The Crucial Role of Corneal Hysteresis in Glaucoma Risk Assessment
What is Corneal Hysteresis?
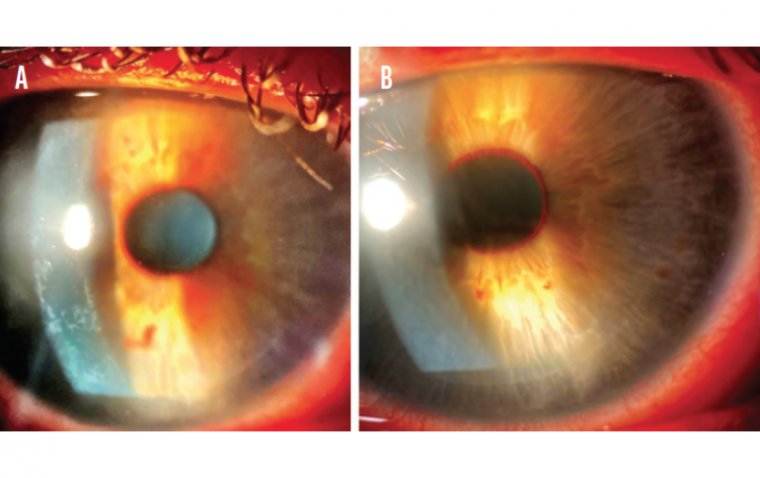
Corneal hysteresis is a measure of the cornea's ability to absorb and dissipate energy when subjected to stress, such as the pressure exerted within the eye. The cornea is the clear, dome-shaped front surface of the eye that covers the iris, pupil, and anterior chamber. It is a complex structure composed of layers of collagen fibers and cells. Corneal hysteresis reflects the cornea's viscoelastic properties, meaning its ability to both resist deformation and return to its original shape after deformation.
Corneal hysteresis is particularly relevant to eye health due to its association with glaucoma, a progressive eye disease that can lead to vision loss if left untreated. Glaucoma is often characterized by increased intraocular pressure (IOP), which can damage the optic nerve, resulting in vision loss. While IOP is a well-known risk factor for glaucoma, it is not the sole determinant of the disease. The ability of the cornea to resist deformation and its role in dissipating energy (corneal hysteresis) are equally important factors.
The Role of Corneal Hysteresis in Glaucoma Risk Assessment
While IOP has long been recognized as a key risk factor for glaucoma, it is now understood that CH plays a pivotal role in the assessment of glaucoma risk. Here's how:
1. Independent Risk Factor: CH is considered an independent risk factor for glaucoma. This means that even individuals with normal IOP levels can be at risk if they have low CH. Conversely, individuals with high CH may have a lower risk of developing glaucoma, even if their IOP is elevated. Therefore, CH provides additional insights into glaucoma risk beyond IOP.
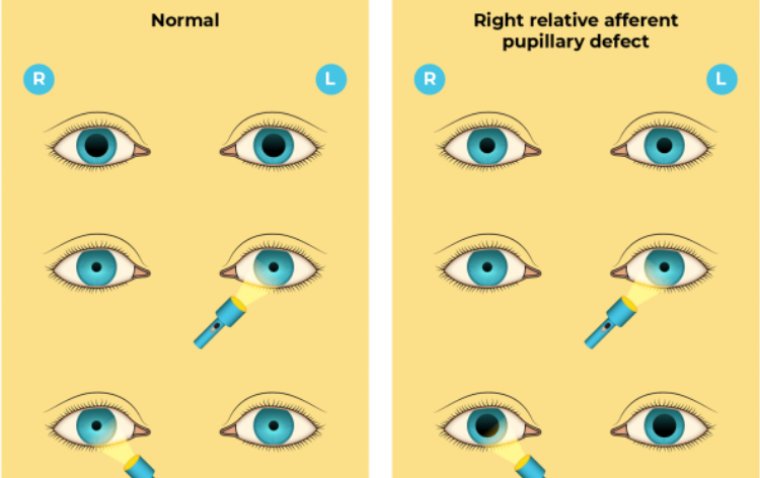
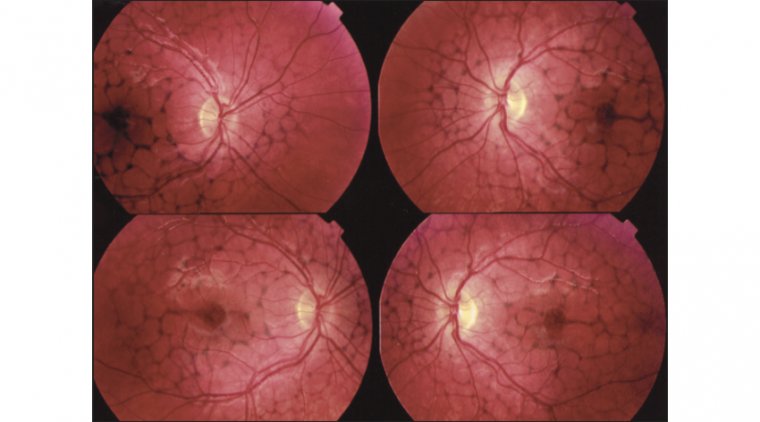
2. Optic Nerve Vulnerability: The optic nerve is the primary target of glaucomatous damage. Low CH is associated with increased susceptibility of the optic nerve to IOP-related damage. When the cornea has low hysteresis, it may transmit a higher proportion of the IOP-related stress to the optic nerve, potentially leading to optic nerve damage and vision loss.
3. Early Detection: CH measurements can aid in the early detection of glaucoma or progression of the disease. By incorporating CH into routine glaucoma assessments, eye care professionals can identify individuals at higher risk and initiate preventative measures or treatment at an earlier stage, potentially preserving vision.
4. Personalized Treatment: CH values can guide ophthalmologists in tailoring treatment plans for glaucoma patients. Patients with low CH may require more aggressive IOP-lowering treatments, while those with high CH may have a lower risk and may not need as intensive therapy.
5. Surgical Decision-Making: For individuals requiring glaucoma surgery, CH can influence the choice of surgical procedure. Some surgical techniques may be more suitable for patients with specific CH values, ensuring better surgical outcomes.
Correlation with Intraocular Pressure (IOP)
The correlation between Corneal Hysteresis (CH) and Intraocular Pressure (IOP) is a fundamental aspect of glaucoma risk assessment that has significantly reshaped our understanding of this sight-threatening disease. Traditionally, IOP has been the primary focus in assessing glaucoma risk, but the emergence of CH as an independent risk factor has brought new insights.
Low CH values are associated with heightened susceptibility to optic nerve damage from IOP-related stress. A cornea with low hysteresis is less adept at dampening IOP fluctuations, thus transmitting a higher proportion of pressure stress to delicate eye structures, including the optic nerve. This makes individuals with low CH more vulnerable to glaucomatous optic nerve damage, even when their IOP falls within the normal range. Conversely, those with high CH values appear to benefit from a protective effect against glaucoma. Their corneas can efficiently absorb and dissipate energy, reducing the transmission of IOP-related stress to the optic nerve. This suggests that even in cases of elevated IOP, individuals with high CH may have a reduced risk of optic nerve damage compared to those with low CH.
These findings have significant clinical implications. Incorporating CH measurements into routine glaucoma assessments enables the early detection of glaucoma risk, providing clinicians with valuable information to identify high-risk individuals, especially when IOP is within the normal range. CH values also guide ophthalmologists in tailoring treatment plans. Patients with low CH may require more aggressive IOP-lowering treatments to safeguard against optic nerve damage, while those with high CH may benefit from less intensive therapy.
Furthermore, when surgery is necessary, CH helps surgeons select the most suitable approach based on the patient's corneal biomechanics and IOP levels. In essence, understanding the correlation between CH and IOP enhances our ability to personalize glaucoma management, improve early detection, and optimize treatment strategies, ultimately preserving the vision and eye health of those at risk of glaucoma.
How to Measure Corneal Hysteresis
Corneal Hysteresis (CH) is a critical parameter in assessing glaucoma risk and understanding corneal biomechanics. To accurately measure CH, ophthalmologists and eye care professionals utilize specialized instruments and techniques designed for this purpose. In this article, we will explore the methods and tools commonly used for measuring CH, highlighting the key aspects of corneal hysteresis measurement.
1. Ocular Response Analyzer (ORA)
The Ocular Response Analyzer (ORA) is one of the most widely used instruments for measuring CH. It employs a patented technology called dynamic bidirectional applanation, which involves two precisely timed air puffs applied to the cornea. Here's how it works:
● Two Air Puffs: The ORA uses two rapid air puffs to deform the cornea, causing it to move inward and outward. These deformations are recorded by a high-speed infrared camera.
● Inward and Outward Movements: During the inward movement, the cornea first flattens and then returns to its original shape. The same process occurs during the outward movement. These deformation patterns provide information about the cornea's viscoelastic properties.
● CH Calculation: The ORA calculates CH by comparing the two applanation pressures during the inward and outward movements. The difference between these pressures is indicative of CH.

2. Corvis ST
The Corvis ST is another instrument used for measuring CH. It combines air puff technology with high-speed Scheimpflug imaging to assess corneal biomechanics. Here's how it works:
● Air Puff and Imaging: The Corvis ST delivers an air puff to deform the cornea while simultaneously capturing high-speed images of the entire process. The system records the cornea's deformation response in real-time.
● Deformation Parameters: The instrument calculates various corneal deformation parameters, including CH, which reflects the cornea's ability to absorb and dissipate energy.

3. Other Techniques
In addition to the ORA and Corvis ST, other techniques and instruments are used for CH measurement. These may include:
● Dynamic Biomechanical Analyzers: Some research-grade instruments are capable of assessing CH using dynamic biomechanical analysis. These systems can provide detailed insights into corneal properties.
● Supersonic Shearwave Imaging: This emerging technology uses ultrasound to assess corneal viscoelastic properties, including CH. It may offer a non-contact alternative for CH measurement.
Factors Affecting Corneal Hysteresis
Corneal Hysteresis (CH) is a vital parameter in assessing glaucoma risk and understanding corneal biomechanics. Various factors can influence CH measurements, and it's essential to consider these factors when interpreting CH values. In this article, we will explore some of the key factors affecting CH, including age, corneal thickness, and others.
1. Age
● Age is a significant factor influencing CH. Research has shown that CH tends to decrease with age. Younger individuals typically have higher CH values, indicating better corneal damping properties. As people age, their corneas may become stiffer, leading to reduced CH.
2. Corneal Thickness
● Corneal thickness plays a crucial role in CH measurement. Thicker corneas generally have higher CH values, as they have more material to absorb and dissipate energy. Conversely, thinner corneas tend to have lower CH values, as they are less capable of absorbing energy.
3. Corneal Rigidity
● Corneal rigidity or stiffness is an inherent property of the cornea. Eyes with stiffer corneas may exhibit lower CH values. This factor can be influenced by various corneal conditions, such as keratoconus or corneal scarring, which can alter the cornea's biomechanical properties.
4. Intraocular Pressure (IOP)
● The relationship between IOP and CH is complex. While IOP is a factor in CH measurement, it does not directly correlate with CH values. However, higher IOP can temporarily increase CH due to the stretching effect on the cornea. Therefore, CH values should be interpreted in the context of IOP measurements.
5. Gender
● Some studies suggest that gender may impact CH, with males tending to have slightly higher CH values than females. However, the clinical significance of this difference is relatively small and may not have a substantial impact on glaucoma risk assessment.
6. Ethnicity
● Ethnicity may also influence CH, with variations observed among different racial groups. Some research indicates that individuals of African descent may have lower CH values on average compared to individuals of European descent. However, this is a complex area of study, and further research is needed to fully understand these ethnic differences.
7. Genetic Factors
● Genetic factors likely contribute to the variation in CH values among individuals. Specific genes may influence corneal structure and biomechanics, affecting CH measurements. Research in this area is ongoing.
Summary
In summary, Corneal Hysteresis (CH) is a critical parameter in the field of ophthalmology, playing a pivotal role in assessing glaucoma risk and understanding the biomechanics of the cornea. Factors such as age, corneal thickness, corneal rigidity, intraocular pressure, gender, ethnicity, and genetics can influence CH measurements. Recognizing these factors is essential for interpreting CH values accurately and making informed clinical decisions.
For anyone concerned about their eye health or at risk of glaucoma, consulting with an eye care professional is strongly recommended. Eye care professionals have the expertise and tools necessary to measure CH and provide personalized insights into its implications for your eye health. Whether it's for early glaucoma detection, treatment planning, or general eye care, your eye care provider can offer valuable guidance to ensure the best possible outcomes for your vision.
FAQ
Corneal hysteresis (CH) is a measure of the cornea's ability to absorb and release energy during deformation. It is an important parameter in assessing the biomechanical properties of the cornea.
(1).jpg)