Corneal Staining: An In-Depth Examination of Causes and Effects
What Is Corneal Staining?
Corneal staining is a critical concept in the field of eye health, referring to a condition where the cornea, the clear front surface of the eye, becomes stained or discolored. This phenomenon is particularly significant because it often indicates underlying issues or damage to the cornea, which is vital for maintaining clear vision. Corneal staining results from the application of special eye drops containing a fluorescent dye that adheres to damaged or compromised areas of the cornea. These stained areas become visible under specific lighting conditions during an eye examination.
Corneal staining serves as an essential diagnostic tool for eye care professionals, allowing them to identify irregularities, injuries, or conditions affecting the cornea's health and integrity. The extent and pattern of staining provide valuable insights into the underlying causes, such as dry eye syndrome, contact lens-related problems, or ocular allergies. Moreover, corneal staining can manifest as discomfort, redness, or visual disturbances for the affected individual, making it a significant concern both diagnostically and in terms of patient well-being.
What Are the Different Types of Corneal Staining?
Corneal staining can manifest in different patterns and types, each indicative of specific underlying issues or conditions affecting the cornea. Understanding these types of corneal staining is essential for eye care professionals to make accurate diagnoses and implement appropriate treatment strategies. Here, we will explore the various types:
1. Diffuse Corneal Staining: This type of staining covers a broad area of the cornea and is often associated with dry eye syndrome. Diffuse staining indicates a deficiency in the tear film, which can lead to increased friction between the eyelid and the cornea.
2. Punctate Epithelial Erosions (PEEs): PEEs are tiny, discrete spots of staining on the cornea's surface. They are a common finding in conditions like dry eye, ocular allergies, or contact lens-related issues. PEEs can cause discomfort and irritation.
3. Superficial Punctate Keratitis (SPK): SPK is characterized by multiple, small punctate areas of staining on the cornea. It often results from infections, allergies, or exposure to irritants.
4. Filamentary Keratitis: In this type of staining, small filaments or strands of damaged epithelial cells adhere to the cornea's surface. It is usually associated with severe dry eye and can cause significant discomfort and foreign body sensation.
5. Sectoral Staining: Sectoral staining affects a specific region or sector of the cornea. Its presence may indicate localized eye conditions or injuries, such as corneal abrasions or infections.
6. Central Corneal Staining: This type involves staining at the center of the cornea and can be seen in conditions like keratoconus or corneal dystrophies. Central staining may affect vision and requires careful management.
7. Peripheral Corneal Staining: Staining occurring at the cornea's periphery can be associated with various causes, including contact lens-related issues or ocular allergies. It's essential to identify and address the underlying factor.
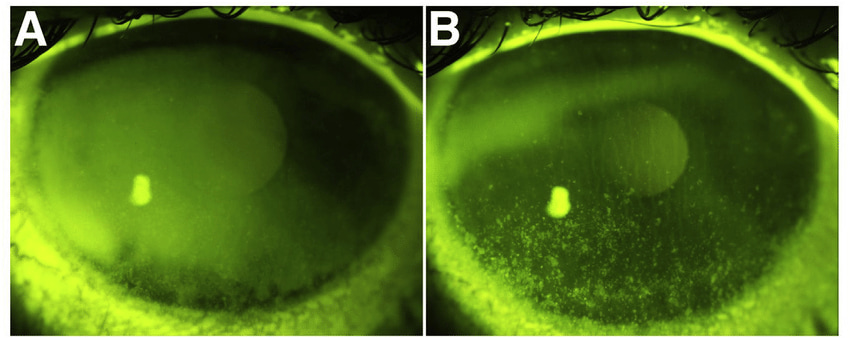
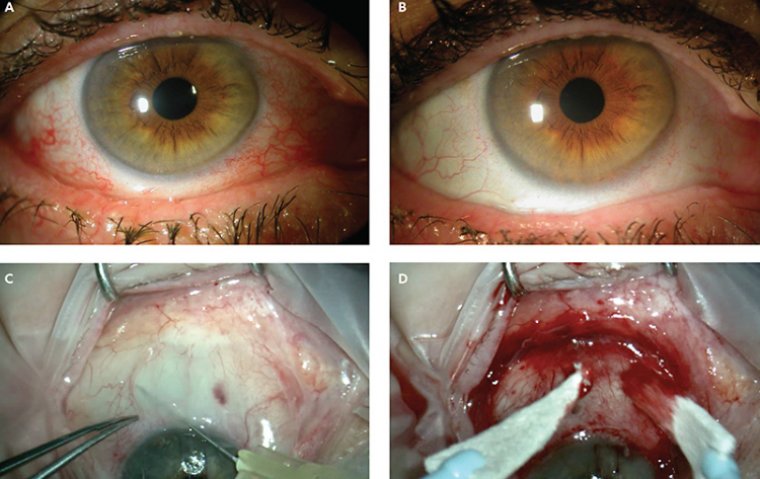
Credit: Research Gate
What Causes Corneal Staining?
1. Contact Lens Use
● Extended Wear Contacts: Prolonged use of extended-wear contact lenses can reduce corneal oxygen supply, leading to corneal staining.
● Improper Lens Care: Inadequate cleaning or disinfecting of contact lenses can introduce irritants or pathogens, causing staining.
● Ill-Fitting Lenses: Poorly fitting lenses can lead to friction and mechanical trauma on the cornea's surface.
2. Dry Eyes
● Tear Film Imbalance: Insufficient tear production or poor-quality tears can result in corneal exposure and dryness, leading to staining.
● Blink Abnormalities: Infrequent or incomplete blinking can disrupt the even distribution of tears, increasing the risk of staining.
3. Eye Injuries
● Corneal Abrasions: Scratches or injuries to the corneal surface can lead to localized staining.
● Foreign Bodies: Particles like dust, sand, or metal fragments can cause mechanical abrasions and staining.
4. Environmental Factors
● Allergens: Pollen, dust, or pet dander can trigger allergies, leading to itching, rubbing, and potential corneal staining.
● UV Exposure: Excessive exposure to ultraviolet (UV) radiation from sunlight or tanning beds can harm the cornea over time.
5. Ocular Infections
● Bacterial or Viral Infections: Infections like conjunctivitis can result in ocular discomfort and potential staining.
● Contact Lens-Related Infections: Inadequate lens hygiene can introduce harmful microorganisms to the cornea.
6. Medications
● Preservatives: Some eye drops contain preservatives that, with prolonged use, can contribute to irritation and staining.
7. Underlying Eye Conditions
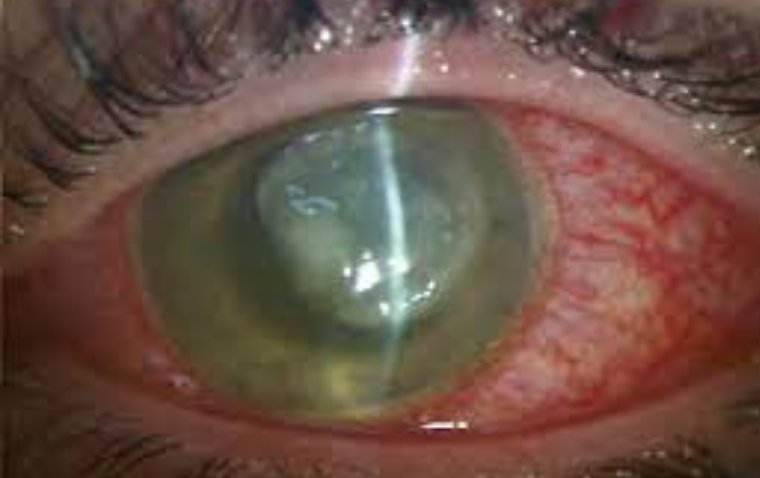
● Keratoconus: A progressive eye disorder characterized by a thinning cornea, making it prone to staining.
● Corneal Dystrophies: Inherited corneal disorders that can affect its clarity and integrity, leading to staining.
Symptoms of Corneal Staining
Corneal staining can manifest through various symptoms, which can vary in severity and frequency. Here are some common and less common symptoms associated with corneal staining:
Common Symptoms
● Eye Redness: The eyes may appear bloodshot due to irritation.
● Blurry Vision: Vision may become temporarily blurred or distorted.
● Foreign Body Sensation: A feeling of having something in the eye, often leading to frequent blinking or rubbing.
● Watery Eyes: Excessive tearing can result from eye irritation.
● Photophobia: Increased sensitivity to light, making it uncomfortable to be in well-lit environments.
● Grittiness: A sensation of grit or sandpaper on the eye's surface.
● Burning or Stinging: Discomfort and burning sensations, particularly when blinking.
● Itching: Intense itching, which can lead to increased rubbing and potential exacerbation.
● Mucous Discharge: Thick or stringy discharge from the eyes.
Less Common Symptoms
● Eye Pain: Sharp or throbbing pain, often associated with more severe corneal abrasions.
● Hazy Vision: A foggy or cloudy appearance to the vision.
● Increased Blinking: Frequent and involuntary blinking to alleviate discomfort.
● Corneal Ulcers: In severe cases, corneal staining can lead to the development of corneal ulcers, which are open sores on the cornea.
These symptoms can significantly impact daily life, making activities such as reading, working on a computer, or even being outdoors uncomfortable or challenging. Additionally, constant rubbing of the eyes to relieve symptoms can potentially worsen the condition and lead to further complications.
How to Diagnose Corneal Staining
1. Clinical Examination: Ophthalmologists and eye care professionals employ various methods to diagnose corneal staining during a clinical examination:
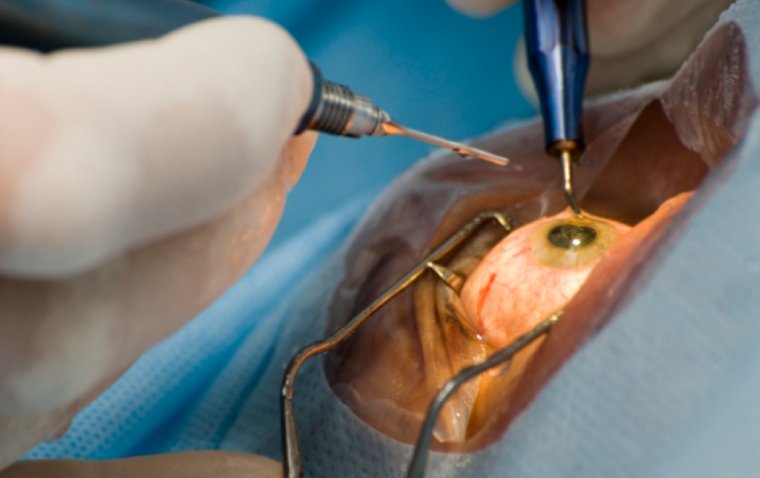
2. Slit Lamp Biomicroscopy: A slit lamp is a specialized microscope that allows the doctor to examine the cornea in detail. They will focus a high-intensity beam of light onto the cornea, enabling them to identify areas of staining.
3. Fluorescein Staining: Fluorescein is a special dye that is applied to the eye's surface. It adheres to damaged or irregular areas on the cornea, causing them to fluoresce under a blue light. This highlights areas of staining, making them easier to detect.
4. Diagnostic Tests: In addition to clinical examination, your eye care professional may use specific diagnostic tests to assess the extent and underlying causes of corneal staining:
5. Schirmer's Test: This measures tear production to determine if dry eyes are contributing to corneal staining. It involves placing small strips of filter paper under the lower eyelid to assess tear volume.
6. Tear Break-Up Time (TBUT): TBUT measures how long it takes for a tear film to break up after a blink. A shorter TBUT may indicate issues with tear film stability and dry eye syndrome.
7. Corneal Topography: This advanced imaging technique creates a detailed map of the cornea's surface, helping to identify irregularities and assess the extent of staining.
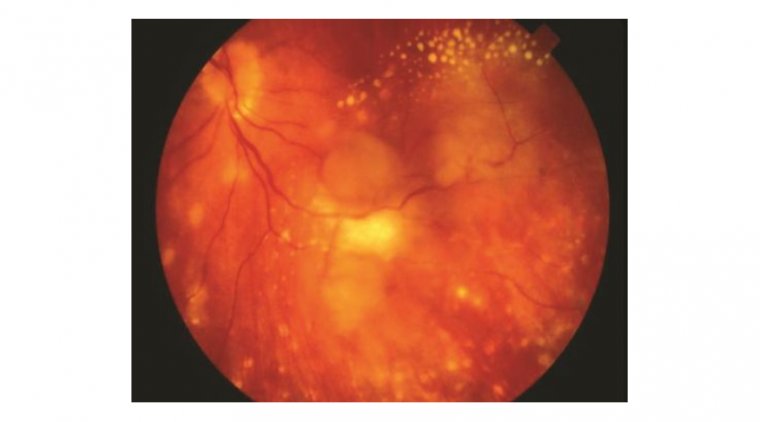
8. Inflammatory Biomarkers: In cases of corneal staining related to inflammation or autoimmune conditions, specific biomarker tests may be conducted to identify the underlying cause.
How is Corneal Staining Treated?
Medical Management
● Artificial Tears and Lubricating Eye Drops: Lubricating eye drops, such as artificial tears, are often the first line of treatment. They help maintain a healthy tear film, reducing friction and irritation on the cornea. Some formulations also contain electrolytes to support corneal healing.

● Prescription Eye Drops: In cases of severe dry eye or corneal inflammation, ophthalmologists may prescribe medicated eye drops, such as corticosteroids or cyclosporine, to reduce inflammation and improve tear production.
● Punctal Plugs: Punctal plugs are tiny devices inserted into the tear ducts to block drainage temporarily. This keeps more natural tears on the ocular surface, aiding in the healing of corneal staining.
● Oral Medications: Inflammatory or autoimmune-related corneal staining may require oral medications to manage the underlying condition.
10 Tips to Prevent Corneal Staining
1. Maintain Proper Hydration
● Staying adequately hydrated helps ensure your body can produce an adequate quantity of tears. Aim to drink enough water throughout the day.
2. Follow Good Contact Lens Hygiene
● If you wear contact lenses, adhere to your eye care professional's recommendations for cleaning, disinfecting, and replacing your lenses. Avoid wearing lenses longer than advised.
3. Take Breaks from Digital Screens
● If you work on a computer or spend extended periods looking at screens, practice the 20-20-20 rule: every 20 minutes, take a 20-second break to look at something 20 feet away. Blink frequently during screen time.
4. Use Humidifiers
● In dry indoor environments, especially during the winter, using a humidifier can add moisture to the air, reducing the likelihood of dry eyes and corneal staining.
5. Protect Your Eyes from Harsh Environments
● Wear wraparound sunglasses or protective eyewear when exposed to windy, smoky, or dusty environments. This shields your eyes from irritants and reduces the risk of corneal staining.
6. Avoid Smoking and Secondhand Smoke
● Smoking and exposure to secondhand smoke can worsen dry eye symptoms and contribute to corneal staining. Quitting smoking or avoiding smoke-filled areas can help.
7. Use Preservative-Free Eye Drops
● When using artificial tears or lubricating eye drops, opt for preservative-free formulations. Some preservatives can exacerbate eye irritation.
8. Regular Eye Exams
● Schedule routine eye check-ups with an optometrist or ophthalmologist, especially if you are prone to dry eyes or other eye conditions. Early detection and management can prevent corneal staining from worsening.
9. Nutritious Diet
● A diet rich in omega-3 fatty acids, found in fish and flaxseed, can support eye health and reduce dry eye symptoms. Discuss dietary changes with a healthcare professional.
10. Blink Regularly
● Pay attention to your blinking patterns, especially when using digital devices. Make a conscious effort to blink regularly to spread tears evenly across the cornea.
Summary
In summary, corneal staining is a condition that can significantly impact eye health and comfort. Understanding its causes, symptoms, and preventive measures is crucial for maintaining clear and healthy eyes.
Remember to:
● Stay hydrated and maintain good contact lens hygiene.
● Take breaks from digital screens and use humidifiers in dry environments.
● Protect your eyes from harsh elements and avoid smoking and secondhand smoke.
● Use preservative-free eye drops and prioritize regular eye exams.
Incorporating these practices into your daily routine can help prevent corneal staining and maintain your eye health. If you experience persistent eye symptoms, don't hesitate to consult an eye care specialist for a thorough evaluation. Your eyes deserve the best care possible.
(1).jpg)