Bullous Keratopathy: Causes, Symptoms, and Treatment
What Is Bullous Keratopathy?
Bullous keratopathy (BK) is a pathological condition characterized by the presence of fluid-filled blisters or "bullae" on the cornea, which is the clear front surface of the eye. The main underlying factor leading to the formation of these bullae is the dysfunction or loss of the corneal endothelial cells. These cells are responsible for maintaining the correct hydration level of the cornea. When their function is compromised, it results in corneal swelling and the eventual formation of blisters, causing discomfort and reduced vision.
Bullous keratopathy predominantly affects older adults, though it can occur at any age depending on the causative factors. While the exact prevalence of BK is difficult to ascertain due to its association with various underlying conditions, it is a relatively common cause of vision impairment in elderly populations.
The incidence is found to be higher among individuals who have undergone cataract surgeries, especially if complications arose during the surgery. It's also worth noting that BK can occur in any demographic, regardless of gender or ethnicity, but those with a history of eye surgeries or eye diseases are at a heightened risk.
Bullous Keratopathy After Cataract Removal
1. Pseudophakic Bullous Keratopathy (PBK)
Pseudophakic bullous keratopathy (PBK) refers to the development of bullous keratopathy after cataract surgery in which an intraocular lens (IOL) has been implanted. It is one of the most common post-operative complications following cataract removal with lens implantation. The term 'pseudophakic' denotes the presence of an artificial lens inside the eye.
PBK arises when the corneal endothelial cells are damaged either during the surgical procedure or due to post-operative complications, leading to their dysfunction. This cell dysfunction subsequently results in corneal swelling, followed by the appearance of bullae on the cornea. PBK may manifest weeks, months, or even years after the surgery, causing reduced vision, pain, and discomfort.
2. Aphakic Bullous Keratopathy
Aphakic bullous keratopathy is similar to PBK but occurs in individuals who have undergone cataract extraction without the implantation of an intraocular lens, leaving them "aphakic" or without a lens. This condition was more prevalent in the past when IOL implantation wasn't a standard procedure after cataract extraction. The absence of the lens can change the anterior chamber's dynamics and impact the corneal endothelium.
Additionally, older surgical techniques had a higher propensity to cause endothelial damage. As with PBK, the damage to the endothelial cells leads to corneal edema and the formation of bullae. Although less common today due to advances in surgical techniques and the routine use of IOLs, aphakic bullous keratopathy remains a significant cause of vision impairment in those who had cataract surgeries in the earlier days.
Bullous Keratopathy Causes
Bullous keratopathy is fundamentally a result of endothelial cell dysfunction in the cornea. The corneal endothelium is a single layer of cells on the inner surface of the cornea, playing a crucial role in maintaining corneal clarity by actively pumping out fluid from the corneal stroma. When these cells are damaged and cannot function adequately, fluid accumulates, causing the cornea to swell. As the cornea swells, fluid-filled blisters or "bullae" can form on its surface, leading to the clinical manifestation known as Bullous Keratopathy.
Role of Previous Eye Surgeries
A major risk factor for the development of Bullous Keratopathy is previous eye surgeries, especially cataract surgery. Despite the significant advancements in surgical techniques, intraoperative trauma to the endothelial cells during cataract extraction and intraocular lens implantation can occur. This trauma, coupled with potential post-operative complications, can pave the way for bullous keratopathy. Both pseudophakic and aphakic bullous keratopathy, as mentioned earlier, are subtypes related to cataract surgeries.
Other Risk Factors:
● Trauma: Direct trauma to the eye can result in damage to the corneal endothelium, leading to Bullous Keratopathy. This includes both blunt trauma and penetrating injuries.
● Glaucoma: Chronic elevated intraocular pressure, as seen in glaucoma, can stress the corneal endothelium. Prolonged use of certain glaucoma medications or complications from glaucoma surgeries can also pose a risk.
● Ocular Diseases: Conditions such as Fuchs' endothelial dystrophy, where there's a progressive loss of endothelial cells, can predispose an individual to bullous keratopathy. Other diseases that affect the corneal endothelium can also be contributing factors.
● Contact Lens Wear: Extended or inappropriate use of contact lenses can cause trauma to the endothelium, especially if the lenses do not fit correctly or are not maintained properly.
Signs and Symptoms of Bullous Keratopathy
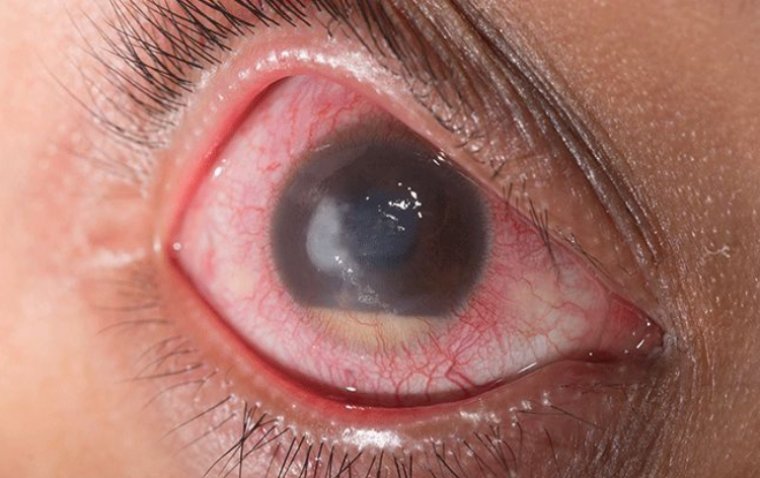
Bullous keratopathy presents with a myriad of signs and symptoms stemming from the accumulation of fluid in the cornea and the formation of bullae or fluid-filled blisters on the corneal surface. These clinical manifestations can be quite distressing for the affected individuals.
Progression of Symptoms:
1. Pain: One of the earliest and most prominent symptoms of Bullous Keratopathy is pain. As the fluid accumulates in the cornea and blisters form, these can rupture and cause significant pain. The exposed nerve endings in the corneal layers contribute to the sensation of pain. The intensity of the pain can vary from a mild, persistent irritation or foreign body sensation to severe, sharp pain.
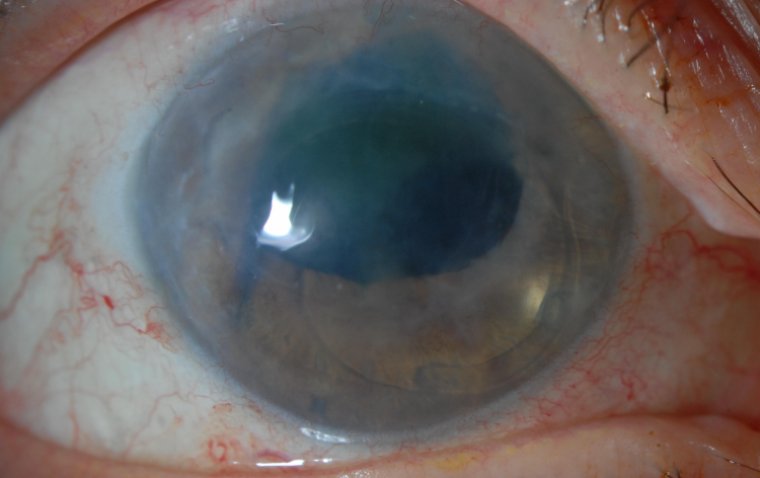
2. Blurred Vision: As the corneal endothelial cells fail to maintain corneal deturgescence, the cornea swells, leading to a loss of its usual clarity. This causes a gradual or sometimes sudden decrease in vision. The swelling primarily affects the cornea's stroma and epithelium, making the vision hazy or clouded.
3. Photophobia: Individuals with Bullous Keratopathy often experience heightened sensitivity to light, known as photophobia. The swollen cornea, along with ruptured blisters, can amplify light dispersion as it enters the eye, leading to discomfort or pain in bright lighting conditions.
4. Tearing: Increased tearing or watery eyes can be a reflex response to corneal irritation and pain.
5. Foreign Body Sensation: Patients often describe a gritty or sandy feeling in the eye, akin to having a foreign body lodged within. This sensation is due to the surface irregularities caused by the blisters and their rupture.
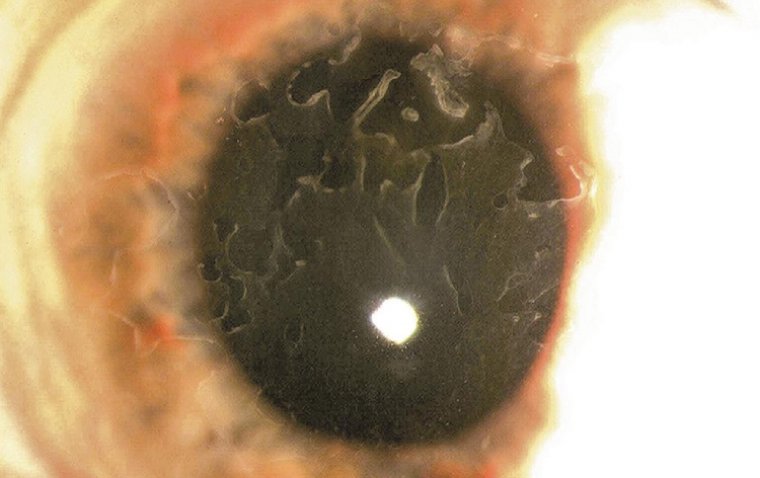
6. Epithelial Erosion: Over time, recurrent rupture of the bullae can lead to areas of epithelial erosion, making the eye vulnerable to infections and further exacerbating the symptoms.
7. Corneal Opacity: In chronic cases, or if left untreated, there may be the formation of subepithelial fibrosis and corneal scarring, leading to a further reduction in vision.
How to Diagnose Bullous Keratopathy
The diagnosis of Bullous Keratopathy begins with a comprehensive eye examination. During the clinical assessment, a patient's medical history, especially any prior eye surgeries, trauma, or diseases, is thoroughly reviewed. Some of the critical examination techniques include:
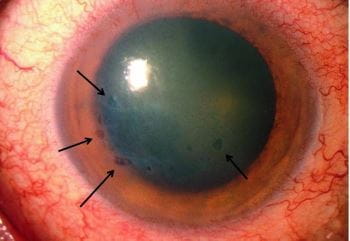
● Slit-lamp Examination: This is a frontline tool in ophthalmology. It provides a detailed, magnified view of the anterior segment of the eye. In Bullous Keratopathy, the slit-lamp reveals corneal edema, bullae formation, and epithelial irregularities.
● Fluorescein Staining: By using this dye, ophthalmologists can identify and assess the areas of epithelial erosion or defects that result from the rupture of bullae.
Importance of Corneal Imaging and Pachymetry
● Specular Microscopy: This non-invasive imaging technique is used to examine the corneal endothelium. In Bullous Keratopathy, it can reveal decreased endothelial cell density, cell polymorphism, and polymegethism.
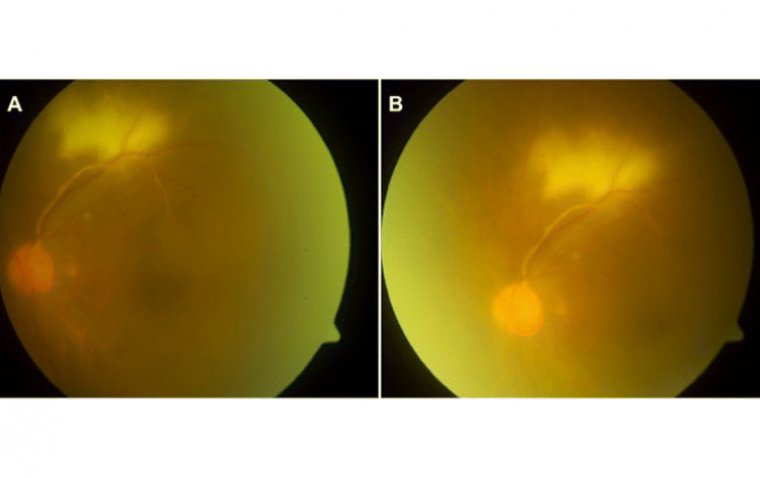
● Optical Coherence Tomography (OCT): Anterior segment OCT provides a cross-sectional image of the cornea, highlighting the layers affected by edema and the presence of bullae.
● Pachymetry: It is a technique used to measure the thickness of the cornea. Given that corneal edema is a hallmark of bullous keratopathy, pachymetry often shows an increased corneal thickness in affected individuals.
Differential Diagnosis to Rule Out Other Similar Ocular Conditions
Bullous keratopathy can mimic several other corneal disorders. Therefore, differential diagnosis is crucial to ensure accurate treatment. Some conditions to consider include:
● Fuchs' Endothelial Dystrophy: Like bullous keratopathy, Fuchs' also involves corneal endothelial cell loss and stromal edema. However, it's primarily a genetic condition and usually affects both eyes.
● Corneal Hydrops: Seen primarily in keratoconus patients, it's a sudden and painful swelling of the cornea, but the presentation and underlying causes are different.
● Infectious Keratitis: While it can cause corneal edema and pain similar to bullous keratopathy, this condition will often have accompanying signs of infection such as redness, discharge, and an inflammatory response.
● Corneal Abrasion or Ulcer: Though these can produce symptoms similar to Bullous Keratopathy, their causes and presentations are distinct, often involving trauma or infection.
Bullous Keratopathy Treatment
Bullous keratopathy, being a progressive disorder of the cornea, requires targeted interventions to manage symptoms and address the root cause. Treatment approaches, ranging from non-surgical to surgical modalities, are geared towards reducing corneal edema, relieving pain, and improving vision.
Non-surgical Management Approaches
1. Medication:
● Hyperosmotic Agents: Solutions such as sodium chloride 5% eyedrops or ointment can help draw fluid out of the cornea, reducing swelling.
● Topical Anti-inflammatory Eye Drops: Steroidal and non-steroidal anti-inflammatory eye drops can manage inflammation and provide symptomatic relief.
● Lubricating Eye Drops and Ointments: These can aid in providing comfort and relief from symptoms like foreign body sensation or dryness.
2. Lifestyle Changes:
● Limiting Eye Strain: Patients might benefit from reducing activities that cause eye strain, like excessive reading or screen time.
● Sunglasses: Wearing sunglasses can help reduce photophobia (light sensitivity) which is commonly associated with the condition.
● Avoiding Trauma: Being cautious and protecting the eyes from potential injury is crucial, as any additional trauma can exacerbate the condition.
Advanced Surgical Interventions:
1. Corneal Transplantation (Penetrating Keratoplasty): This involves replacing the damaged cornea with healthy donor tissue. It's a more traditional approach and is generally reserved for cases where the entire corneal thickness is compromised.
2. Endothelial Keratoplasty: This is a more contemporary approach, focusing on the replacement of only the damaged inner layer of the cornea (endothelium). Types include:
● Descemet's Stripping Automated Endothelial Keratoplasty (DSAEK): Only the abnormal endothelial layer is replaced with a thin layer of donor tissue.
● Descemet Membrane Endothelial Keratoplasty (DMEK): A selective transplant involving only the innermost layer of the cornea, resulting in potentially faster visual recovery and lesser risk of graft rejection.
3. Therapeutic Contact Lenses: In some cases, wearing a bandage contact lens can help in reducing pain and discomfort by protecting the compromised corneal surface.
Summary
Bullous keratopathy is a corneal disorder that presents with edema, pain, and vision disturbances. While medications and lifestyle modifications can provide relief from symptoms, the definitive resolution, especially in advanced cases, often necessitates surgical intervention. Both traditional and contemporary surgical methods offer promising outcomes. However, the choice of treatment should be individualized, considering the severity of the disease, patient's age, comorbidities, and their specific needs. Regular follow-ups with an ophthalmologist are crucial to monitor disease progression and ensure optimal visual rehabilitation.
(1).jpg)