An Overview of Horner Syndrome
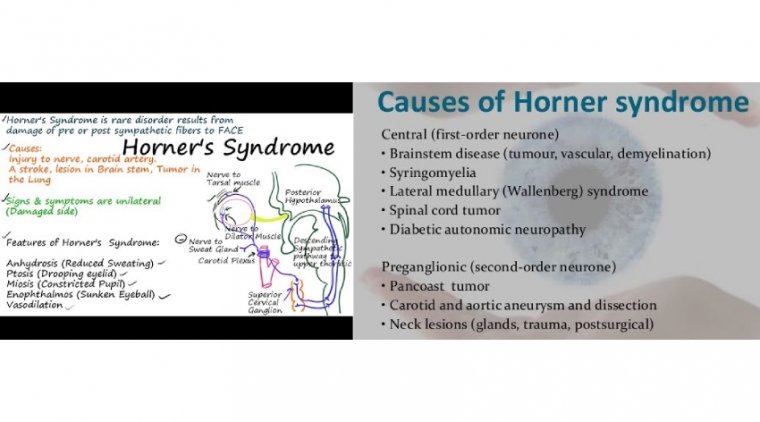
Horner syndrome is a relatively rare disorder characterized by a constricted pupil (miosis), drooping of the upper eyelid (ptosis), absence of sweating of the face (anhidrosis), and sinking of the eyeball into the bony cavity that protects the eye (enophthalmos). These are the four classic signs of the disorder.
The congenital, and more rare, form of Horner syndrome is present at birth but the cause is not known. Most often, Horner syndrome is acquired as a result of some kind of interference with the sympathetic nerves serving the eyes.
The underlying causes can vary enormously, from a snake or insect bite to a neck trauma made by a blunt instrument.
Horner syndrome is a combination of signs and symptoms caused by the disruption of a nerve pathway from the brain to the face and eye on one side of the body.
Typically, Horner syndrome results in a decreased pupil size, a drooping eyelid and decreased sweating on the affected side of your face.
Horner syndrome is the result of another medical problem, such as a stroke, tumor or spinal cord injury. In some cases, no underlying cause can be found. There's no specific treatment for Horner syndrome, but treatment for the underlying cause may restore normal nerve function.
Horner syndrome is also known as Horner-Bernard syndrome or oculosympathetic palsy.
Symptoms
Horner syndrome usually affects only one side of the face. Common signs and symptoms include:
- A persistently small pupil (miosis)
- A notable difference in pupil size between the two eyes (anisocoria)
- Little or delayed opening (dilation) of the affected pupil in dim light
- Drooping of the upper eyelid (ptosis)
- Slight elevation of the lower lid, sometimes called upside-down ptosis
- Sunken appearance to the eye
- Little or no sweating (anhidrosis) either on the entire side of the face or an isolated patch of skin on the affected side
Signs and symptoms, particularly ptosis and anhidrosis, may be subtle and difficult to detect.
Horner syndrome is characterized by ipsilateral ptosis, miosis, and anhidrosis that result from a lesion affecting the oculosympathetic pathway. The syndrome can be benign if idiopathic or iatrogenic but can be predictive of a lifethreatening event such as demyelinating inflammatory, infectious, vascular, or neoplastic problems.
It is important to promptly and accurately diagnose the cause; ophthalmologists are likely to be on the front lines. No definitive information is available about the pathologies associated with Horner syndrome and the incidence rate in US adults is unknown.
Because no US population-based studies of the syndrome had been undertaken, it has been set out to determine its population-based incidence in adults, evaluate the underlying causes and disease manifestations, and investigate the value of imaging in patients with a neurologically isolated Horner syndrome.
Retrospective Review
The investigators conducted a retrospective chart review of all adults diagnosed with Horner syndrome in Olmsted County, Minnesota, using the Rochester Epidemiology Project database between January 1, 2000, and December 31, 2018.
According to this review, the team of inveatigators reviewed the charts for the correct diagnoses and recorded the patient demographic data, presenting signs and symptoms, imaging results, and etiologies and analyzed all of the results.
Of the 736 patients identified in the review of cases, 78 confirmed cases were included in the study; the rest were excluded because of their nonresident status, disease onset outside the study time frame, or miscoded or incorrect diagnoses.
According to the team of investigators, the causes varied widely from those that were benign including idiopathic and surgical causes, cluster headache, and goiter to the neurologically or systemically dangerous causes that included carotid artery dissection, stroke, neoplastic and traumatic causes, varicella zoster, arteriovenous fistula, and fibromuscular dysplasia.
Findings
The median patient age was 57 years, and all patients were Caucasian. The age- and sex-adjusted incidence of Horner syndrome during the study period was 4.24/100,000/year with no difference in gender or over time.
“We did find a significant [P < 0.001] difference across age groups, with older patients having a higher incidence of Horner syndrome,” the researchers pointed out. Three-quarters of cases were diagnosed first by neurologists followed by ophthalmologists, with most diagnosed clinically.
“Interestingly, idiopathic cases were more likely to be confirmed with cocaine or apraclonidine eyedrop testing (P = 0.002), and stroke, surgical, and dangerous causes were more often diagnosed clinically (P = 0.008).
Common Etiologies
The most common etiologies were idiopathic (20 patients, 25.6%), followed by internal carotid artery (ICA) dissection (15 patients, 19.2%), stroke (12 patients, 15.4%), surgical (12 patients, 15.4%), and neoplastic (11.5%).
Analysis of the etiologies indicated that about 56% of cases had a dangerous neurologic or systemic origin, according to investigators.
Compared with other etiologies, the patients with ICA dissections, which were more likely to be diagnosed in younger individuals who were a mean age of 49 years (P = 0.02), were more likely to have pain (P < 0.001), facial paresthesia (P = 0.007), blurred vision (P = 0.04), and photophobia (P < 0.004). Most of the cases with a stroke had a lateral medullary infarction.
Neoplastic Causes
Neoplastic causes included 4 pancoast tumors that affected the oculosympathetic pathway at the lung apex. It was noted that the most common neoplasm was lung cancer.
Moreover, the investigators found that neuroimaging results were surprising in that almost 40% of patients with a neurologically isolated Horner syndrome had a positive finding on computed tomography (CT) or magnetic resonance imaging (MRI).
In isolated Horner Syndrome cases, pain suggested both a dangerous etiology and a positive imaging result, which was driven primarily by patients found to have an ICA dissection.
In this first US population-based study of the incidence of Horner syndrome, the primary take-home points are that 56.4% of cases resulted from a dangerous cause; in previous reports the percentages ranged from 8% to 78%.
Another finding useful in diagnosis is that about 40% of patients with an isolated Horner syndrome had positive CT or MRI findings, which is almost double that reported previously.
Finally, investigators noted that pain reported by patients suggested a dangerous etiology and positive imaging, which in this study was most likely secondary to an ICA dissection.
Ophthalmologists should keep in mind that ICA dissections are likely to occur in younger patients, may look like an isolated syndrome or present with neurologic disease and stroke, are painful, and may cause facial paresthesia, blurred vision, or photophobia compared with other causes.
Ophthalmologists recommend imaging of the oculosympathetic pathway in all cases of Horner syndrome without a clear ethology, even in neurologically isolated cases, particularly when pain is present.
(1).jpg)