How to Slow The Myopia In Children With Contact Lenses
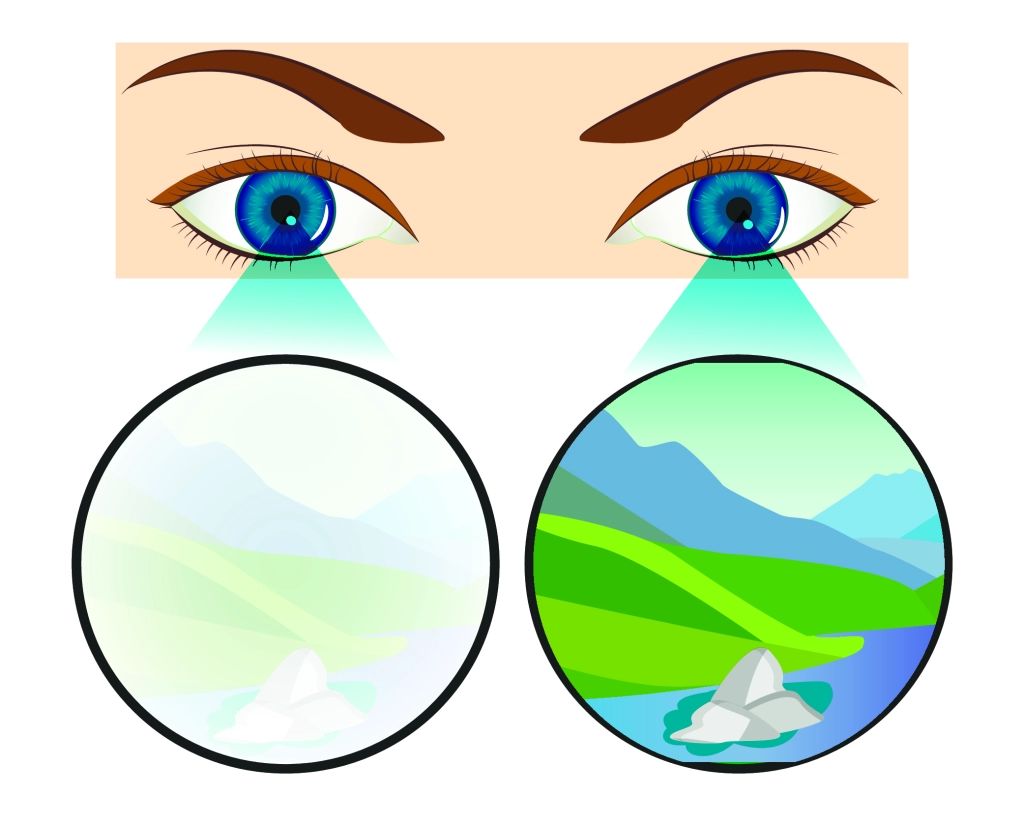
Myopia, or short-sightedness, is one of the most common eye health issues in children and means that they can’t see objects that are far away, causing their vision to blur.
Symptoms usually appear between the ages of 8 and 12 and can get progressively worse over time, with most children quickly becoming reliant on glasses to see clearly into the distance.
According to a 2019 study in the Investigative Ophthalmology and Visual Sciences journal, more than 32% of the world’s population suffers from myopia, with that figure estimated to rise to 50% by 2050.
Are you prescribing contact lenses for myopia management? We ask this question at the start of every myopia management lecture we deliver. Over the past two years, we have gone from having audiences with no hands raised to now having audiences with upwards of 20 percent of the attendees raising their hands.
While a number of clinical trials are still ongoing, evidence continues to mount regarding the effectiveness and safety of soft contact lens (CL)-based myopia management, and because of this, we expect the number of eye care providers prescribing myopia management to increase.
Myopia is a complex trait influenced by a number of environmental and genetic factors, and the mechanisms underlying onset and progression are not fully understood.
Although there is a great deal to learn about the mechanisms of myopia and why individuals respond differently to different stimuli and treatments, some behavioral, pharmaceutical and optical strategies already show promise in clinical trials in combating myopia—many of which can be incorporated into current day practice.
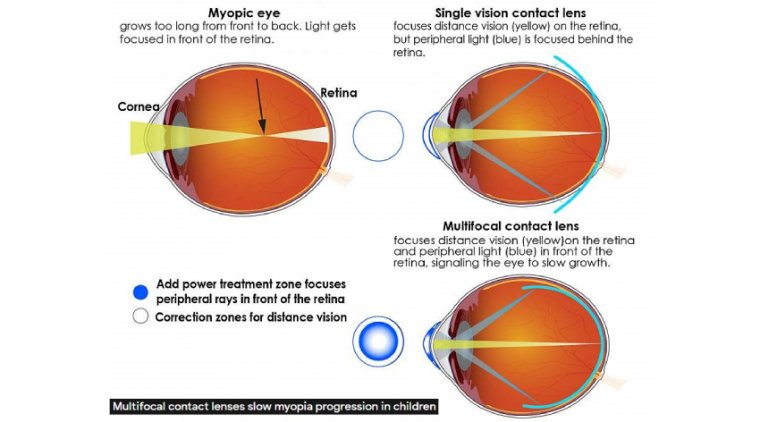
Contact lenses used for myopia control can be either bifocal or multifocal soft contact lenses, as well as the rigid contact lens designs used in orthokeratology.
Investigators have proposed several mechanisms to explain their myopia control effect, including: contact lenses correct or reduce accommodative lag, which is considered a stimulus for eye elongation; they reduce the peripheral retinal defocus, which is considered to increase the risk of eye elongation by shifting the image closer to the retina; and the lenses impose myopic defocus across areas of the retina, which is considered to inhibit eye growth.
Myopia is a nearly silent public health crisis growing in prevalence worldwide year upon year. Preventing high myopia with myopia management is becoming the standard of care for children and adolescents discovered to have myopia.
Center-distance MF contact lenses, including soft lenses and GP lenses, can provide myopia control in children. Similar to daily wear contact lenses, ortho-k lenses are also capable of generating the retinal defocus stimulus that retards myopia progression.
Atropine by itself, or potentially in combination with myopia control contact lenses, may also be efficacious.
With so many options already available and more forthcoming, it is incumbent upon eyecare practitioners to offer these treatment options to children whom they have diagnosed with myopia.
Doing so is likely to improve their quality of life and also decreases their likelihood of developing detrimental visual complications decades in advance.
Myopia is the most common refractive error, affecting 30% of adolescents and young adults worldwide; between 2000 and 2050, myopia’s worldwide prevalence is projected to increase from 23% to 54%.
The prevalence of high myopia is expected to increase from 3% to 10%. Higher increases in prevalence are found among East Asian populations.
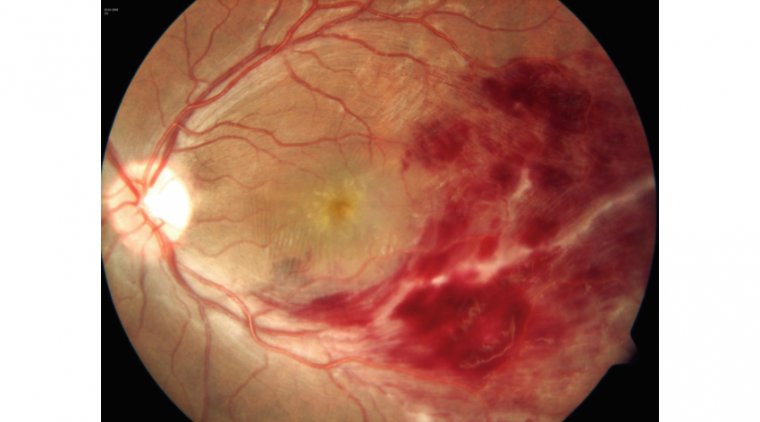
Myopia is an abnormal process that disrupts emmetropization. Longer axial length in myopic eyes, especially in high myopes (–6.00D or greater or axial length of 26mm or greater), increases the risk for developing sight-threatening complications such as chorioretinal atrophy, foveoschisis, rhegmatogenous retinal detachment, myopic maculopathy, glaucoma, and cataract.
Progressive myopia is a serious ocular condition, and the younger that children are when diagnosed with myopia, the greater the risk they have for developing high myopia. The burden associated with visual impairment from myopia complications elevates the need to implement myopia management strategies as soon as possible in children.
Typical myopia control strategies include contact lens options, such as soft multifocal (MF) lenses and orthokeratology (ortho-k), and low-dose atropine. The following discussion focuses on contact lens options, including specialty lens options, for myopia control, how to fit these lenses, and follow-up care.
CONTACT LENS OPTIONS FOR MYOPIA CONTROL
Focusing light in front of the retina effectively retards axial length growth in humans. Contact lenses for myopia control function by simultaneously focusing light onto—and in front of—the retina.
This provides acute vision for daily activities and also a defocus stimulus that slows axial length growth. Reducing myopia progression by at least 40% is considered clinically meaningful.
On average, soft MF contact lenses with center-distance-design optics slow myopia progression by 46%. Corneal reshaping with ortho-k lenses likely employs the same mechanism for slowing myopia progression.
As an alternative to typical soft MF and ortho-k designs, daytime-wear GP MF options (such as corneal and scleral GP MF and hybrid lenses) may be prescribed for myopia management. These alternative lens options may best suit higher amounts of refractive error and astigmatism.
WHEN AND WHOM TO START FITTING
Two crucial questions to consider are the timing of myopia management implementation and which children to treat. Indeed, age is the most critical factor that influences myopia progression.
The younger that children become myopic, the faster myopia progresses, thereby increasing the likelihood of developing high myopia. For example, in the Correction of Myopia Evaluation Trial (COMET) study, children 6 or 7 years old progressed twice as fast as the children who were 11 years of age.
Children from East Asian countries experience a higher rate of myopia progression compared to Western children. However, it is less clear whether children of Asian descent in North America progress faster compared to their non-Asian counterparts.
For example, the COMET study reported that Asian-American children progressed faster compared to African-American children but no faster than Hispanic and Caucasian children.
In contrast, another study by Cheng et al demonstrated an increased rate of axial length progression in Asian-American children consistent with East Asian counterparts.
Given the available evidence, there is a rationale for preferentially initiating myopia control in ethnically Asian children.
Parental history of myopia is also a factor when potentially initiating myopia control. Children of myopic parents are at increased risk of developing myopia.
Priority for initiating myopia management strategies, including fitting contact lenses for myopia control, should be given to children who are young, of Asian background, and/or who have a history of parental myopia.
As nearly all young myopes progress, myopia management strategies should be offered to myopic school-aged children. While low-to-moderate amounts of myopia in children are well understood, there is minimal research on more severe, pathological, early-onset high myopia.
Young children usually are hyperopic. If myopia onsets earlier than 5 years of age, consider further evaluation including genetic testing. Early myopia may be associated with systemic conditions such as Marfan syndrome or Stickler syndrome.
Myopia control strategies can be offered to those who have early-onset high myopia. However, the parents must be educated that their child’s response to treatment may not be as effective.
FITTING SOFT LENSES
All soft MF lenses validated for myopia control are center distance in design. Originally prescribed for presbyopia, both aspheric and concentric-ring-design MF lenses can be prescribed with center-distance optics for myopia control.
Standard aspheric center-distance MF lenses consist of a central distance zone that gradually transitions into an intermediary add power before extending into the full near add power at the end of the optic zone.
In contrast, concentric-ring-design MF lenses have a central distance zone surrounded by alternating rings of near and distance power that extend throughout the remainder of the optic zone. Interestingly, the concentric-ring MF potentially creates optics that equally balance between distance and near correction with varying pupil size.
The only U.S. Food and Drug Administration (FDA)-approved contact lens indicated to slow the progression of nearsightedness is based on concentric-ring-design MF optics.
All other lens designs that create simultaneous center-distance MF optics may be prescribed for retarding myopia progression; however, this is considered an off-label use in the United States.
As the goal is to decrease the progression of myopia, prescribing soft MF contact lenses in children is different from prescribing them to presbyopes. In addition to the axial length and refractive error, other factors such as the add power and pupil size need to be considered for prescribing lenses that create effective myopia control.
Myopia control with soft MF contact lenses depends on focusing some light in front of the retina; this slows growth in axial length, thereby retarding myopia progression.
Clinically, it makes sense to infer that higher add powers may provide better myopia control, because they can focus light further in front of the retina compared to lower add powers.
To examine this hypothesis, the Bifocal Lenses In Nearsighted Kids (BLINK) study randomly assigned children to wear either commercially available single-vision contact lenses or medium- (+1.50D) or high- (+2.50D) add-power soft MF contact lenses for three years.
This study demonstrated that treatment with high-add-power MF contact lenses reduced the rate of myopia progression more effectively compared to either the medium-add-power MF or the single-vision contact lenses.
Therefore, when prescribing soft MF lenses for myopia control, consider fitting children in higher add powers to best decrease myopia progression.
MF optics are associated with increased total aberrations, including higher-order aberrations, which disturb visual quality, especially in low-light settings.
These visual disturbances increase with increasing add power. Nevertheless, most children easily adapt to MF optics and report good-quality visual stereo acuity. If patients are bothered visually, consider prescribing –0.25D or –0.50D more distance power to relieve their symptoms.
As mentioned above, defocused retinal images induced by hyperopic blur retard axial length growth. Prescribing MF lenses that create myopic blur within the visual axis will, therefore, be most effective in retarding myopia progression.
To maximize the myopia control effect, consider pupil size when prescribing soft MF lenses for myopia control. Ensure that the near-add-power optic is within the pupillary visual axis during normal lighting conditions.
To assess this, take a corneal topography map over the MF soft lens on the eye to examine the centration and size of the multifocal optic. This can be compared to the photopic pupil size measured under normal lighting during the baseline evaluation.
Assessing the fit of soft MF lenses on children is typical to assessing any soft lens on the eye. Ensure that the lens has good coverage, movement, and on-eye stability. The average corneal diameter and sim curvature are approximately 11.80mm and 43.00D, respectively; however, this may vary from child to child.
Custom soft MF lenses are available in variable diameters and base curvatures to fit children who fall outside of these normative parameters.
Fitting children who have astigmatism in soft lenses for myopia control can be accomplished by adding a toric prescription to the MF lens. Troubleshooting visual complaints in soft MF toric lenses can be challenging, because it may not be apparent whether the disturbance in vision is coming from the MF optics or from uncorrected astigmatism.
A stepwise approach to fitting toric MF lenses in children would start with fitting a single-vision distance toric lens first. Once it is established that the lens fits well and that the patient has good quality of vision, order the same lens with MF optics.
FITTING ORTHOKERATOLOGY
Overnight ortho-k received FDA approval to correct myopia in 2002. For this purpose, ortho-k is highly effective. Additionally, myopia management with ortho-k reduces myopia progression by 40% to 60% compared to spectacle correction alone.
It is worth noting, however, that prescribing ortho-k lenses for myopia management is considered an off-label use. This may be disconcerting to some parents, but the effectiveness of ortho-k is nonetheless well-established for myopia management.
Modern ortho-k lenses have a reverse geometry design. The primary measurements needed to order these lenses empirically include a manifest refraction, horizontal visible iris diameter (HVID), and corneal topography.
Some lenses are designed from flat keratometry (flat K) measurements, although custom lens design software may require eccentricity and apical radius of curvature measurements. These lenses are larger in overall diameter—often 90% to 95% of the total HVID.
The back surface of an ortho-k lens has a minimum of four curves; however, some designs that correct higher amounts of myopia can have up to six curves.
Ortho-k lenses for myopia management should center well, and the lens should display an adequate fluorescein pattern of central alignment under the back-optic zone radius (BOZR), clearance throughout the entire reverse zone, and proper landing throughout the alignment zone.
The lens should also move well and have adequate clearance under the peripheral zone to maintain good tear exchange
Topographically, after the lens is removed, there should be a classic bull’s-eye pattern of an even, flattened treatment zone and a steepened reverse curve zone centered within the pupillary circumference.
This proper centration of the reverse zone allows for peripheral defocus to be generated inside the pupil, thereby maximizing the myopia control effect. Adjacent to the steepened reverse zone, a more pronounced flattened area 360º around should be visible.
This zone represents adequate positioning and applanation of the alignment curve within the peripheral cornea. With the ortho-k lens removed, patients should be able to achieve their best-corrected visual acuity.
Any residual myopia may be corrected with regular distance spectacles during the day. As the cornea remains molded from the ortho-k treatment, the peripheral retinal defocus responsible for myopia control remains in effect even with over spectacles to correct residual myopia.
After lens removal, the cornea should be clear with no signs of punctate epithelial staining, negative staining, or stromal opacities. Any of these findings indicates mechanical contact of the lens with the corneal surface and/or corneal hypoxia. Additionally, patients should report good, functional vision throughout the day.
Spherical ortho-k lenses on highly astigmatic corneas usually result in poor centration, leading to induced irregular astigmatism, glare, and poor visual outcome. Limbus-to-limbus, against-the-rule, and larger astigmatic errors are not well corrected with spherical lens designs.
Therefore, toric ortho-k lenses are indicated to achieve effective myopia treatment and visual correction in astigmatic patients. Corneal topography is used to determine whether a toric design is needed.
A sagittal height difference between the flat and steep corneal meridians of 30 microns or greater at the landing chord length of the alignment curve suggests that the treatment may benefit from adding lens toricity.
LENS DESIGNS WITH GP OPTICS
In general, daytime GP lenses offer sharp optics and are a great option, especially in highly astigmatic children. Similar to soft lens designs, multifocal optics can be added to the surface of a GP lens and are especially useful for myopia control in highly astigmatic myopic children.
Although this lens type offers improved optical quality over spectacles and soft lenses in highly astigmatic children, there is the perception that it is difficult to adapt to GP lenses. Nonetheless, 80% of children become accustomed to corneal GP lenses, which is the same adaptation rate as for adults.
Additionally, with the availability of hybrid and scleral GP lenses as well as improved designs of newer corneal lenses, initial lens awareness is now much less of a concern. Consider prescribing daytime GP multifocal lenses for children who have more than 2.50D of corneal astigmatism.
Corneal GPs Bitoric corneal GP lenses can be prescribed to correct myopia and astigmatism in children. These lenses can easily be ordered empirically through a contact lens laboratory using keratometry values and cycloplegic refraction.
Similar to prescribing soft toric MF lenses, GP bitoric lenses must be well centered and have good on-eye stability. After achieving a good fit, the front-surface center-distance MF optics for myopia control can be added.
Hybrid Lenses Hybrid lenses are comprised of a GP center surrounded by a soft-lens-material skirt. The soft skirt of the hybrid lens keeps the GP lens well centered and stable on the eye.
This makes hybrid lenses a good choice for highly astigmatic myopic children who have active lifestyles and for whom lens dislodgment may be a concern during their activities.
Center-distance MF optics are available on hybrid lenses for myopia control. As these lenses generally center well, the MF optics can be added on the front of the lens during empirical ordering.
Scleral Lenses Typically fitted in adult patients, scleral lenses are indicated in pediatric cases when it is difficult to achieve an acceptable fit or sufficient vision with other lenses, such as in cases of high myopia and astigmatism.
In such cases, MF center-distance optics may be placed on the surface of a scleral lens for myopia control. The underlying tear lens in a traditional prolate-design scleral lens generates a more myopic prescription on the eye.
However, an oblate reverse geometry design can be created in which the base curve is significantly flattened, thus creating a more plus prescription on the eye.
Therefore, a scleral lens that has a hyperopic or low-minus prescription with center-distance MF optics can be created for a young high myope needing myopia control.
COMBINATION TREATMENTS
In addition to contact lenses, there is a pharmacological approach to myopia management using the antimuscarinic agent atropine. The mechanisms of both contact lenses and atropine in myopia management are not entirely understood.
Different mechanisms may be involved, and a synergistic effect could exist if contact lenses are combined with low-dose atropine.
Long-term studies are underway evaluating low-dose atropine combined with bifocal soft contact lenses and with ortho-k in retarding the progression of myopia.
Regardless of whether there are combination effects, an effective strategy may be to start young children on atropine and then continue with contact lenses as soon as they are able to wear them.
FOLLOW-UP CARE AND DISCONTINUATION
After prescribing myopia control contact lenses, employ follow-up care every six months to monitor the effectiveness of treatment. Cycloplegic refraction and axial length measurements are the standard of care to monitor the effectiveness of myopia control daytime use contact lenses.
Because ortho-k corrects refractive error by reshaping the cornea, refractive error cannot be used as an effective treatment indicator. If ortho-k is chosen, axial length is the most accurate measurement for the evaluation of myopia progression.
Based on currently available data, every 1.00D of change in refractive error corresponds to a 0.28mm increase in axial length in children ages 6 to 7 years and to a 0.32mm increase in axial length in children ages 12 to 13 years.
There is evidence for accelerated myopia progression or rebound following the cessation of some treatments. For example, following discontinuation of 1% atropine, myopia progressed at twice the normal rate, but less acceleration occurred after discontinuation of treatment with lower atropine concentrations.
Interestingly, two randomized clinical trials showed that no acceleration occurred when one year of treatment with progressive-addition spectacles or MF soft lenses was followed by one year of their discontinuation.
With this in mind, clinicians should be aware of the potential for accelerated progression once myopia control is discontinued and should monitor patients closely.
CONTACT LENS RISKS IN CHILDREN
As they have a longer time to live with potential visual consequences, contact lens safety in children is a concern. Microbial keratitis (MK) is the most severe and sight-threatening complication of all lens-related adverse events.
Thankfully, the risk of MK associated with soft lens wear in children ages 8 to 12 years is no higher than in adults and may be substantially lower. MK is rare in soft daily disposable lens wearers (around 2 per 10,000 patient-years of wear).
This risk for MK, specifically Acanthamoeba keratitis (AK), may be higher in overnight ortho-k wearers in comparison to daily soft lens wearers.
Increased risk factors for AK in overnight ortho-k wear include rinsing and/or storing lenses in tap water. It is critical to educate patients about the hazard that tap water poses and to demonstrate the correct care of their lenses.
(1).jpg)