Hypertensive Retinopathy: Causes, Symptoms, and Treatment
What is Hypertensive Retinopathy?
Hypertensive retinopathy is a condition that affects the blood vessels in the eyes and is directly linked to uncontrolled high blood pressure. This condition is a critical example of how hypertension can impact various organs, including the eyes.
In this article, we will delve into the causes, symptoms, stages, diagnosis, treatment, and prevention of hypertensive retinopathy, highlighting the importance of managing blood pressure for both overall health and eye well-being.
What Causes Hypertensive Retinopathy?
Hypertensive retinopathy is a direct consequence of uncontrolled hypertension, where high blood pressure strains the delicate blood vessels within the retina. This strain causes changes in the blood vessel walls, leading to retinal damage. Common risk factors for hypertensive retinopathy include:
● Long-term or severe high blood pressure.
● Poorly managed hypertension.
● Preexisting medical conditions, such as diabetes.
Symptoms of Hypertensive Retinopathy
Detecting hypertensive retinopathy in its early stages is crucial for effective management. Symptoms may vary in severity and can include:
● Visual Changes: Blurred vision, reduced visual acuity, and vision disturbances.
● Headaches: Particularly those that affect vision or are accompanied by eye pain.
● Floaters: Dark spots or floaters in the field of vision.
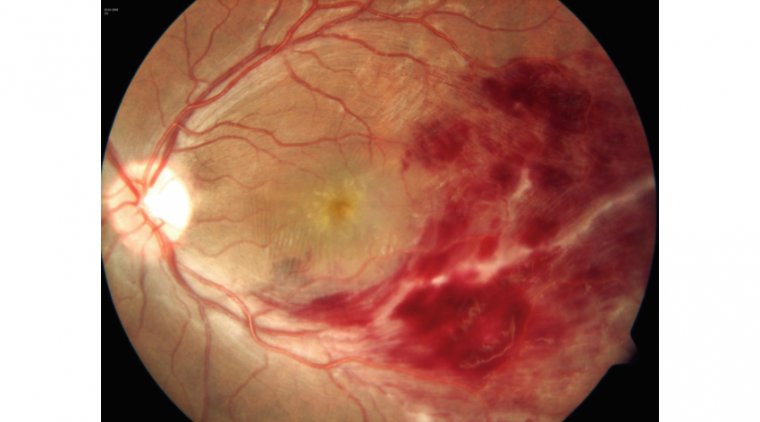
● Hemorrhages: Bleeding within the retina, visible as small, dark spots on the eye's surface.
● Loss of Vision: In severe cases, vision loss may occur.
Four Stages of Hypertensive Retinopathy
Hypertensive retinopathy is classified into several stages, ranging from mild to severe. The stages are indicative of the level of retinal damage and the potential impact on vision:
1. Mild Hypertensive Retinopathy: Mild narrowing of the blood vessels.
2. Moderate Hypertensive Retinopathy: Increased narrowing, along with signs of retinal damage.
3. Severe Hypertensive Retinopathy: Extensive narrowing and severe retinal damage.
4. Malignant Hypertensive Retinopathy: The most severe stage, involving swelling of the optic nerve and potential vision loss.

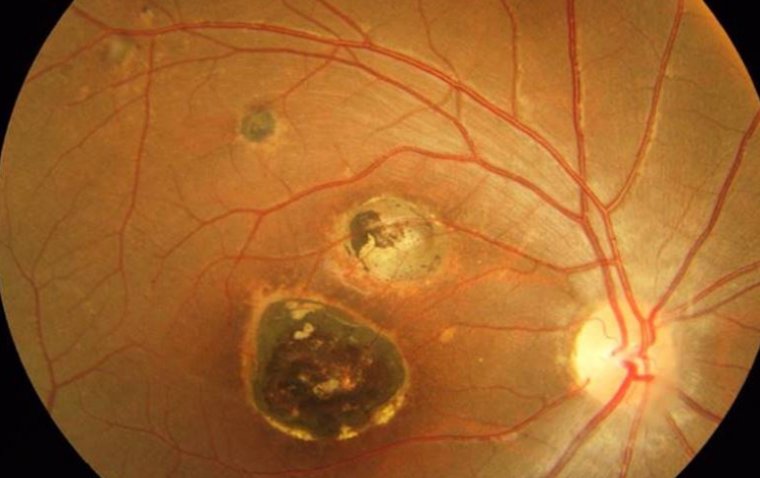
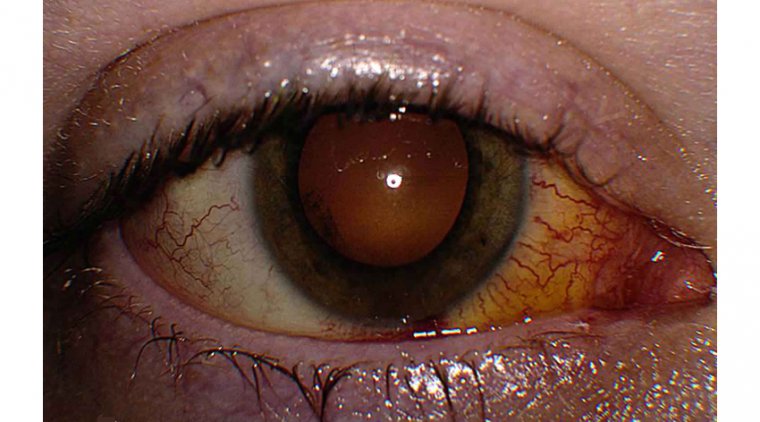
Clinical picture: Hypertensive retinopathy
How to Diagnose Hypertensive Retinopathy
Ophthalmologists typically diagnose hypertensive retinopathy during a comprehensive eye examination. The following diagnostic tools and measures are employed:
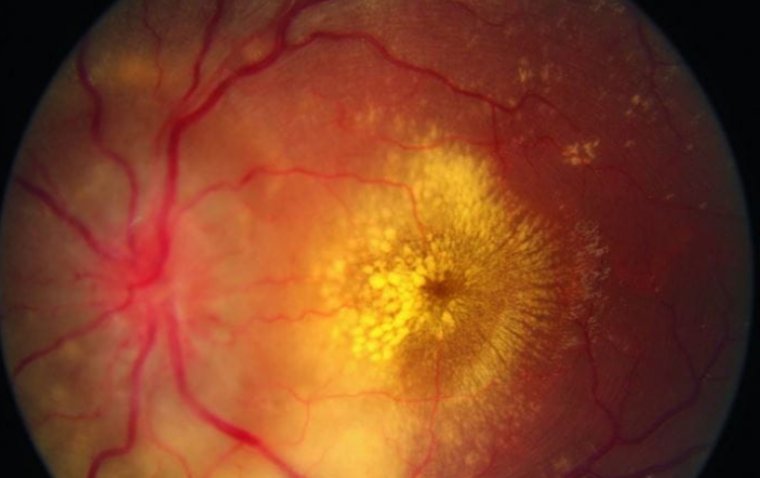
Ophthalmoscopy: A direct examination of the retina to detect changes in blood vessels.
Fundus Photography: Capturing images of the retina to document retinal damage.
Blood Pressure Measurement: Assessing blood pressure levels to confirm hypertension.
Hypertensive Retinopathy vs Diabetic Retinopathy
Hypertensive retinopathy and diabetic retinopathy are both conditions that affect the retina, but they have distinct differences. Hypertensive retinopathy is primarily a consequence of uncontrolled high blood pressure, which causes damage to the blood vessels in the retina. It typically presents as narrowed blood vessels, retinal hemorrhages, and, in severe cases, vision disturbances.
On the other hand, diabetic retinopathy is a complication of diabetes and results from prolonged high blood sugar levels. It manifests as damage to the blood vessels in the retina, leading to the formation of new, abnormal blood vessels, retinal swelling (macular edema), and potential vision loss. While both conditions emphasize the importance of early detection and management, their causes, risk factors, and treatments are distinct, making it crucial to differentiate between the two in clinical practice.
How is Hypertensive Retinopathy Treated?
Hypertensive retinopathy necessitates a multifaceted approach that involves both the management of high blood pressure and the treatment of retinal damage. The choice of treatment depends on the severity of the condition and the specific retinal changes observed. Here are the key treatment approaches:
1. Blood Pressure Control: Controlling high blood pressure is the cornerstone of treating hypertensive retinopathy. This involves medications prescribed by a healthcare provider, as well as lifestyle modifications. Medications may include angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), diuretics, or other antihypertensive drugs. Lifestyle changes, such as adopting a heart-healthy diet, engaging in regular exercise, reducing sodium intake, and avoiding smoking and excessive alcohol consumption, are also crucial in effectively managing blood pressure.
2. Laser Photocoagulation: In cases where retinal hemorrhages or microaneurysms are present, laser photocoagulation may be recommended. This procedure employs a focused laser beam to seal or cauterize the abnormal blood vessels, preventing further bleeding and damage to the retina. It is especially beneficial in cases of macular edema, where swelling of the macula can lead to central vision impairment.
3. Vitrectomy: In severe cases of hypertensive retinopathy with significant bleeding within the eye, a surgical procedure known as vitrectomy may be necessary. During vitrectomy, the vitreous humor (the gel-like substance within the eye) is removed, and any blood or scar tissue that is obscuring vision is carefully extracted. This procedure is typically reserved for advanced cases of hypertensive retinopathy with severe visual impairment.
4. Anti-VEGF Injections: In some instances, individuals with hypertensive retinopathy may develop abnormal blood vessel growth within the retina. In such cases, anti-VEGF (vascular endothelial growth factor) injections may be administered. Anti-VEGF medications work to inhibit the growth of these abnormal blood vessels, reducing the risk of complications and preserving vision.
It's important to note that the choice of treatment depends on the individual's specific condition and its severity. Healthcare professionals, particularly ophthalmologists, will assess the extent of retinal damage and tailor the treatment plan to address the unique needs of each patient.
Prevention and Management of Hypertensive Retinopathy
Preventing hypertensive retinopathy involves proactive blood pressure management and overall eye health maintenance. Key steps include:
● Regular blood pressure monitoring and control.
● Adopting a heart-healthy lifestyle: a balanced diet, regular exercise, and avoiding smoking and excessive alcohol.
● Routine eye exams to detect early signs of hypertensive retinopathy.
Can Hypertensive Retinopathy Lead to Permanent Vision Loss?
Untreated hypertensive retinopathy carries the potential for severe complications, including retinal detachment, where the delicate retina becomes detached from the underlying tissue, leading to significant vision impairment. Additionally, it can result in optic nerve damage, a condition that may lead to irreversible vision loss.
Moreover, individuals with uncontrolled hypertensive retinopathy may experience macular edema, characterized by swelling of the macula, the central part of the retina responsible for sharp vision. Macular edema can profoundly affect central vision, diminishing the ability to see fine details and causing distortions in one's sight. Early detection and effective management of hypertensive retinopathy are critical in preventing these debilitating complications and preserving vision.
Summary
Hypertensive retinopathy serves as a clear example of the far-reaching impact of uncontrolled high blood pressure on various organs, including the eyes. Recognizing the symptoms, diagnosing the condition early, and effectively managing blood pressure are crucial steps to prevent or mitigate the effects of hypertensive retinopathy. By taking these steps, individuals can safeguard their overall health and preserve their eye health.
(1).jpg)