to prevent infection and reduce inflammation. Preventive measures are fundamental, encompassing diligent post-surgery care, eye protection, lifestyle adjustments, and regular eye check-ups to monitor ocular health.
We strongly encourage readers to seek professional help for any eye-related concerns, as early detection and intervention are critical for preventing and managing complications like iris prolapse. Your eye health is a vital aspect of your overall wellbeing, and timely attention to any issues can significantly improve outcomes. Remember, proactive eye care is a step towards a healthier, clearer vision.
(1).jpg)