Corneal Melt: A Rare but Vision-Threatening Condition
What Is Corneal Melt? (Keratolysis)
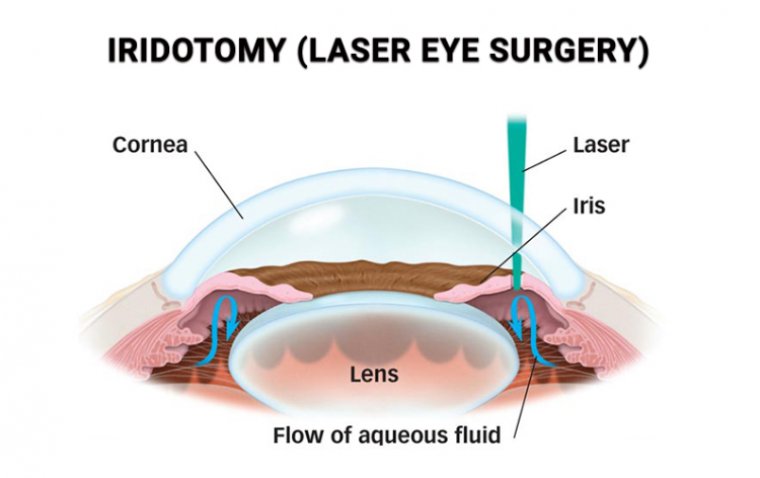
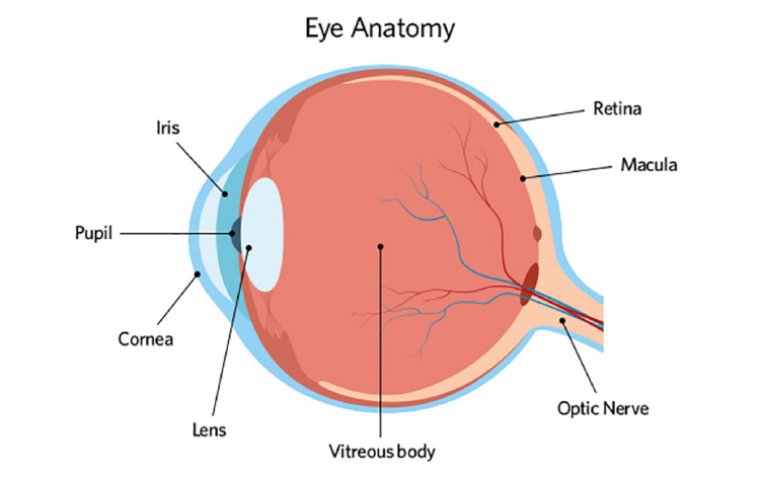
Corneal Melt, also known as keratolysis, is a severe degenerative condition of the eye characterized by the progressive dissolution of the corneal stroma, the middle and thickest layer of the cornea. This dissolution often leads to a thinning and potential perforation of the cornea, posing a serious threat to vision.
The cornea is a vital component of the eye's optical system. It functions as the outermost lens, focusing light onto the retina, which then transmits visual signals to the brain. A clear and intact cornea is essential for good vision as it contributes to about 65-75% of the eye's total focusing power. Corneal melt compromises the structural integrity and clarity of the cornea, which in turn, significantly affects visual acuity and can lead to vision loss if left untreated.
Corneal melt is considered a rare but serious condition. Its rarity makes it a challenging condition to diagnose and manage, often requiring the expertise of cornea specialists. The occurrence of corneal melt can be devastating, given its potential to cause severe vision impairment or blindness. Therefore, it's a condition that underscores the importance of early detection and intervention to preserve eye health and vision.
What Causes a Corneal Melt?
Corneal melt, or keratolysis, can result from various factors and medical conditions. Below are some notable causes categorized under autoimmune diseases, infections, and trauma:
1. Autoimmune Diseases: Autoimmune diseases can significantly contribute to the development of corneal melt:
● Collagen Vascular Diseases: These diseases are found in approximately 50% of all noninfectious cases of peripheral ulcerative keratitis, a serious condition synonymous with corneal melt. Rheumatoid arthritis is the most prevalent among these diseases.
● Other Autoimmune Disorders: Various autoimmune disorders can trigger inflammatory responses that affect the cornea's health, potentially leading to corneal melt.
2. Infections: Infections can cause or exacerbate corneal melt:
● Microbial Keratitis: This is a severe infection of the cornea that can lead to corneal melt if not treated promptly.
3. Trauma: Trauma to the eye can cause immediate or delayed onset of corneal melt:
● Penetrating Injuries: Injuries that penetrate the eye can cause immediate damage to the cornea, leading to corneal melt.
4. Postoperative Complications: Corneal melt can occur postoperatively due to infectious, inflammatory, or trophic causes. Structural or mechanical eyelid problems, known as Dellen effects, may also contribute to postoperative corneal melt.
5. Other Factors
● Nutritional Causes: Although less common in developed countries, nutritional deficiencies can contribute to corneal melt.
The exact incidence or prevalence of corneal melt is not widely reported, but a study aimed to estimate the incidence of corneal melting in association with systemic disease in the Yorkshire Region, emphasizing the systemic association with this condition.
What Are the Symptoms of Corneal Melting?
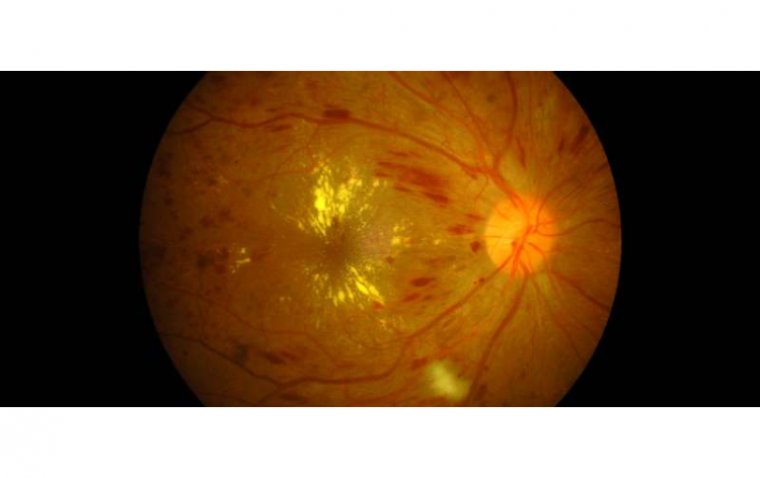
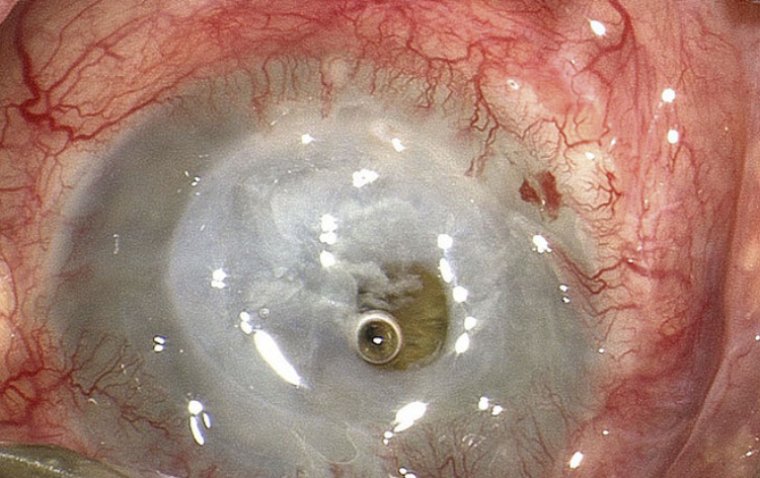
Credit: Science Direct
Corneal melt presents with a variety of symptoms, some more common than others. Here are the symptoms associated with corneal melt:
● Pain: One of the most common symptoms is eye pain which can range from mild to severe.
● Redness: The eye may appear red and inflamed due to irritation and inflammation.
● Visual Disturbances: blurred vision, decreased visual acuity
● Tearing: Increased tearing or watery eyes is a common symptom.
● Sensitivity to Light: Individuals may experience heightened sensitivity to light, known as photophobia.
● Foreign Body Sensation: A sensation of something being in the eye may be experienced.
● Eye Discharge: There might be a discharge from the eye, especially if an infection is present.
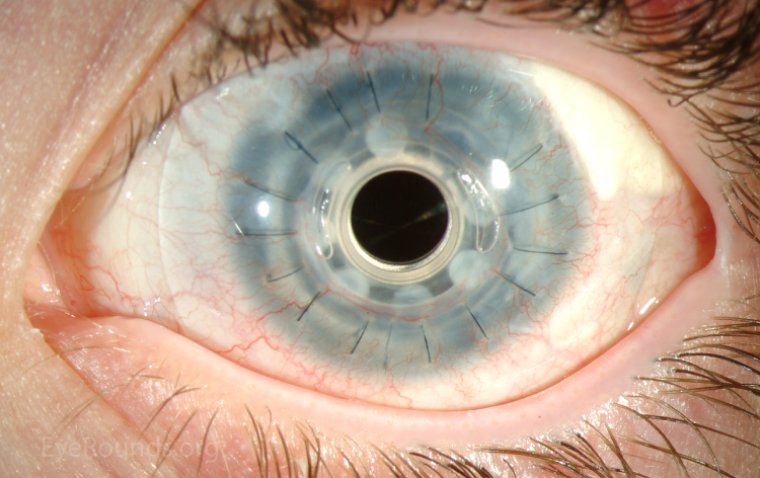
● Visible Thinning or Clouding of the Cornea: In severe cases, the thinning or clouding of the cornea may be visible to the naked eye or upon close inspection.
How to Diagnose Corneal Melting
The diagnosis of corneal melt is a thorough process that involves a detailed examination by an ophthalmologist, supplemented by specific diagnostic tests to ascertain the extent of the condition and plan the treatment accordingly. Early diagnosis and prompt medical attention are crucial to mitigate the risks and manage the condition effectively.
1. Ophthalmologist Examination: A comprehensive eye examination by an ophthalmologist is the first and foremost step in diagnosing corneal melt:
2. Slit-Lamp Examination: Utilizing a slit-lamp, the ophthalmologist examines the cornea under high magnification to assess its clarity, thickness, and overall structure. This helps in identifying any areas of thinning or other abnormalities associated with corneal melt.
3. Visual Acuity Testing: Assessing the visual acuity helps in determining the impact of the corneal melt on vision.
4. Intraocular Pressure Measurement: Measuring the pressure inside the eye is essential to rule out other ocular conditions that might be contributing to the symptoms.
5. External Eye Examination: Examining the eyelids, conjunctiva, and the surrounding structures to check for any abnormalities or signs of infection.
6. Diagnostic Tests: Specific diagnostic tests provide a more detailed understanding of the extent and nature of corneal melt:
7. Corneal Topography: Though not done commonly in the cases of corneal melt, this test maps the surface curvature of the cornea, providing detailed information about its shape and any irregularities.
8. Optical Coherence Tomography (OCT) of the Anterior Segment: OCT captures cross-sectional images of the cornea, allowing for a detailed assessment of its thickness and structure.
9. Corneal Pachymetry: Measuring the thickness of the cornea helps in assessing the extent of corneal melt.
10. Microbiological Testing: If an infection is suspected, samples from the cornea may be taken for microbiological testing to identify any pathogenic organisms.
Treatment Options for Corneal Melt
The treatment of corneal melt is a meticulous process aimed at addressing the underlying causes, preventing further corneal degradation, and restoring vision. Below are various treatment approaches categorized under medical management, surgical interventions, and aftercare:
1. Medical Management: The primary goal of medical management is to treat the underlying conditions and halt the progression of corneal melt:
● Topical and Systemic Immunosuppression: These medications help in managing autoimmune or inflammatory conditions associated with corneal melt.
● Antibiotic Eye Drops: Used to treat or prevent bacterial infections which might exacerbate corneal melt.
● Steroidal Eye Drops: These help to reduce inflammation and slow down the corneal melting process.
● Artificial Tears: Lubricating the eye can help in alleviating dryness and irritation, which may aggravate corneal melt.
2. Surgical Interventions: Surgical procedures aim to repair the damaged cornea and restore vision:
● Corneal Gluing: Temporizing measure to seal small corneal perforations using medical-grade adhesive.
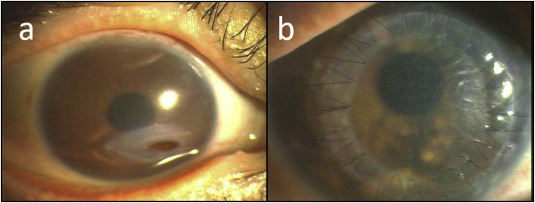
● Corneal Transplantation: In cases of severe corneal melt, transplantation of a healthy cornea from a donor might be necessary.
●Lamellar Keratoplasty and Penetrating Keratoplasty: Procedures to replace the affected corneal tissue with healthy donor tissue.
● Corneal Cross-Linking (CXL): A recent advancement, CXL, strengthens corneal tissue to halt the melting process.
Are There Any Tips to Prevent Corneal Melt?
Preventing corneal melt, especially in individuals at higher risk due to underlying systemic or ocular conditions, is of paramount importance. Here are some preventive measures, lifestyle adjustments, and medical management tips:
● Regular Eye Examinations: Routine eye check-ups can help in early detection of conditions that may lead to corneal melt. This is especially vital for individuals with known autoimmune diseases or other systemic conditions that could affect eye health.
● Manage Underlying Conditions: If you have autoimmune disorders or other health conditions associated with eye problems, work closely with your healthcare providers to manage these conditions effectively. This includes adhering to prescribed medications and treatment plans.
● Use Prescribed Eye Drops: If you have a history of eye infections or other eye conditions, it’s essential to use any prescribed eye drops or medications as directed to maintain eye health and prevent complications that could lead to corneal melt.
● Eye Protection: Protect your eyes from potential injuries and irritants by wearing protective eyewear during activities that pose a risk to eye safety. This includes sports, woodworking, or when exposed to chemicals or harsh environmental conditions.
● Avoid Eye Rubbing: Avoid rubbing your eyes, as this can cause irritation and potentially exacerbate existing eye conditions or create a conducive environment for infections.
● Maintain Good Eye Hygiene: Practice good eye hygiene by washing your hands frequently, especially before touching your eyes, and keeping contact lenses clean.
● Nutritional Balance: Maintain a balanced diet rich in vitamins and minerals essential for eye health. Vitamins A and C, in particular, are known to support corneal health.
● Stay Hydrated: Adequate hydration is crucial for maintaining the moisture balance in your eyes, which can be beneficial for corneal health.
● Educate Yourself: Stay informed about your eye health and the risks associated with corneal melt. Understanding your risks and the steps you can take to mitigate them is empowering and beneficial for proactive eye care.
Summary
Corneal melt, or keratolysis, is a severe, albeit rare, eye condition characterized by the progressive dissolution of the corneal stroma, leading to corneal thinning and potentially, perforation. The cornea plays a crucial role in focusing light onto the retina, and any damage to it can significantly impair vision. Corneal melt usually arises due to underlying autoimmune diseases, infections, or trauma to the eye. The symptoms of corneal melt vary from eye redness, pain, and tearing to more severe signs like visible thinning or clouding of the cornea and reduced visual acuity.
Early detection through regular eye examinations and prompt medical attention are fundamental for managing this condition effectively. Diagnosis encompasses a thorough ophthalmologist examination alongside specific diagnostic tests such as corneal topography and Optical Coherence Tomography of the anterior segment.
Treatment options include medical management to address underlying conditions and halt the corneal melting progression, surgical interventions like corneal transplantation or corneal cross-linking to repair the damaged cornea, and diligent aftercare to monitor healing and prevent recurrence.
Preventive measures mainly revolve around managing underlying conditions, protecting the eyes from injury, and maintaining good eye hygiene. Regular eye check-ups are indispensable for early detection of potential issues and timely intervention.
We strongly encourage readers to seek immediate medical attention if they experience any eye-related symptoms, especially those associated with corneal melt. Your eye health is an integral part of your overall wellbeing, and timely care is crucial for preserving your vision.
(1).jpg)