The Role of Penetrating Keratoplasty in Corneal Disorder Solutions
What is Penetrating Keratoplasty?
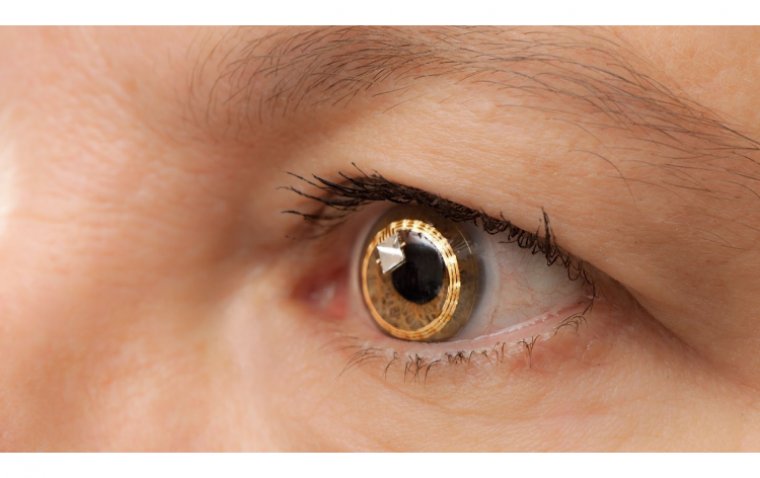
Penetrating Keratoplasty (PKP), also known as a full-thickness corneal transplant, is a significant ophthalmic surgical procedure aimed at restoring visual acuity in patients with corneal diseases. This procedure involves the replacement of the entire corneal tissue with a donor graft. It is a delicate surgery requiring meticulous precision, as the cornea is a vital component of the eye, playing a crucial role in focusing light onto the retina.
Overview of the Conditions and Disorders That May Necessitate PKP
PKP is indicated in various corneal conditions where other treatments have failed or are unsuitable. The primary indications include:
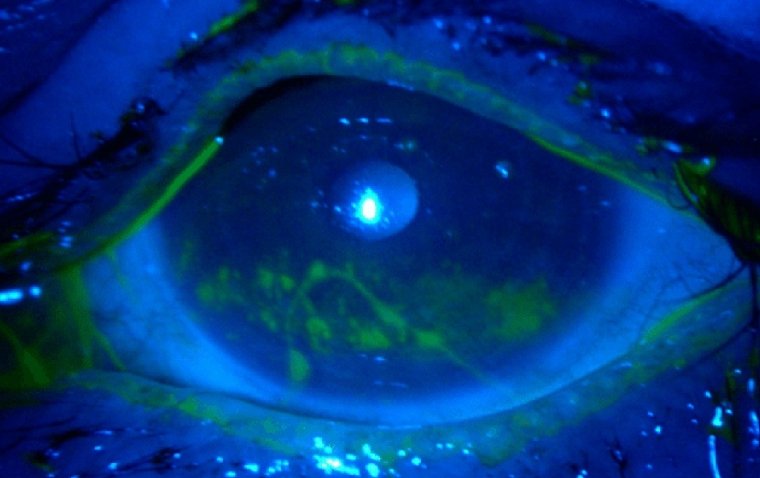
1. Keratoconus: A progressive thinning and bulging of the cornea, leading to severe astigmatism and scarring. When corrective lenses are no longer effective, PKP may be considered.
2. Corneal Scarring: Resulting from infections (like herpes simplex keratitis), injuries, or surgical complications, significant scarring can impair vision and necessitate PKP.
3. Corneal Dystrophies: These are a group of genetic, often progressive disorders affecting the cornea, such as Fuchs' dystrophy. When vision is significantly affected, PKP may be the only viable option.
4. Bullous Keratopathy: A condition often associated with cataract surgery complications, where fluid buildup leads to corneal swelling and pain. PKP can alleviate symptoms and restore clarity.
5. Corneal Ulcers and Infections: In severe cases where medical treatment is insufficient, PKP might be required to remove the infected or non-healing tissue.
6. Chemical Burns and Traumatic Injuries: In instances of severe corneal damage due to chemical exposure or physical trauma, PKP can be a restorative procedure.
Candidacy for PKP: Who Qualifies?
Evaluation Criteria for Patients Eligible for Penetrating Keratoplasty
Determining the eligibility for Penetrating Keratoplasty (PKP) involves a comprehensive assessment of both the physical state of the eye and the overall health of the patient. The evaluation criteria for PKP candidates are multifaceted and include the following key aspects:
● Severity of Corneal Disease: The primary consideration is the extent of corneal damage or disease progression. PKP is usually recommended when less invasive treatments are ineffective or when the cornea is extensively scarred or thinned.
● Corneal Thickness: Adequate corneal thickness is crucial for a successful PKP, as it affects the ability to secure the donor graft properly.
● Overall Eye Health: The absence of active ocular diseases such as severe dry eye, uncontrolled glaucoma, or retinal pathologies is essential, as these conditions can compromise the success of the transplant.
● Visual Potential: Assessment of the potential visual improvement is vital. PKP is more likely to be advised if significant vision enhancement is anticipated.
● Systemic Health Considerations: The patient's general health status, including the ability to undergo surgery and tolerate post-operative medications, is critically evaluated. Conditions like diabetes or autoimmune diseases need to be well-managed.
● Patient Compliance and Understanding: The willingness and ability of the patient to adhere to post-operative care, including regular follow-ups and medication regimens, are crucial for the success of PKP.
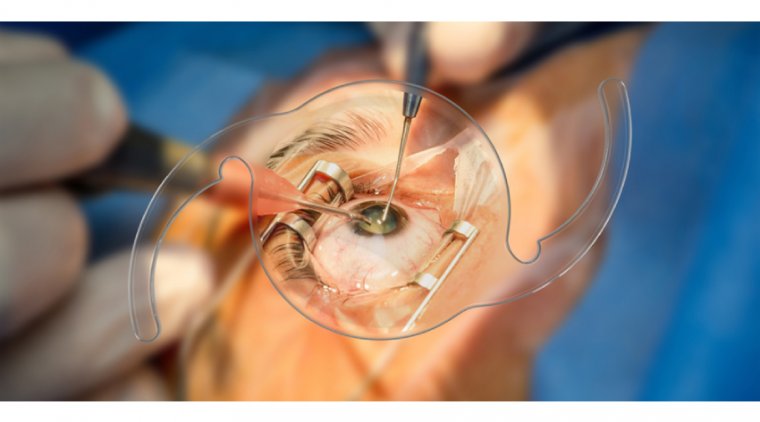
Step-by-Step Breakdown of the PKP Surgical Procedure
Penetrating Keratoplasty (PKP) is a complex but well-structured surgical process. Here is a step-by-step guide:
1. Preoperative Assessment and Preparation: This includes a thorough examination of the patient's eye, confirmation of the corneal disease, and measurement for donor cornea sizing. Patients also undergo general health assessment to ensure fitness for surgery.
2. Anesthesia and Sterilization: PKP is usually performed under local anesthesia with sedation, although general anesthesia may be used in certain cases. The eye and surrounding area are sterilized to minimize infection risk.
3. Incision and Removal of the Diseased Cornea: A precise circular incision is made on the cornea using a trephine. The diseased or damaged corneal tissue is carefully removed, leaving a gap for the donor cornea.
4. Preparation and Placement of the Donor Cornea: A donor cornea, matched in size and tissue type, is prepared. It is then placed into the opening where the patient's original cornea was removed.
5. Suturing the Graft: The donor cornea is meticulously sutured into place using fine, specialized sutures. This step requires exceptional skill to ensure proper alignment and tension.
6. Postoperative Care: The eye is usually covered with a patch and shield immediately after surgery. Postoperative care includes regular check-ups, use of antibiotic and anti-inflammatory eye drops, and careful monitoring for signs of graft rejection.
.jpg)
Insight into the Use of Donor Corneas and Grafting Techniques
The success of PKP significantly depends on the quality and suitability of the donor cornea. Donor corneas are obtained from eye banks where they are stored and preserved after being donated post-mortem. These donor tissues are rigorously tested for diseases and suitability. The matching process considers factors like corneal size, curvature, and absence of transmittable diseases.
In grafting, precision is key. The graft must fit perfectly into the recipient's eye. The suturing technique also varies depending on the specific case, with some surgeons preferring running sutures while others use individual (interrupted) sutures.
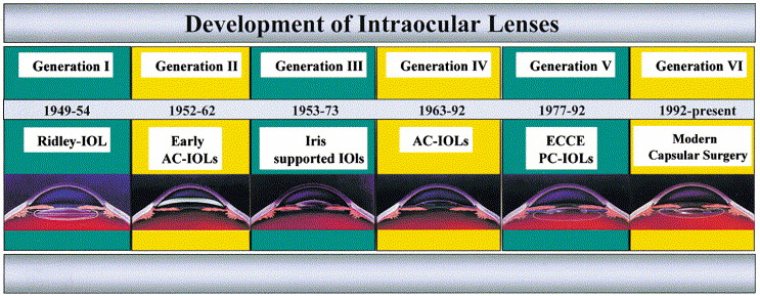
Highlighting Advancements in Technology Impacting the Surgical Process
Technological advancements have significantly impacted PKP, enhancing both its safety and efficacy:
Improved Surgical Instruments: Development of more precise trephines and suturing materials has improved the accuracy and outcomes of PKP.
Advanced Imaging Technologies: Devices like anterior segment OCT (Optical Coherence Tomography) provide detailed images of the cornea, aiding in precise graft placement.
Laser-Assisted Procedures: The introduction of femtosecond laser technology in corneal transplantation allows for more precise and consistent incisions, potentially reducing complications.
Eye Banking Techniques: Advances in cornea preservation and eye banking have extended the viability of donor tissues, making them available to more patients.
Immunosuppressive Therapies: The development of better immunosuppressive medications has reduced the risk of graft rejection significantly.
Potential Intraoperative and Post-Operative Complications
Recovery and Post-Operative Care
Guidelines for Post-Operative Care Following PKP
Following Penetrating Keratoplasty, meticulous post-operative care is crucial for optimal healing and the success of the transplant. The key guidelines include:
● Medication Adherence: Patients must strictly follow the prescribed regimen of antibiotics and anti-inflammatory eye drops to prevent infection and reduce the risk of graft rejection.
● Regular Follow-Up Appointments: These are essential to monitor the healing process, check for complications, and adjust medications as needed.
● Eye Protection: Patients should wear eye protection, especially in the initial weeks post-surgery, to avoid accidental trauma.
● Avoidance of Eye Rubbing: Rubbing the eye can disrupt the healing of the surgical site and should be avoided.
● Activity Limitations: Vigorous activities, heavy lifting, and certain sports should be avoided until the eye has sufficiently healed and the doctor advises it is safe to resume.
● Visual Rehabilitation: Use of corrective glasses or contact lenses may be necessary post-PKP for optimal vision, often after complete suture removal.
Expected Recovery Timeline and Potential Complications
The recovery timeline can vary depending on the individual case and the absence or presence of complications:
First Few Weeks: Initial healing occurs, with gradual reduction in swelling and discomfort. Vision may be blurry during this period.
First Few Months: Gradual improvement in vision is expected. Complete suture removal typically occurs around 12-18 months post-operatively, depending on healing.
Long-Term: Final visual outcomes may take up to a year or more to stabilize.
Potential complications during recovery include graft rejection, infection, increased intraocular pressure, and irregular astigmatism.
Lifestyle Adjustments and Precautions for Optimal Healing
1. Vision Considerations: Patients should be prepared for fluctuations in vision during the healing process and the possible need for vision correction.
2. Sun Protection: Wearing sunglasses is advisable to protect the eyes from UV rays.
3. Diet and Hydration: A balanced diet rich in vitamins and antioxidants, along with adequate hydration, can support healing.
4. Avoiding Contaminated Water: Activities like swimming, especially in lakes or pools, should be avoided in the early post-operative period to reduce infection risk.
5. Stress Management: Managing stress and avoiding strenuous activities that can strain the eyes is important.
6. Awareness of Symptoms: Patients should be educated about the signs of complications, such as redness, pain, or a sudden decrease in vision, and instructed to seek immediate medical attention if these occur.
Conclusion
In summary, Penetrating Keratoplasty (PKP) stands as a pivotal surgical intervention in the field of ophthalmology, offering hope and improved vision to individuals suffering from various corneal disorders. The procedure involves the full-thickness replacement of the diseased cornea with a donor graft, a process that requires exceptional surgical precision and post-operative care. PKP is indicated for conditions such as keratoconus, corneal scarring, dystrophies, and others where less invasive treatments have proven ineffective.
For those considering Penetrating Keratoplasty, it is essential to have a thorough discussion with healthcare providers. A personalized approach, considering the specific needs and conditions of each patient, is critical in making informed decisions about this life-altering surgery. Remember, each patient's journey is unique, and the best outcomes are achieved through collaboration, careful planning, and dedicated post-operative care.
(1).jpg)
.JPG)