Postmenopausal Women - Dry Eye Disease & Estradiol Drops
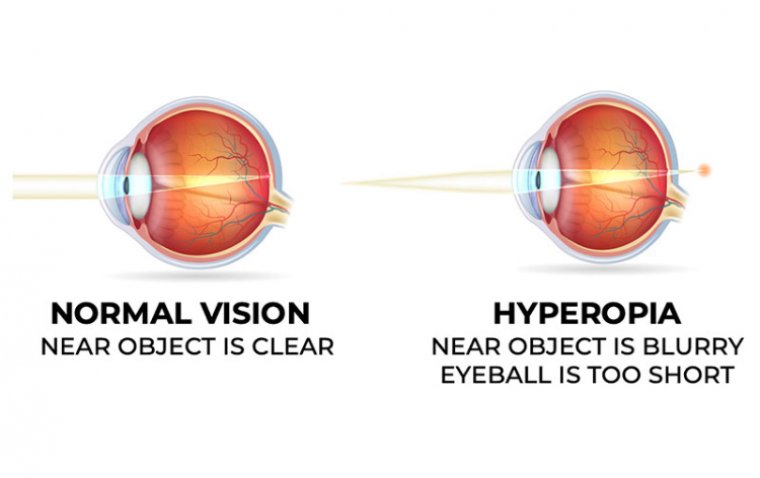
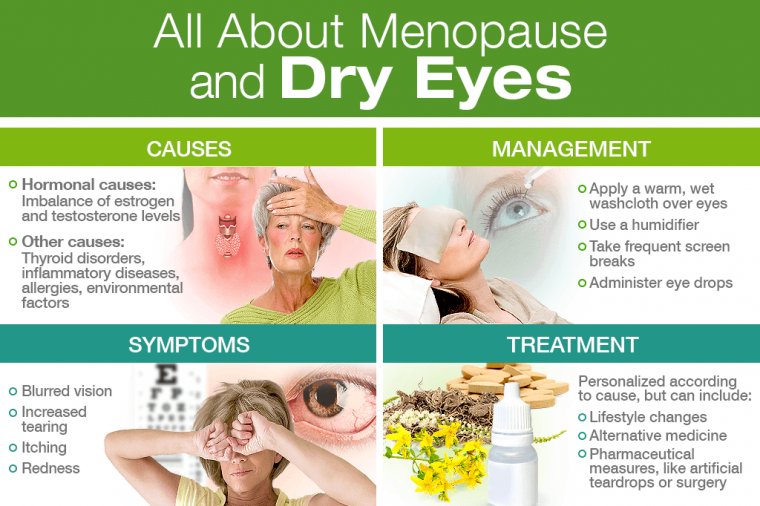
A common ocular problem is dry eye syndrome. Women are more likely to acquire dry eye syndrome and its accompanying detrimental implications on their general eye health, especially menopausal women with comorbidities.
One of the most common ocular disorders is dry eye syndrome, which can have a significant negative impact on a patient's quality of life, particularly in the elderly. Dry eye problems might be greatly influenced by menopause.
Dry eyes affect about 61 percent of perimenopausal and menopausal women.
Dry eyes are a common menopause side effect for many women. Hot flashes, night sweats, insomnia, and even sadness are just a few of the painful symptoms that can occur during menopause due to the body's decreased production of androgen, estrogen, and progesterone.
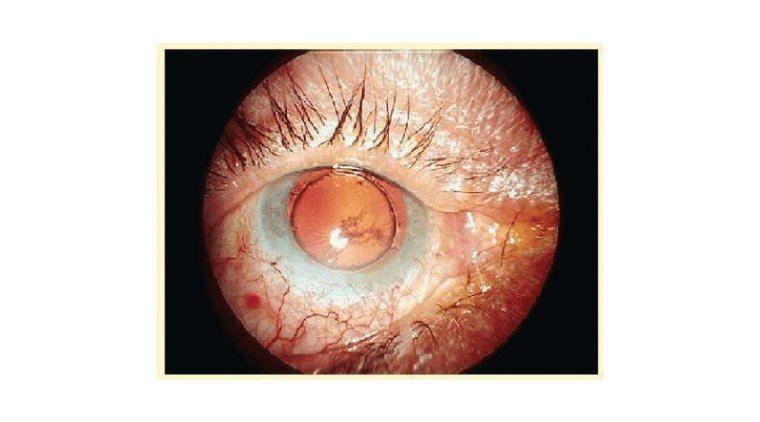
During menopause, the androgen hormone decreases, affecting the meibomian and lacrimal glands in the eyelids.
When these oil and fluid producing glands are affected, the eyelids can become inflamed, reducing tear production and tear quality— consequently leading to dry eyes.
Some researchers believe that changes in estrogen levels are also linked to dry eye. This may be the reason for an increase in dry eye symptoms during certain times of your monthly cycle, or while taking birth control pills.
Hormone Replacement Therapy
Hormone replacement therapy is prescribed for the treatment of many uncomfortable menopausal symptoms.
Although both low and high estrogen levels have been associated with symptoms of dry eye disease, low androgen levels are a more consistent factor in its etiology.
Postmenopausal HT with estrogen or estrogen plus progestogen has shown a limited benefit for dry eye symptoms and may even result in progression of meibomian gland dysfunction, decreased tear film break up time, and tear flow reduction.
However, systemic or local androgen treatment has shown promising results in improving dry eye symptoms.
Because of the high incidence of dry eye among postmenopausal women that may be related to the hormonal treatment, a multidisciplinary approach should be considered between gynecologists and ophthalmologists in management of this disorder.
The women who receive hormone replacement therapy (HRT), especially with unopposed estrogen therapy, have an increased risk of dry eye syndrome. Although they found no medical conditions to have a confounding impact, they did not consider rosacea in the list of confounding conditions.
Clinically significant rosacea occurs in approximately 30% of menopausal women. The diagnosis of rosacea is based on the finding of persistent erythema, prominent telangiectases, and papulopustules of the cheeks, chin, and forehead.
Easy flushing or blushing due to physical exertion or consumption of hot beverages is also characteristic. Noticeably lacking are the comedones that characterize acne vulgaris.
The failure to include rosacea as a confounding condition is significant because of the coexistence of this cutaneous condition with ocular rosacea. Ocular rosacea is a common cause of dry eye or keratoconjunctivitis sicca.
While the incidence of ocular rosacea is not known, it may be present in as many as 58% of patients with rosacea and has been suggested to be present in up to 75% of perimenopausal women with facial rosacea.
Another study found all patients with cutaneous rosacea to have some degree of ocular involvement. Common symptoms of ocular rosacea include irritation and dryness, the same 2 symptoms assessed by Schaumberg et al.
A novel treatment for dry eye disease (DED) in the form of a topical formulation of estradiol drops can reduce signs and symptoms of DED in postmenopausal women for at least 3 months.
Sex hormone receptors or estrogen receptors have been found to be present on the ocular surface in several tissues, such as the conjunctiva, cornea, and Meibomian glands.
The pronounced contrast in dry eye prevalence between men and women, especially women who are postmenopausal, points toward an involvement of sex hormones in the disease process.
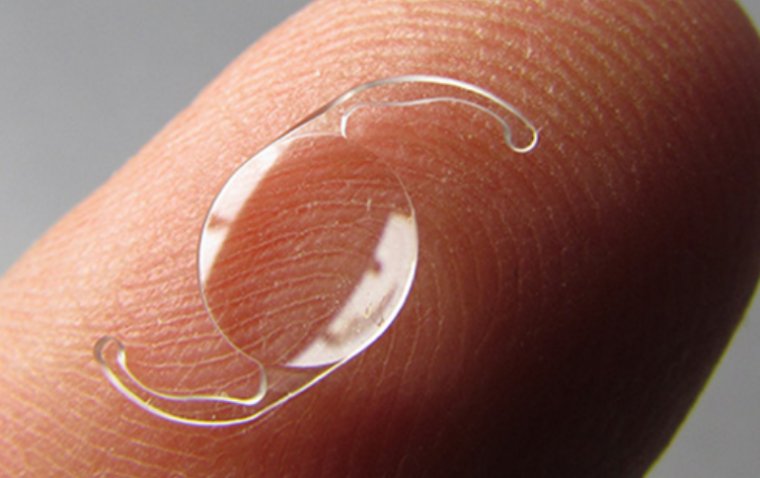
Furthermore, antiestrogen treatment seems to disrupt tear production. The therapeutic formulation used in the randomized, controlled, parallel-group study was RP101, which contains 17-beta-estradiol as the active ingredient and a sterile isotonic thermogelling (IntelliGel) solution as the drug delivery system.
This thermosensitive, supramolecular hydrogel becomes a gel at eye temperature, allowing for a long period of residency on the ocular surface and thus permitting sustained drug delivery.
The study aimed to determine the optimal dose regimen of RP101 and to evaluate its safety in postmenopausal women with moderate-to-severe DED.
The 4 arms of the study included 0.05% twice daily, 0.1% morning and vehicle (isotonic thermogelling solution) in the evening, 0.1% twice daily, and a control group who received the vehicle twice daily.
The treatment period was 3 months. Investigators used Schirmer Test II and grading of corneal fluorescein staining, taking measurements at baseline and at various points during treatment: day 14, day 30, day 60, and day 90 (treatment completion).
Patients reported outcomes for various DED symptoms via the Symptom Assessment Questionnaire iN Dry Eye (SANDE) and the visual analog scales (VAS). Investigators enrolled 104 patients in the study, with 77 completing the study according to the protocol.
Five patients requested withdrawal, 21 withdrew due to adverse events, and 1 withdrew for other reasons. Corneal fluorescein staining score significantly decreased during the 3-month treatment period (P < 0.001 vs baseline).
Investigators found no significant difference between treatment groups. The staining of the inferior cornea, however, showed a significantly more pronounced reduction in the highest dose group compared to vehicle, P = 0.0463.
The Schirmer II Test showed an increase in tear production, reaching maximum effect after 90 days of treatment.
Schirmer Test II increased significantly after 14 days of treatment in the active groups and after one month of treatment in the control group and remained significantly elevated until the end of the study.
The SANDE symptom score, a frequently used standardized questionnaire for the assessment of severity and frequency of dry eye symptoms, showed a decrease at the end of the treatment period in all groups.
Moreover, patient-reported outcome via VAS in all four treatment arms showed a decrease in symptoms of DED, such as foreign body sensation, burning/stinging, itching, pain, sticky feeling, redness, and tearing.
The topical RP101 eye drops were well tolerated on the ocular surface and showed a favorable safety profile. Most treatment-related adverse events were eye related and mostly mild or moderate.
The most frequent adverse events (more than 5% in at least 1 treatment group) were blurred vision, eye pain, eye irritation, ocular hyperemia, eyelid swelling, or foreign body sensation.
All these adverse events had resolved at the end of the study. At this time, therapy data are limited to use in postmenopausal women.
Further studies are needed to investigate whether other target populations would benefit from topical estrogen treatment. The next step will be a phase 3 study, with a larger population than that in phase 2, the basis of which will be the data obtained from the phase 2 study.
The data show that all dosages of RP101 were safe and improved signs and symptoms of DED at the end of the observation period.
The topical approach would make the most sense in dry eye patients, as it can reach higher levels on the ocular surface while not needing high plasma levels, which would be the case when estrogen is given systemically.
The thermosensitive hydrogel solution, which served as a control in the study, also had an impact on signs and symptoms of DED.
Systemic estrogen is not a preferred option to treat DED in postmenopausal women because it has been linked to serious systemic adverse effects in patients.
(1).jpg)