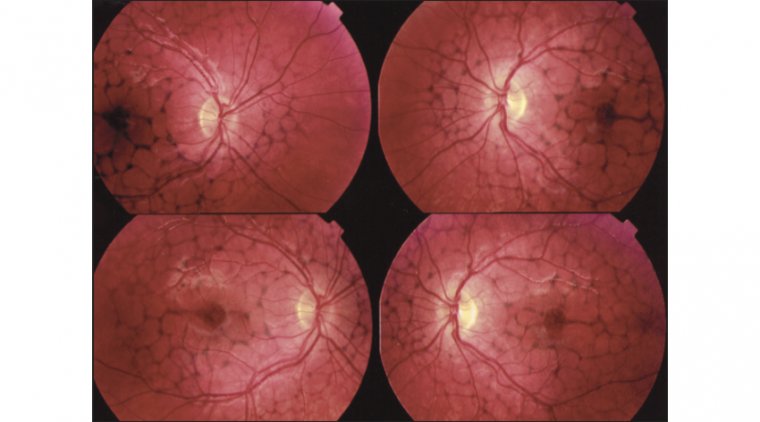
Types and Classification of Retinal Pattern Dystrophies
Retinal pattern dystrophies, as the name implies, are a group of disorders characterized by diverse pigment deposition patterns in the macula's retinal pigment epithelium (RPE). The RPE, located in the retina's outermost layer, is rich in pigment particles, such as melanin and lipofuscin, that prevent light damage. A yellowish, orange, or brown lipofuscin accumulation in the subretinal region characterizes many pattern dystrophies. Typically, these dystrophies are associated with a favorable visual prognosis; however, gradual central vision loss remains a possibility.
How is it inherited?
Mutations cause pattern dystrophies in any of several genes inherited in an autosomal dominant manner. This fact means that a parent with pattern dystrophy has a 50% chance of passing it on to their child, regardless of gender. That child would have one gene causing the disorder and one normal gene in a single pair of genes. For instance, if the father has one gene for pattern dystrophy and one normal gene, but the mother has two normal genes, the mother will always pass on a normal gene from that pair to their offspring. There is a 50/50 probability that the father will give the gene for pattern dystrophy or the normal gene.
However, another condition might arise when an individual carries the disease-causing genetic mutation but does not exhibit the phenotypic condition. This characteristic is non-penetrance. When a gene is non-penetrant, it appears to have skipped a generation. For example, in a family where many members, including a child and grandparent, have pattern dystrophy, the intervening parent with the dominant gene for pattern dystrophy has normal eyesight.
Types of Pattern Dystrophies:
1. Adult-onset foveomacular vitelliform dystrophy: It is the most prevalent kind of pattern dystrophy. It is characterized by bilateral, symmetrical, grayish-yellow, round lesion within macular region. The lesion is typically one-third to one-half the diameter of a disc.
2. Butterfly-shaped pattern dystrophy: It is commonly observed between the second and fifth decades of life. They manifest as yellow and melanin pigmentation in the fovea, typically in a spoke-like or butterfly-wing-like configuration.
3. Reticular dystrophy is usually seen in the 5th decade of life. Clinically, it features a network of pigmented lines and knots in a fish net-like appearance in the RPE. Lesions are up to five-disc diameters from the macula and typically fade with age.
4. Multifocal Pattern Dystrophy includes multiple irregular white-yellow specks dispersed across the macula, comparable to the flecks in Stargardt disease.
5. Fundus Pulverulentus: Fundus pulverulentus is characterized by a granular appearance and punctiform mottling of the retinal pigment epithelium (RPE) within the macula. Due to the RPE mottling, Fundus pulverulentus might be confused for age-related macular degeneration; however, OCT imaging can help differentiate the two.
Symptoms
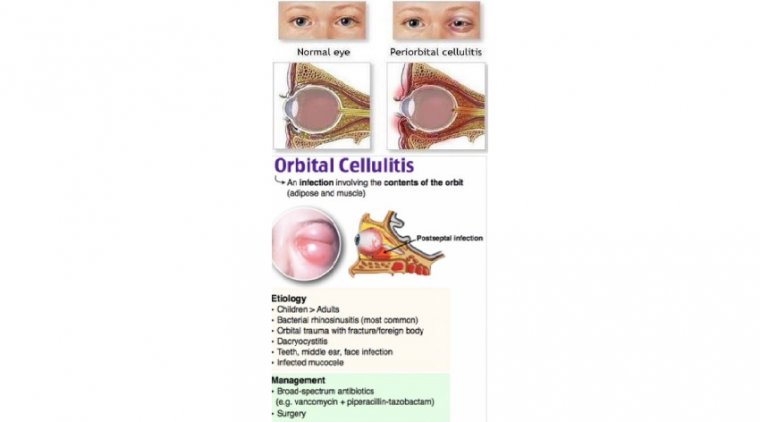
Due to the benign nature of the symptoms, pattern dystrophies are frequently detected during routine or unrelated eye exams. In rare circumstances, patients may experience substantial vision loss caused by complications, such as choroidal neovascularization.
The following are the typical symptoms of Pattern Dystrophies:
- Metamorphosis
- Decreased Visual Acuity
The onset of these symptoms is in early adulthood or later, but many individuals are asymptomatic.
Diagnosis & Treatment options
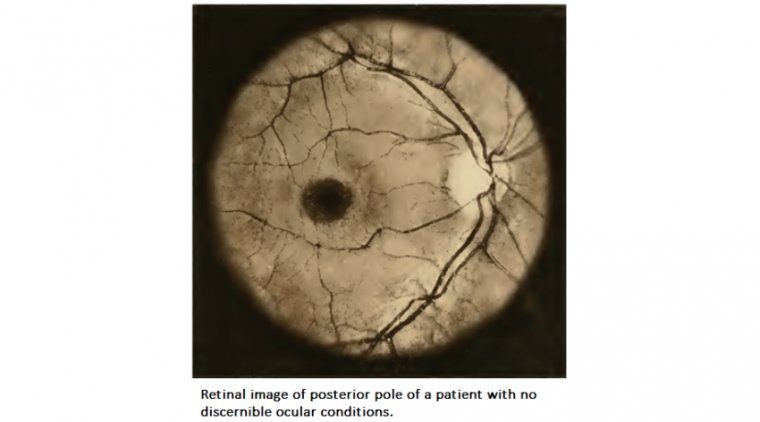
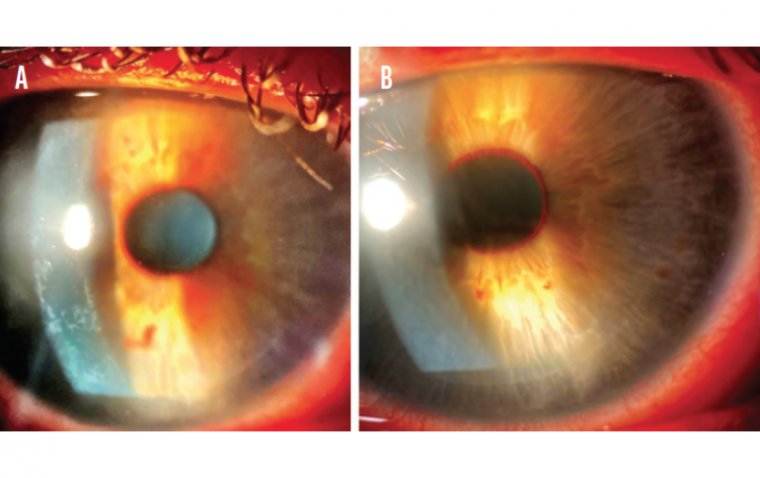
Primarily, Pattern dystrophy is diagnosed clinically through dilated fundus examination. The pattern's nature and description determine the sort of pattern dystrophy a patient has.
Fluorescein angiography (FA), fundus autofluorescence (FAF), electrooculography (EOG), and electroretinography (ERG) can provide additional data to stage and characterize the pattern.
Currently, there is no treatment supported by evidence for Pattern dystrophies. Despite that, they often have a favorable visual prognosis. However, vision loss can be more rapid in some patients due to secondary problems such as choroidal neovascularization and retinal holes, which require anti-VEGF injections and surgical hole repair.
Role of Low-Vision Aid
Low vision therapy is most effective at mitigating the impact of visual loss on a patient's life. Patients will most likely benefit from single-vision reading glasses and may need monocular occlusion for reading. Patients can utilize monocular telescopes for long-range observation. Optivisors can improve visual performance for people who want to be able to do household repairs. A pair of bifocal spectacles with an add in the distance portion for intermediate vision and an add in the bifocal part for near work can be used for close work and intermediate vision.
Dr. Muhammad Saad
Resident Ophthalmologist-Cornea Department
Al-Shifa Trust Eye Hospital
Rawalpindi, Pakistan
(1).jpg)