From Diagnosis to Management: Navigating Chorioretinitis
What Is Chorioretinitis?
Chorioretinitis is a medical condition characterized by inflammation and infection of the choroid and retina, two important structures located in the back of the eye. Choroid is a layer of blood vessels that supplies nutrients to the retina, and the retina is responsible for sensing light and transmitting visual signals to the brain.
Chorioretinitis can be caused by various factors, including bacterial, viral, or fungal infections, as well as autoimmune diseases, such as uveitis or lupus. It can also occur as a complication of other eye conditions, such as retinal detachment or age-related macular degeneration.
Symptoms of Chorioretinitis
Symptoms of chorioretinitis can range from mild to severe, depending on the underlying cause and extent of the inflammation. Common symptoms include:
● Blurred or decreased vision
● Floaters (small, moving specks that appear in the field of vision)
● Flashes of light (when the retina is tugged by the movement of fluid inside the eye)
● Pain or redness in the eye
● Sensitivity to light
.jpg)
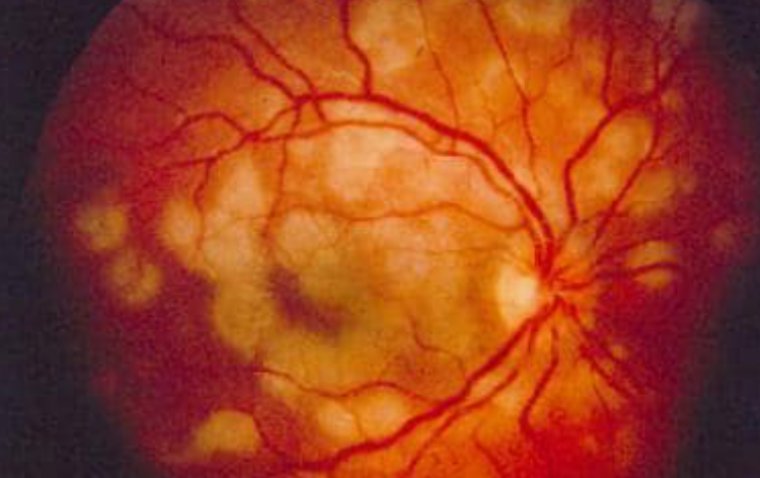
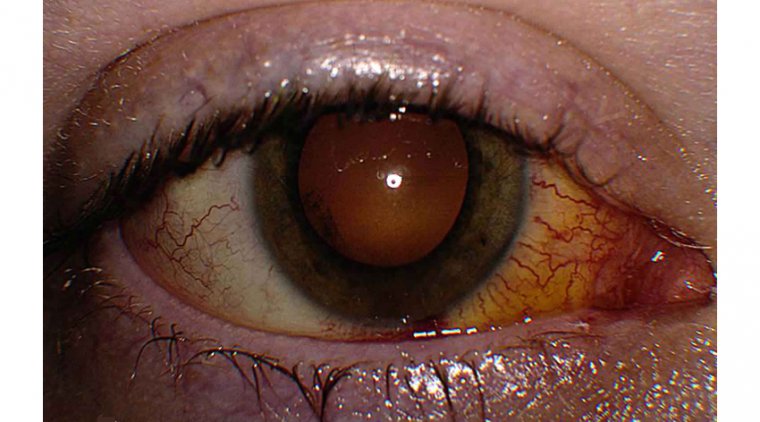
Fundus photograph of left eye showing active chorioretinitis Credit: Research Gate
What Is The Most Common Type of Chorioretinitis?
The most common type of chorioretinitis is toxoplasmic chorioretinitis. It is caused by the parasite Toxoplasma gondii and is usually acquired through contaminated food or water. Toxoplasmic chorioretinitis is more common in people with weakened immune systems, such as those with HIV/AIDS or individuals undergoing immunosuppressive treatment. This type of chorioretinitis can cause inflammation and damage to the retina and the choroid, leading to vision loss if left untreated.
How to Diagnose Chorioretinitis
Consult an ophthalmologist: The first step in diagnosing chorioretinitis is to consult an eye specialist, also known as an ophthalmologist. They will perform a comprehensive eye exam and take a thorough medical history to determine the underlying cause of the condition.
Visual acuity test: The ophthalmologist will measure the sharpness of your vision with a visual acuity test. This test involves reading letters on a chart and determining the smallest line of letters you can read.
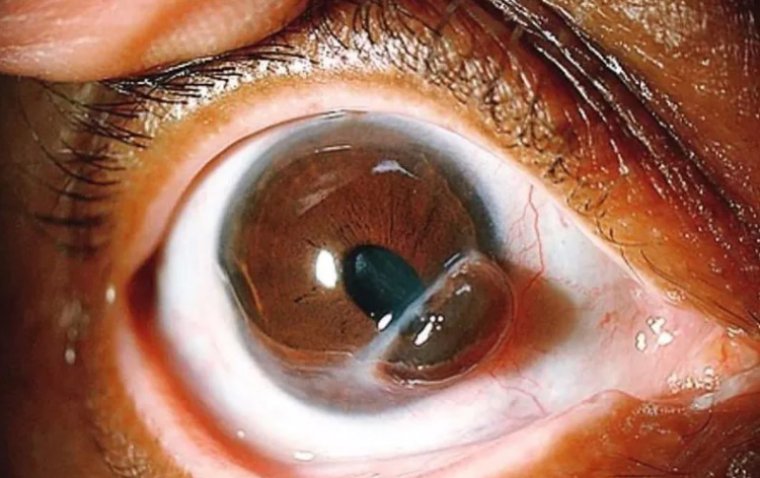
Dilated eye exam: The ophthalmologist may also dilate your pupils to get a better view of the retina and the choroid. They will use a special tool to examine the back of the eye and identify any signs of inflammation or damage.
Imaging tests: If needed, the ophthalmologist may also request additional tests, such as an optical coherence tomography (OCT) scan, fluorescein angiogram, or ultrasound to confirm the diagnosis and assess the extent of the damage.
Treating Chorioretinitis
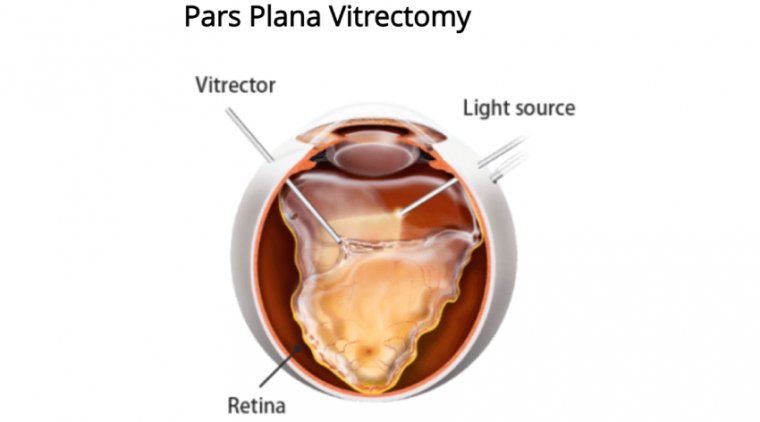
Treatment of chorioretinitis depends on the underlying cause and can range from antibiotics or antivirals for infections to corticosteroid therapy for autoimmune-related inflammation. In rare cases, laser therapy or surgery may be necessary to prevent further damage to the retina.
Preventing chorioretinitis requires practicing good eye hygiene, such as protecting the eyes from UV radiation and avoiding contact with contaminated objects. In addition, regular eye exams can help detect and treat eye conditions that may increase the risk of developing chorioretinitis.
In conclusion, chorioretinitis is a serious eye condition that can cause permanent vision loss if left untreated. It is important to seek prompt medical attention if you experience any symptoms of chorioretinitis. By taking care of your eyes and getting regular eye exams, you can help prevent the development of this condition and maintain good vision health.
(1).jpg)