Graves’ Eye Disease (Graves’ Ophthalmopathy or Graves’ Orbitopathy)
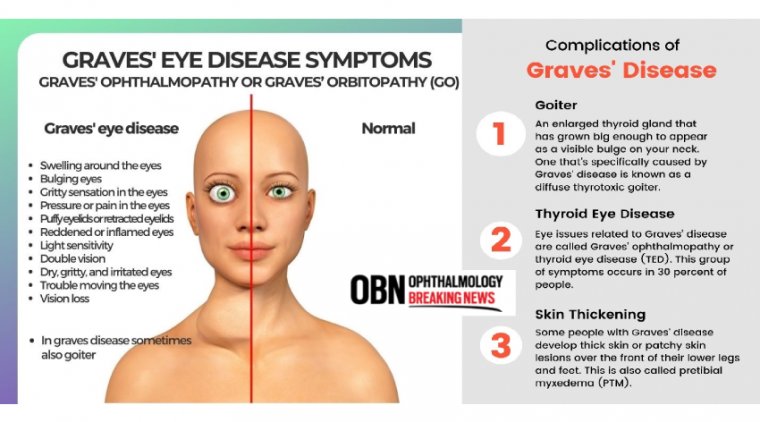
Graves’ eye disease, also known as Graves’ Ophthalmopathy or Thyroid Eye disease, is a condition that typically develops in people with an overactive thyroid caused by Graves’ disease.
The Link to Hyperthyroidism and Eye Symptoms
The underlying cause of Graves' eye disease lies in the immune system's attack on thyroid receptors. This autoimmune disorder leads to hyperthyroidism, a condition where the thyroid gland produces an excessive amount of thyroid hormones. The same antibodies that attack the thyroid receptors also affect the receptors present on the cells behind the eyes. Consequently, the eye muscles and tissues become inflamed, leading to a range of eye symptoms.
Thyroid Eye Disease (TED) Spectrum: Signs and Symptoms
Thyroid eye disease (TED) is an autoimmune condition associated with Graves' hyperthyroidism. It manifests with a spectrum of signs and symptoms, impacting the eyes and surrounding tissues.
Incidence and Demographics
TED predominantly affects women between the ages of 30 and 50. However, it's important to note that while TED is more common in women, its severity tends to be more pronounced in men and older individuals. The prevalence of TED is estimated at 16 cases per 100,000 women and three cases per 100,000 men each year.
Risk Factors
Several factors contribute to an individual's susceptibility to developing TED. Among the most significant risk factors are cigarette smoking, which not only increases the likelihood of TED but also worsens its severity. Patients with Graves’ hyperthyroidism diagnosed at an older age and those with uncontrolled thyroid dysfunction are also at a higher risk of developing TED. Additionally, individuals who have undergone radioactive iodine treatment may be at an increased risk.
Biphasic Course: Active and Inactive Phases
TED follows a biphasic course, characterized by an active phase that can last up to three years, followed by a stable or inactive phase. During the active phase, patients may experience worsening eye symptoms, while the inactive phase is marked by stabilization or improvement of symptoms.
Clinical Features of TED
TED can present with a range of clinical features, each with varying degrees of severity. Eyelid retraction is one of the hallmark signs, causing the eyes to appear more open and prominent. Periorbital edema, or swelling around the eyes, may also be evident. Patients may experience conjunctival injection and chemosis, which refers to redness and swelling of the conjunctiva (the clear membrane covering the white part of the eyes). Proptosis, the bulging of the eyes, is a significant feature of TED. Extraocular muscle restriction can lead to double vision, especially when looking in different directions. Exposure keratopathy, caused by inadequate eyelid closure, can result in dry and irritated eyes. In severe cases, TED can affect the optic nerve, potentially leading to vision loss.
Multidisciplinary Approach to TED
Given the complex nature of TED and its potential impact on various aspects of eye health, a multidisciplinary approach to management is essential. Ophthalmologists, endocrinologists, and other specialists work collaboratively to provide comprehensive care. This approach ensures that the patient's thyroid function is well-regulated, and any potential complications related to the eyes are managed promptly and effectively.
Molecular Mechanisms of TED
The pathophysiology of TED involves a complex interplay of immune responses and cellular changes in the retrobulbar tissue. The antibodies directed against the thyroid receptors lead to the proliferation of orbital fibroblasts, which are specialized cells in the eye tissues. These activated fibroblasts secrete inflammatory cytokines and hyaluronan, causing fluid accumulation in the orbit. As a consequence, the extraocular muscles and other orbital tissues become swollen and inflamed. Some fibroblasts also differentiate into mature adipocytes, leading to the expansion of orbital adipose tissue, contributing to the characteristic proptosis (bulging of the eyes) observed in TED.
Classifying TED
Classifying TED is crucial for assessing its severity and guiding treatment decisions. The 'NO SPECS' mnemonic is one of the classification tools commonly used by ophthalmologists. It outlines key clinical signs associated with TED, including No signs or symptoms, Soft tissue involvement, Proptosis, Extraocular muscle involvement, Corneal involvement, and Sight loss. The Clinical Activity Score (CAS) is another important tool that helps differentiate active and inactive stages of the disease, aiding in the monitoring of disease progression and response to treatment. Additionally, the European Group on Graves’ Orbitopathy (EUGOGO) has developed guidelines that help physicians manage TED effectively based on evidence from clinical trials.

Diagnostic Approaches for TED
Accurate and timely diagnosis of TED is essential for initiating appropriate management. The diagnostic process involves a comprehensive assessment that includes a detailed clinical history, a thorough eye examination, relevant blood tests, and imaging studies.
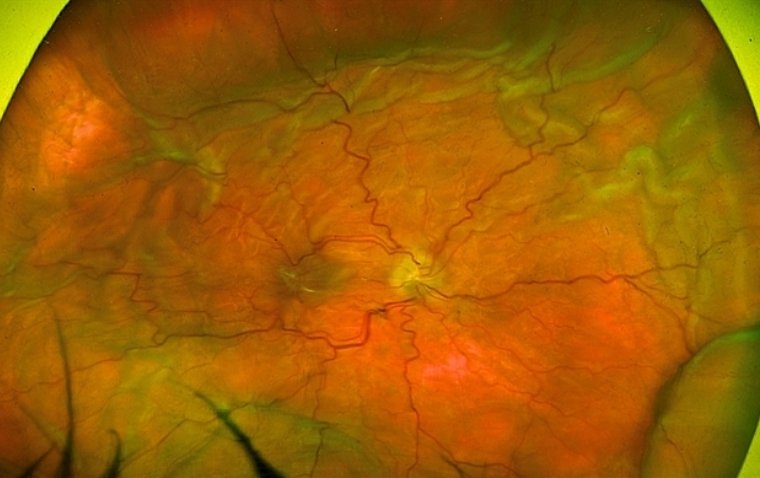
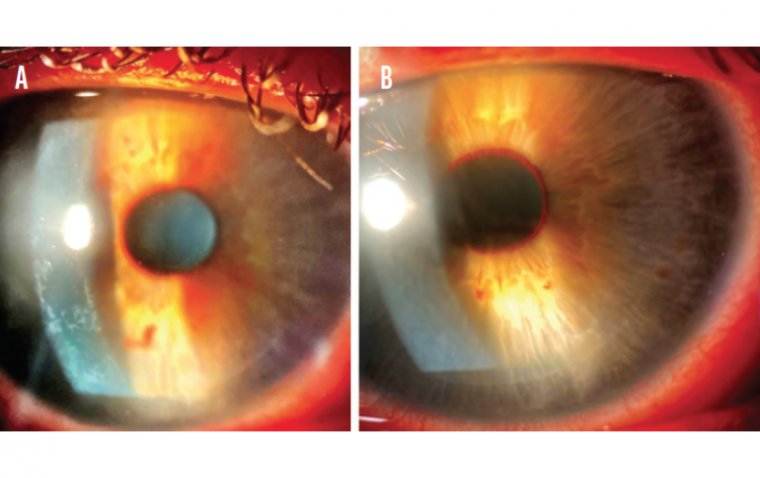
Clinical Examination and Signs
The clinical evaluation of TED focuses on assessing visual acuity, pupils, color vision, extraocular movements, visual fields, exophthalmometry (measurement of eye protrusion), external eyelid evaluation, slit-lamp examination, and dilated fundus examination. Clinicians carefully examine for signs of eyelid retraction, conjunctival and caruncle injection and/or edema, eyelid edema and/or erythema with diurnal variation, ocular motility disruption or strabismus, and proptosis.
Blood Tests
Blood tests, including a thyroid function panel, are essential to assess thyroid hormone levels. However, it's worth noting that some patients with TED may have normal thyroid function, and their thyroid hormone levels may not necessarily correlate with the severity of their eye symptoms. In such cases, additional laboratory tests, such as TSH receptor antibodies (TRAb), thyroid stimulating immunoglobulins (TSI), and thyroid peroxidase antibody (TPO), may be necessary to aid in the diagnosis.
Imaging Studies
Imaging studies, including ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI), play a significant role in confirming the diagnosis of TED and excluding other potential causes of eye-related symptoms. CT scans are commonly used to visualize the bony structures of the orbit and assess the degree of extraocular muscle involvement. MRI may be preferred when optic nerve involvement or other soft tissue abnormalities are suspected. Moreover, imaging studies allow clinicians to track disease progression and response to treatment over time.
Management of Thyroid Dysfunction
Restoring a Euthyroid State
The primary treatment goal for patients with Graves’ eye disease is to restore and maintain a euthyroid state, where thyroid hormone levels are balanced. Achieving a euthyroid state helps stabilize the underlying autoimmune process that triggers TED.
Treatment Options
There are several treatment options available for hyperthyroidism associated with Graves' eye disease. These include anti-thyroid drugs, thyroidectomy (surgical removal of the thyroid gland), and radioactive iodine therapy. Each treatment option has its benefits and potential side effects, and the choice of treatment depends on factors such as disease severity, patient preference, and overall health status.
Controversy Surrounding Radioiodine Therapy
Radioactive iodine (RAI) therapy is one of the standard treatments for hyperthyroidism. However, there is some debate over its use in patients with Graves' eye disease, as it can potentially worsen eye symptoms in some cases. Ophthalmologists may recommend the use of corticosteroids following radioiodine therapy to reduce the risk of worsening or developing TED.
Importance of Smoking Cessation
Smoking is a significant modifiable risk factor for Graves’ eye disease. Studies have shown that smokers have a higher risk of developing TED and experiencing more severe symptoms compared to non-smokers. Quitting smoking is crucial for improving overall outcomes and reducing the risk of TED-related complications.
Conservative Treatments for TED
Conservative treatment options focus on managing symptoms and providing relief for patients with TED. These non-invasive approaches can be effective in reducing discomfort and improving overall eye health.
Preservative-Free Ocular Lubrication
Preservative-free ocular lubrication is often recommended to alleviate dry eye symptoms associated with TED. These lubricating drops provide relief by mimicking the natural tear film, helping to maintain adequate moisture and comfort in the eyes.
Moisture Chambers and Eyelid Taping
Moisture chambers are protective eyewear designed to reduce exposure of the eyes to environmental elements, providing relief from symptoms such as dryness, irritation, and sensitivity to light. Eyelid taping, another conservative measure, helps in managing dry eye syndrome by promoting better eyelid closure during sleep, which can reduce symptoms of exposure keratopathy.
Sunglasses for Photosensitivity and Glare
Sunglasses can be beneficial for patients with TED, especially those experiencing photosensitivity and glare. These specially designed glasses shield the eyes from bright light and reduce discomfort caused by excessive sensitivity to light.
Prisms and Monocular Occlusion for Diplopia
During the active phase of TED, patients may experience double vision (diplopia) due to the misalignment of the eyes. In such cases, special lenses with prisms or monocular occlusion (covering one eye) can be prescribed to help manage diplopia and improve visual comfort.
Botulinum Toxin Injections and Orbital Radiation
In certain cases of TED, targeted treatments can be employed to address specific eye symptoms and provide symptomatic relief. Botulinum toxin injections can be used to address upper eyelid retraction, a common feature of TED. By temporarily weakening the muscles responsible for eyelid elevation, botulinum toxin injections help reduce the prominence of the eyes and improve their appearance. Orbital radiation, also known as radiotherapy, is sometimes utilized to reduce inflammation and swelling in the orbital tissues. It can be an option for patients with active and severe TED who do not respond adequately to other treatments. However, the use of orbital radiation remains controversial due to potential risks and uncertainties about long-term effects.
Managing Sight-Threatening TED
Sight-threatening TED refers to severe complications that can jeopardize vision and require prompt intervention to preserve eye health. Certain signs and symptoms suggest sight-threatening TED, requiring urgent evaluation and treatment. These signs include unexplained deterioration of vision, altered color vision in one or both eyes, globe subluxation (dislocation of the eye from its socket), corneal opacification, recent development of choroidal folds (abnormalities in the layer of the eye responsible for vision), and optic disc edema (swelling of the optic nerve head).
Compressive optic neuropathy, a severe complication of TED, occurs when the optic nerve is compressed within the crowded orbital space. This condition demands immediate attention, and patients may be treated with high-dose intravenous corticosteroids. If there is little or no response to corticosteroids, urgent orbital decompression surgery may be necessary to relieve pressure on the optic nerve and prevent permanent vision loss.
In severe cases of TED, exposure keratopathy can lead to corneal damage, including ulceration, thinning, and even perforation. Specialized interventions may be required to promote corneal healing and prevent further complications.
For patients with severe corneal exposure, conventional lubricants may not suffice to protect and promote healing of the cornea. In such cases, moisture chambers and specialized lubricants can be employed to create a more controlled environment, supporting corneal healing and reducing the risk of complications.
In some cases of severe TED, surgical intervention may be necessary to manage sight-threatening complications and improve visual function.
Orbital decompression surgery involves removing a portion of the bony structures around the eyes to create more space for the swollen orbital tissues. This procedure alleviates pressure on the optic nerve and reduces proptosis, helping to protect vision.
Extraocular muscle surgery, also known as strabismus surgery, is considered for patients who continue to experience double vision after orbital decompression. The goal of this surgery is to realign the eyes and reduce diplopia, enhancing binocular vision.
Eyelid procedures may be performed to address eyelid retraction and achieve a more symmetrical appearance. The aim is to maintain adequate corneal coverage and improve the overall aesthetic appearance of the eyes.
Conclusion
Graves' eye disease, or thyroid eye disease, is a complex condition that requires careful evaluation and management. A comprehensive approach that involves a multidisciplinary team of specialists can help provide the best possible care for patients with TED. Early diagnosis, along with appropriate medical and surgical interventions, can significantly improve outcomes and enhance the quality of life for individuals affected by this condition. Moreover, patients are encouraged to adopt healthy lifestyle habits, such as quitting smoking, to reduce the risk of developing or exacerbating TED. With advances in research and treatment options, the future holds promising prospects for patients with Graves' eye disease.
(1).jpg)