Ocular Inflammation: Types, Causes, Diagnosis, and Treatment
Ocular inflammation is a critical eye condition that can lead to discomfort, impaired vision, and, if left untreated, long-term damage to your eyesight. This comprehensive guide explores what ocular inflammation is, its various types, common causes, diagnostic procedures, its connection with immunology, available treatments, and preventative measures to manage and reduce symptoms.
Ocular Inflammation: Causes and Insights
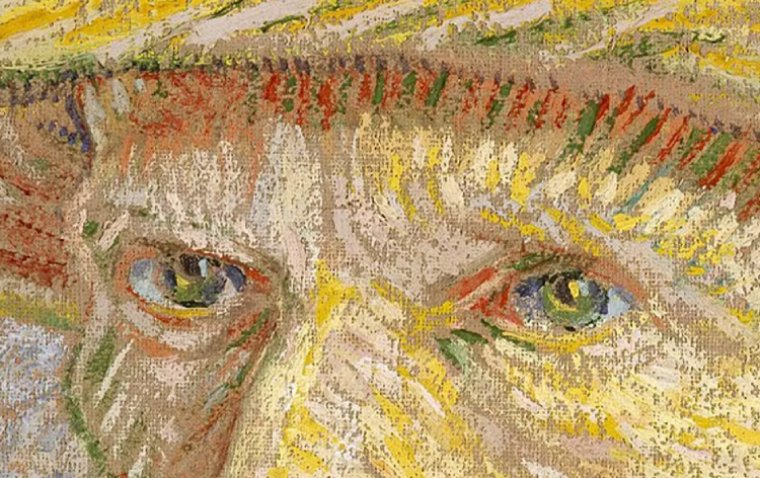
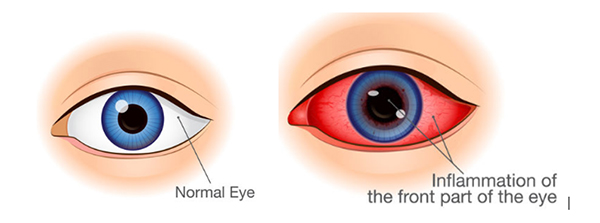
Ocular inflammation refers to the inflammation of one or more parts of the eye. It is characterized by swelling, redness, pain, and sometimes a decrease in vision. This condition can affect various parts of the eye, including the uvea (uveitis), iris (iritis), and conjunctiva (conjunctivitis), among others. Ocular inflammation can be acute or chronic and may affect one or both eyes.
Types of Ocular Inflammation
1. Uveitis: Inflammation of the uvea, the middle layer of the eye.
2. Iritis: A type of uveitis that specifically affects the iris.
3. Scleritis: Inflammation of the sclera, the white outer wall of the eye.
4. Episcleritis: Inflammation affecting the episclera, a thin layer of tissue between the conjunctiva and sclera.
5. Keratitis: Inflammation of the cornea, the eye's front surface.
What Causes Ocular Inflammation?
Ocular inflammation can be triggered by a variety of factors, including:
● Infections: Caused by bacteria, viruses, fungi, or parasites.
● Autoimmune Disorders: Such as rheumatoid arthritis, lupus, and sarcoidosis, where the body's immune system attacks its own tissues.
● Injury: Physical trauma to the eye.
● Allergies: Reactions to allergens such as pollen, dust, or pet dander.
● Environmental Factors: Exposure to chemicals, pollutants, or UV light.
How to Diagnose Ocular Inflammation
Diagnosing ocular inflammation requires a thorough examination by an eye care professional to identify the underlying cause and determine the most appropriate treatment. Here's a more detailed look at the diagnostic process:
1. Visual Acuity Test
The visual acuity test is a preliminary assessment that measures how well you can see the details of a letter or symbol from a specific distance. It's often conducted using a chart with rows of letters that decrease in size. This test helps determine the impact of ocular inflammation on your vision, highlighting any immediate effects on your ability to see clearly. A significant change in visual acuity might indicate the presence of inflammation or other abnormalities within the eye.
2. Slit Lamp Examination
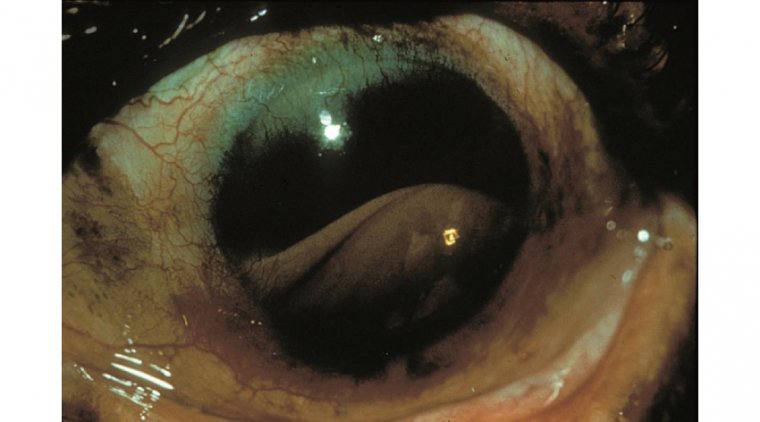
A slit lamp examination allows the eye care professional to examine the various structures of the eye under high magnification and illumination. During this examination, a slit lamp (a microscope combined with a bright light) is used to illuminate the front part of the eye, including the cornea, iris, and lens. This detailed inspection can reveal signs of inflammation, such as swelling, redness, or abnormal cells in the aqueous humor. The slit lamp examination is crucial for diagnosing specific types of ocular inflammation, such as uveitis and keratitis.
3. Ophthalmoscopy
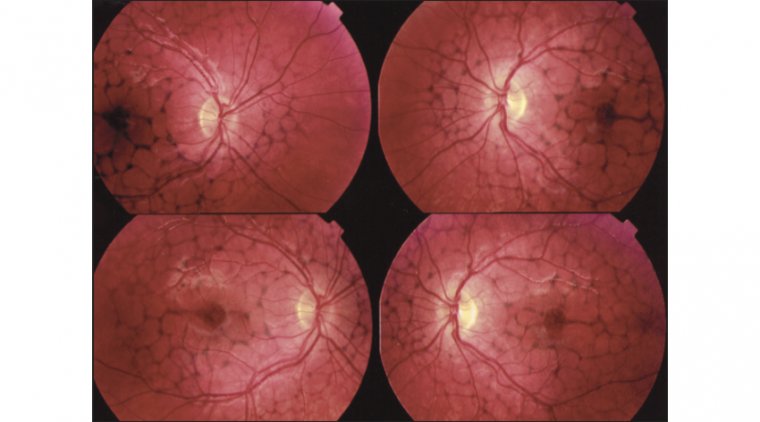
Ophthalmoscopy, also known as fundoscopy, is a procedure used to examine the back of the eye, including the retina, optic nerve, blood vessels, and vitreous humor. This examination can be performed using a direct or indirect ophthalmoscope, which shines a light through the pupil to visualize the internal structures. Ophthalmoscopy helps detect signs of inflammation at the back of the eye, such as optic nerve swelling (papillitis), retinal vasculitis, or lesions on the retina, which are critical for diagnosing conditions like posterior uveitis.
4. Laboratory Tests
In addition to these eye-specific tests, laboratory tests can play a vital role in diagnosing ocular inflammation. Blood tests, for example, can detect markers of inflammation, autoimmune diseases, or infections that might be causing or contributing to the ocular condition. Depending on the suspected cause, specific tests for conditions like rheumatoid arthritis, sarcoidosis, or Lyme disease may be recommended. In cases where an infectious agent is suspected, cultures or polymerase chain reaction (PCR) tests from ocular samples might be performed to identify the responsible pathogen.
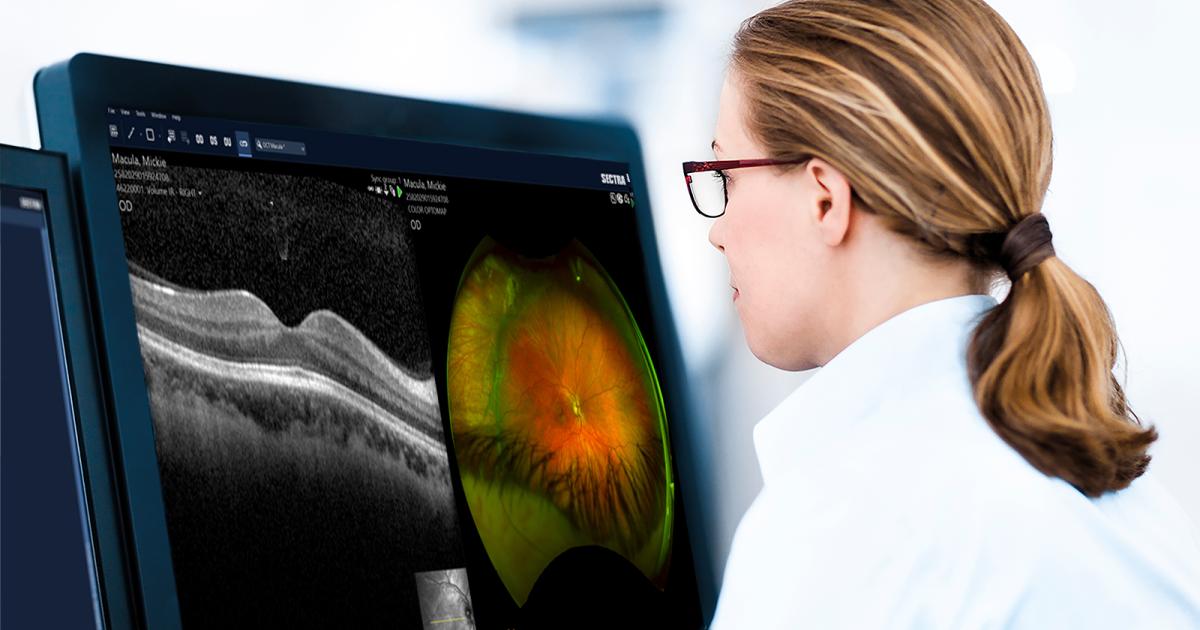
5. Imaging Studies
Imaging studies, such as optical coherence tomography (OCT), fluorescein angiography, or ultrasound (B-scan), may also be used to provide detailed images of the eye's structures. OCT offers cross-sectional images of the retina, revealing any swelling or abnormalities. Fluorescein angiography involves injecting a dye into the bloodstream and taking photographs as the dye passes through the blood vessels in the eye, highlighting any blockages or leaks that could indicate inflammation. Ultrasound imaging can be helpful in cases where the view of the back of the eye is obstructed by opacities in the cornea or lens.
By combining these diagnostic tools and tests, eye care professionals can accurately diagnose ocular inflammation, determine its severity, and identify the underlying causes, guiding the development of an effective treatment plan.
Treatment for Ocular Inflammation
1. Medications: Steroids and Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Steroids (corticosteroids) and NSAIDs are pivotal in reducing ocular inflammation. Steroids can be administered in various forms, including eye drops, oral medications, or injections, depending on the inflammation's severity and location. They work by suppressing the immune system's response, thereby reducing inflammation and swelling. However, long-term use of steroids can have side effects such as increased intraocular pressure, leading to glaucoma, and cataract formation. Therefore, their use is closely monitored by healthcare professionals.
NSAIDs, on the other hand, are often used for milder cases of inflammation and can also be administered as eye drops or oral medications. They work by inhibiting enzymes that contribute to the inflammatory process, offering pain relief and reducing swelling without the steroid-associated risks.
2. Antibiotics or Antiviral Agents
Infections caused by bacteria or viruses are common triggers for ocular inflammation. Identifying the causative agent is crucial for determining the appropriate treatment. Antibiotics are prescribed to combat bacterial infections and can be administered as eye drops, ointments, or systemic medications, depending on the infection's severity and location. Antiviral agents are used to treat viral infections, such as herpes simplex virus, and can significantly reduce the risk of complications when used promptly. The choice between antibiotics and antivirals depends on diagnostic tests that identify the pathogen.
3. Immunosuppressive Agents
For ocular inflammation stemming from autoimmune diseases, where the body's immune system mistakenly attacks its own cells, immunosuppressive agents may be prescribed. These drugs, including methotrexate, azathioprine, and cyclosporine, work by dampening the overall immune response, thereby reducing inflammation. They are particularly useful in managing chronic conditions and are often considered when steroids are ineffective or their side effects become a concern. The use of these medications requires careful monitoring for potential side effects, such as increased susceptibility to infections.
4. Surgery
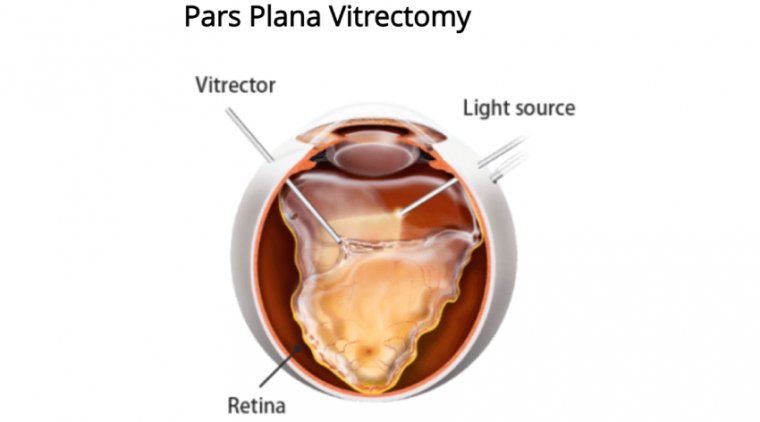
Surgical intervention may be necessary in severe cases of ocular inflammation, especially when there is structural damage to the eye or when other treatments have failed. Surgical procedures might include:
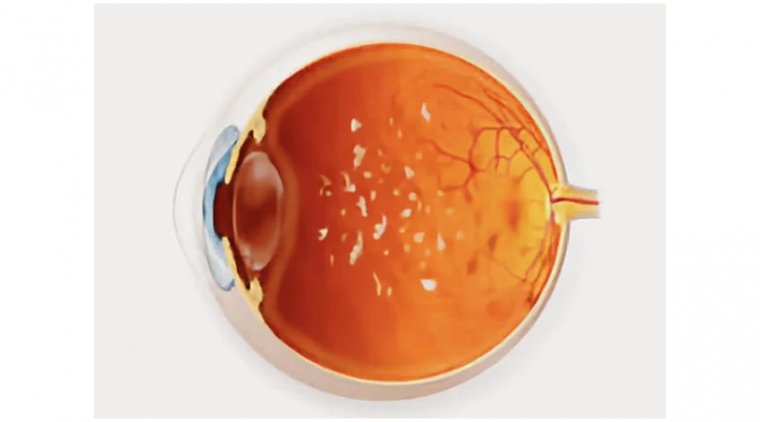
● Vitrectomy: Removal of the vitreous humor (the clear gel that fills the eye between the lens and the retina) to eliminate inflammatory debris and reduce the load of infectious or inflammatory agents.
● Repair of Structural Damages: In cases where inflammation has led to complications such as retinal detachment or severe corneal damage, surgery may be required to repair these structures and restore vision.
Surgery is considered a last resort due to the risks involved, but it can be life-changing for patients with severe ocular inflammation, offering a chance to preserve or improve vision.
How Do You Reduce the Risk of Ocular Inflammation?
Preventative measures and lifestyle adjustments can help manage and reduce the risk of ocular inflammation:
Protect Your Eyes: Use safety glasses to prevent injuries and sunglasses to shield your eyes from UV rays.
Maintain Good Hygiene: Wash your hands regularly and avoid touching your eyes with unclean hands.
Control Environmental Factors: Use air purifiers to reduce allergens and maintain a clean environment.
Healthy Diet and Supplements: Nutrients like omega-3 fatty acids, vitamin C, and vitamin E can support eye health.
Conclusion
Ocular inflammation is a condition that requires prompt attention to prevent potential vision loss. Understanding the types, causes, and treatment options is the first step toward effective management. If you experience symptoms of ocular inflammation, consulting an eye care professional is essential for accurate diagnosis and appropriate treatment. With proper care, most individuals can recover from ocular inflammation without lasting effects on their vision.
(1).jpg)