Trabeculectomy: A Comprehensive Guide to Understanding the Procedure and Recovery
What is Trabeculectomy?
Trabeculectomy is a surgical procedure primarily used to treat glaucoma, a group of eye conditions characterized by damage to the optic nerve, often due to abnormally high pressure in the eye. As one of the most commonly performed surgeries for glaucoma, trabeculectomy aims to lower intraocular pressure and subsequently minimize further optic nerve damage and potential vision loss.
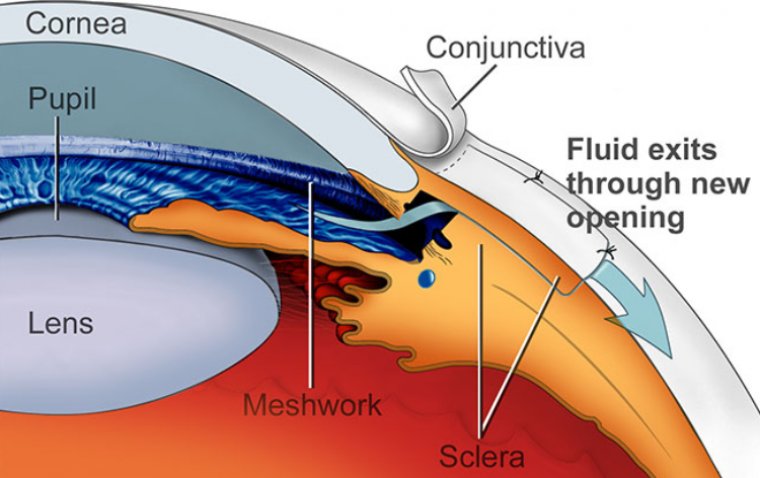
The procedure involves creating a small hole in the eye's white part (the sclera), covered by a thin trap-door in the sclera. The fluid inside the eye, known as aqueous humor, drains through the hole to a small reservoir or bleb just under the eye surface, in the conjunctiva (the clear skin covering the sclera). From here, the fluid is absorbed into the bloodstream. This process helps to lower the intraocular pressure.
Trabeculectomy is usually considered when other treatments, such as eye drops or laser procedures, have failed to control the eye pressure adequately, or if the pressure needs to be lowered significantly. The operation is typically performed under local anesthesia and requires a short hospital stay.
Types of Glaucoma Suitable for Trabeculectomy
Trabeculectomy is typically employed for treating various types of glaucoma where other treatments have not effectively controlled intraocular pressure or in cases where significant reduction of the eye pressure is required. Here are the types of glaucoma that can be effectively managed with trabeculectomy:
1. Open-Angle Glaucoma: This is the most common type of glaucoma, where the drainage angle formed by the cornea and iris remains open, but the trabecular meshwork is partially blocked, causing an increase in eye pressure.
2. Chronic Angle-Closure Glaucoma: In this form, the iris bulges forward, narrowing or blocking the drainage angle formed by the cornea and iris, leading to a slow rise in eye pressure. Trabeculectomy is often performed when medication and laser procedures are insufficient to control eye pressure.
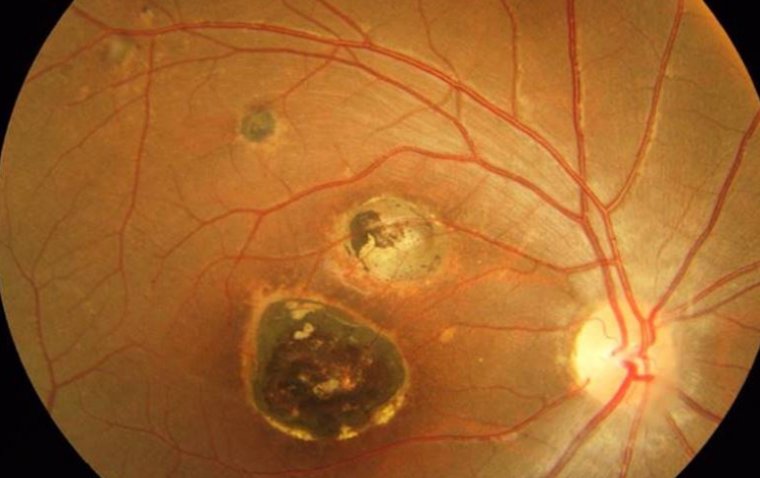
3. Neovascular Glaucoma: This is a type of secondary glaucoma, often linked to diabetes or certain types of retinal vascular diseases. It is typically aggressive and resistant to treatment, often requiring procedures like trabeculectomy.
4. Congenital Glaucoma: Though not as common, trabeculectomy can be employed for treating congenital glaucoma (present from birth) if other surgical interventions aren't successful.
5. Secondary Glaucoma: Trabeculectomy can also be useful for secondary glaucoma types that result from injury or other eye diseases.
Benefits and Risks of Trabeculectomy
The primary benefit of trabeculectomy is its potential to substantially reduce intraocular pressure (IOP), often to a level that is not achievable with medication or laser treatment alone. By creating a new drainage pathway, the procedure helps in controlling IOP, slowing the progression of glaucoma, and preserving vision. The long-term success rate of trabeculectomy is quite promising, with studies reporting controlled IOP in a significant proportion of patients several years post-surgery.
However, like any surgical procedure, trabeculectomy carries certain risks. The most common complications include over-filtration or under-filtration, where too much or too little fluid is drained, respectively. Over-filtration can result in extremely low IOP or hypotony, potentially causing vision problems. In contrast, under-filtration could fail to sufficiently lower IOP, necessitating additional treatment.
Other potential complications include infection, cataract development, and changes in refractive error, which might lead to a need for glasses or a change in the current prescription. In rare cases, serious complications like retinal detachment or loss of vision can occur. Bleb-related complications, including leaks or infections, are also possibilities and need close monitoring.
It's crucial that patients are well-informed of both the potential benefits and risks associated with trabeculectomy. They should have open discussions with their healthcare providers to make an informed decision regarding their treatment options. Personalized treatment planning and diligent postoperative care can help minimize these risks and optimize outcomes.
Preparing for Trabeculectomy Surgery
Preparation for trabeculectomy surgery is a vital aspect that ensures a safe and effective procedure. In the days or weeks leading up to the surgery, your ophthalmologist will conduct a comprehensive eye examination to assess the overall health of your eyes and the severity of your glaucoma. This may include tests such as visual field testing, optical coherence tomography (OCT), and tonometry to measure your intraocular pressure.
Patients are usually asked to fast (avoid eating or drinking) for a certain number of hours before surgery. This is a standard precaution for many types of surgeries to prevent any complications during anesthesia. Your surgeon will provide you with specific instructions based on your health status and the type of anesthesia to be used.
Moreover, it's crucial to discuss with your surgeon about any medications you're currently taking, including over-the-counter drugs, supplements, or herbal remedies, as some of these may need to be adjusted or stopped temporarily. Medicines like blood thinners can increase the risk of bleeding during surgery, while certain eye drops may need to be paused prior to the procedure.
Lastly, arranging for a family member or friend to accompany you to the clinic or hospital on the day of the surgery is recommended. This is because you will not be able to drive immediately following the procedure due to the temporary effects of the anesthesia.
Understanding the Trabeculectomy Procedure
Trabeculectomy is a complex surgical procedure designed to alleviate intraocular pressure caused by glaucoma. The surgery usually takes about an hour to complete and is often performed under local anesthesia, ensuring that the patient is awake but feels no pain. For some patients, sedation or even general anesthesia might be administered based on their health status or personal preference.
The process begins with the surgeon making a tiny incision in the conjunctiva (the clear tissue covering the white part of the eye) and creating a partial-thickness flap in the sclera, which is the white outer layer of the eye. This scleral flap serves as a sort of valve, controlling the amount of fluid that can flow out of the eye.
Next, the surgeon makes a small hole in the eye under the scleral flap, which leads to the anterior chamber of the eye - the space between the iris (the colored part of the eye) and the cornea (the eye's clear front surface). This hole is the new drainage channel, allowing the excess fluid to escape, thereby reducing intraocular pressure.
The scleral flap is then sutured back into place in a way that allows it to lift slightly, creating a passage for fluid to flow out of the eye and into a small reservoir or bleb formed under the conjunctiva. This fluid will eventually be absorbed into the bloodstream.
Overall, the goal of the trabeculectomy procedure is to create a new pathway for fluid to exit the eye, helping to lower the intraocular pressure and prevent further damage to the optic nerve, which is crucial for maintaining good vision.
Postoperative Recovery and Care
The recovery period following a trabeculectomy surgery is a critical time during which the eye is given the opportunity to heal and the desired reduction in intraocular pressure is achieved. It is normal for the eye to feel irritated or sensitive for a few days after the procedure. Mild discomfort, blurry vision, and the appearance of floaters (spots or specks drifting in your field of vision) are common experiences during this time.
Following the surgery, the surgeon will typically apply a patch or shield over the eye to protect it from injury. Patients are usually advised to rest and avoid any strenuous activities. Reading, watching TV, or using a computer are generally permitted, but activities that might strain the eyes or increase pressure, such as bending over or lifting heavy objects, should be avoided.
It's essential to keep all follow-up appointments with your ophthalmologist so that they can monitor your healing process, check the intraocular pressure, and adjust medications as necessary. These visits are crucial for minimizing complications and ensuring the success of the procedure. Your doctor will give you detailed instructions regarding postoperative care, which might include using specific eye drops to control inflammation and prevent infection.
In the weeks following the procedure, the operated eye should be protected from potential harm. This might include wearing an eye shield at night or during naps, avoiding rubbing or pressing on the eye, and refraining from swimming or using hot tubs to prevent infection.
Recovery time can vary from person to person, depending on their overall health, age, and the specific details of their procedure. Most patients will notice an improvement in their symptoms within a few weeks, but full recovery can take several months. Remember, the primary aim of trabeculectomy is to prevent further vision loss rather than to restore vision that has already been lost due to glaucoma.
Managing Complications and Risks After Trabeculectomy
Managing complications and risks after trabeculectomy is crucial in ensuring a successful recovery and the overall effectiveness of the surgery. Potential complications can range from mild and temporary to more severe and permanent, depending on various factors such as the patient's overall health, age, and the specific details of their procedure.
Mild complications may include temporary blurred vision, discomfort or irritation in the eye, and the presence of floaters. These usually resolve on their own or can be managed with prescribed medications.
More significant complications can include infection, excessive or insufficient drainage leading to changes in intraocular pressure, and in rare cases, loss of vision. Therefore, it's essential to promptly report any unusual symptoms or concerns to your eye doctor to prevent or mitigate these potential issues.
If infection occurs, it is typically treated with antibiotics. Changes in intraocular pressure may require additional medical or surgical interventions.
The most effective way to manage potential complications is through regular follow-ups with your ophthalmologist. These check-ups allow your doctor to monitor your recovery, assess the success of the surgery, adjust medications as needed, and address any emerging issues promptly.
Furthermore, adhering to postoperative care instructions, including taking prescribed medications, protecting the eye from injury, and avoiding activities that may strain the eye, can significantly reduce the risk of complications. Remember, early detection and prompt treatment are crucial in effectively managing complications and ensuring the best possible outcome after a trabeculectomy.
Summary
In conclusion, trabeculectomy plays a crucial role in managing glaucoma, particularly in cases resistant to medication or other less invasive treatments. By creating a new drainage pathway, it helps to lower intraocular pressure and thereby, prevent further optic nerve damage and vision loss.
We've explored the types of glaucoma suitable for trabeculectomy and the benefits and potential risks associated with the procedure. Remember, adequate preparation before surgery and following through with postoperative care instructions are essential steps toward ensuring a successful outcome.
Importantly, while trabeculectomy can effectively manage glaucoma, it also carries potential risks and complications. Regular follow-up visits with your ophthalmologist are imperative for monitoring your recovery, managing any complications, and adjusting treatment plans as necessary.
Ultimately, each patient's case is unique. Thus, a consultation with an ophthalmologist is critical for personalized treatment recommendations. An open and informed discussion about the benefits, risks, and alternative treatment options can help guide the best course of action for managing your glaucoma effectively. Stay informed, ask questions, and actively participate in your eye health care.
(1).jpg)