Explained: Why Do Some Corneal Transplants Fail?
| Table of Content |
| Immunological Rejection |
| Graft-versus-Host Disease (GVHD) |
| Postoperative Infections |
| Recurrent Corneal Diseases |
| Surgical Complications |
| To Conclude |
Corneal transplantation, also known as keratoplasty, is a common procedure performed to restore vision in individuals with corneal diseases or injuries. While the majority of corneal transplants are successful, a significant number of cases experience complications or ultimately fail.
This article delves into the complex factors that contribute to corneal transplant failures, shedding light on the challenges encountered in achieving long-term success.
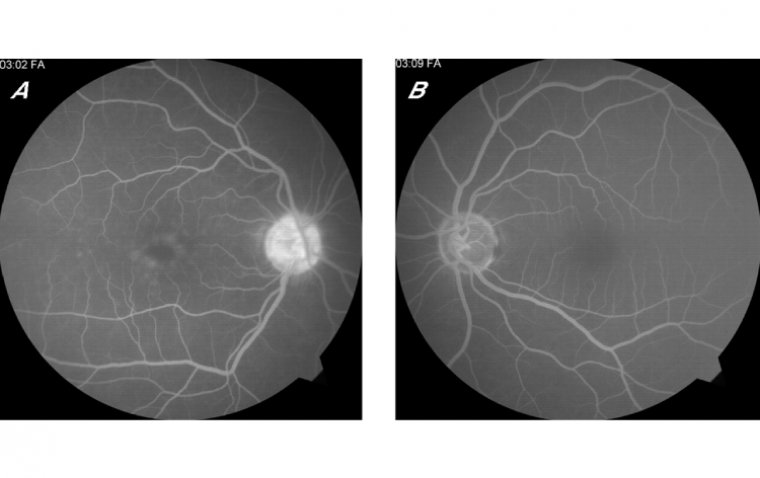
1. Immunological Rejection
One of the leading causes of corneal transplant failure is immunological rejection. The cornea is a unique tissue that typically enjoys immune privilege, meaning it is less susceptible to immune system attacks. However, transplanting corneal tissue from a donor introduces foreign antigens that can trigger an immune response, leading to rejection. The recipient's immune system may recognize the transplanted cornea as an invader and initiate a destructive immune reaction, resulting in graft failure.
2. Graft-versus-Host Disease (GVHD)
GVHD is a rare but severe complication that can occur when the donor cornea contains immune cells that attack the recipient's tissues. This condition is more common in cases where corneal tissue is transplanted from a related donor, such as a family member. GVHD can lead to significant inflammation, scarring, and graft failure.
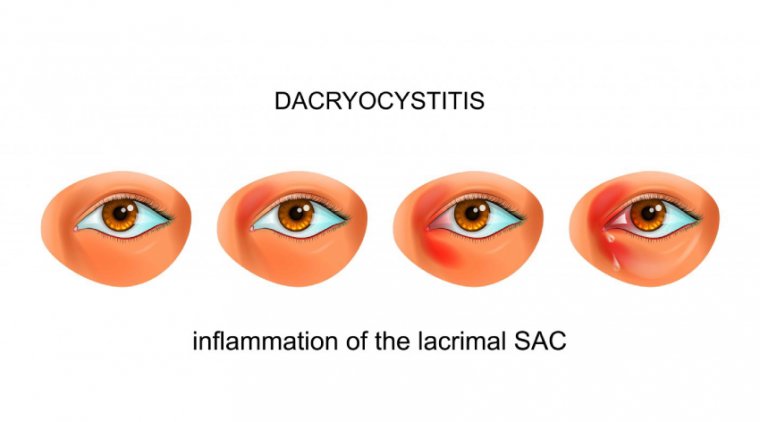
3. Postoperative Infections
Infections following corneal transplantation pose a significant risk to the success of the procedure. Bacterial, fungal, or viral infections can adversely impact the transplanted cornea, leading to graft failure. Strict adherence to sterile surgical techniques, vigilant postoperative care, and appropriate administration of prophylactic antibiotics is crucial in reducing the risk of infections.
4. Recurrent Corneal Diseases
Some underlying corneal diseases, such as certain forms of keratoconus or Fuchs' endothelial dystrophy, can recur even after a successful corneal transplant. These diseases can affect the newly transplanted cornea and compromise its long-term function, eventually leading to graft failure. Close monitoring and proactive management of the underlying condition are essential in mitigating this risk.
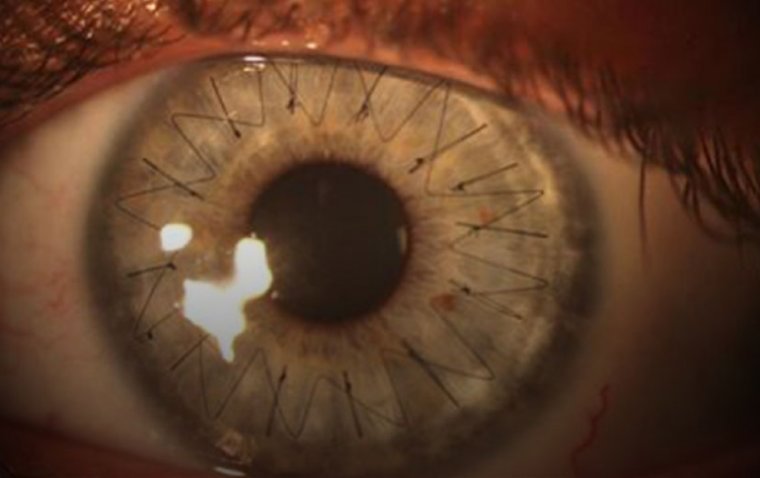
5. Surgical Complications
Various surgical complications can contribute to corneal transplant failures. Issues such as inadequate wound healing, suture-related problems, or graft misalignment can compromise the integrity and function of the transplanted cornea. Skillful surgical techniques, meticulous wound closure, and careful monitoring postoperatively can help minimize such complications.
To Conclude…
Corneal transplantation is a valuable procedure that has restored vision in countless individuals worldwide. However, understanding the factors contributing to corneal transplant failures is crucial to improve long-term outcomes.
By addressing challenges related to immunological rejection, graft-versus-host disease, infections, recurrent corneal diseases, and surgical complications, researchers and clinicians can work towards enhancing the success rates of corneal transplants. Continued research and advancements in surgical techniques, immunosuppressive therapies, and postoperative care hold promise for improved outcomes and increased success rates in corneal transplantation.
(1).jpg)