2024 Recap: Top 10 Breakthroughs in Ophthalmology Research
2024 has been a landmark year for breakthroughs in ophthalmology research, showcasing transformative advancements that are shaping the future of eye care. From novel therapeutic strategies to innovative technologies, these discoveries are pushing the boundaries of science, offering hope and improved outcomes for millions of patients worldwide.
Explore the top 10 research breakthroughs revolutionizing ophthalmology:
1. Breakthrough Study Reveals Promising Treatment for Corneal Endothelial Disease
.jpg)
A groundbreaking study published in The American Journal of Pathology by researchers at Mass Eye and Ear, part of the Harvard Medical School Department of Ophthalmology, has introduced an innovative therapeutic strategy to address corneal degeneration and disease. The study highlights the use of the neuropeptide α-melanocyte–stimulating hormone (α-MSH), demonstrating its potential to promote corneal healing and restore normal eye function.
The research focused on the local administration of α-MSH in a well-established model of injury-induced endothelial decompensation. The treatment showed promising effects, including:
• Reduction of persistent corneal edema.
• Regeneration of corneal endothelium.
By activating the melanocortin pathway, α-MSH offers a novel approach to treating corneal damage and dysfunction.
These findings underscore the significant potential of α-MSH in transforming the treatment landscape for corneal conditions, opening new possibilities for innovative and effective ocular therapies.
2. New Experimental Drug Shows Promise in Treating Diabetic Macular Edema
.jpg)
A recent study published in Nature Medicine reveals encouraging findings for a potential breakthrough in treating Diabetic Macular Edema (DME). The study highlights a novel class of therapeutics known as senolytics, which could revolutionize treatment outcomes with more effective and longer-lasting solutions.
Developed by UNITY Biotechnology, based in San Francisco, in collaboration with the Maisonneuve-Rosemont Hospital Research Center, affiliated with Université de Montréal, the experimental drug UBX1325 (foselutoclax) has demonstrated significant promise.
Key Insights:
• Effective in patients with poor responses to standard DME treatments.
• Offers potential for improved therapeutic outcomes in a condition that remains challenging to manage.
This innovative approach positions UBX1325 as a potential game-changer in managing DME, providing hope for patients with limited options and enhancing the future of ocular therapies.
3. Novel Gene Editing Method Shows Promise in Treating Genetic Eye Disorders
.jpg)
Researchers at the Broad Institute of MIT and Harvard have achieved a major advancement in gene editing technology, introducing a novel method to deliver prime editing tools into the cells of living animals. This breakthrough, published in Nature Biotechnology, leverages engineered virus-like particles (eVLPs) to transport prime editors with remarkable efficiency, offering new hope for treating genetic disorders.
Highlights of the Research
• Enhanced Prime Editing Efficiency:
By adapting eVLPs, originally developed to carry base editors, researchers significantly improved the delivery and effectiveness of prime editing tools in living organisms.
• Application in Genetic Blindness:
Using this method, scientists successfully corrected mutations in mouse models of genetic blindness, achieving partial restoration of vision.
• Safe and Precise Editing:
Demonstrated safe application in the mouse brain with no detectable off-target effects, underscoring its potential for therapeutic use.
Prime editing, celebrated for its capacity to correct a wide range of disease-causing genetic mutations, has now been validated in living organisms. This innovative delivery method could revolutionize gene therapy, paving the way for treating genetic disorders with unprecedented precision and safety.
4. Breakthrough Smart Contact Lens Measures Eye Pressure in All Temperatures
.jpg)
Researchers have developed a prototype smart contact lens capable of accurately measuring eye pressure under varying temperatures. This innovative lens, detailed in a study published in ACS Applied Materials & Interfaces, overcomes a critical challenge in current pressure-sensing technologies.
Traditional smart contact lenses, designed to detect subtle changes in intraocular pressure, often transmit signals to receptor glasses. However, their accuracy can be affected by temperature shifts, such as stepping into cold weather or warm environments. To address this issue, Dengbao Xiao and his research team developed a contact lens prototype that:
• Maintains accuracy across a wide temperature range.
• Wirelessly transmits real-time data about intraocular pressure.
The researchers suggest that their dual-circuit smart lens design has the potential to enable precise early detection and monitoring of glaucoma, even under varying temperature conditions. This breakthrough could pave the way for more reliable, non-invasive glaucoma management, benefiting patients globally.
5. Robot Radiotherapy Could Improve Treatment for Wet AMD
.jpg)
Researchers from King’s College London, in collaboration with doctors at King’s College Hospital NHS Foundation Trust, have introduced an innovative robotic system for treating wet neovascular age-related macular degeneration (AMD). This groundbreaking approach delivers a one-time, minimally invasive dose of targeted radiation, followed by standard injections, significantly reducing the number of treatments required.
The trial revealed that this cutting-edge method could reduce the global need for injections by approximately 1.8 million annually, offering a transformative solution for wet AMD management.
Key Features of the Treatment:
• Precision Robotics: The system delivers three beams of focused radiation directly to the affected area of the eye.
• Reduced Treatment Burden: Patients needed fewer injections compared to standard care.
• Cost Savings: This approach could result in substantial savings for healthcare systems, including the NHS.
Conducted in collaboration with the University of Bristol and Queen's University Belfast, the study represents a major advancement in AMD treatment, providing hope for better patient outcomes and alleviating healthcare challenges.
6. Researchers Develop Novel Phototherapy Technique to Treat Ocular Melanoma
.jpg)
Scientists from the Optics and Photonics Research Center (CePOF) in Brazil, in collaboration with researchers from the University of Toronto and the Princess Margaret Cancer Center in Canada, have made a significant advancement in cancer treatment. Their study, published in Proceedings of the National Academy of Sciences, demonstrates the successful application of a novel phototherapy technique to eliminate ocular melanoma in mice.
Photodynamic therapy (PDT), which uses light to activate drugs, has been effective in treating various cancers. However, its application to melanoma has been limited due to the pigment melanin absorbing much of the light, reducing its efficacy.
The research team addressed this challenge by utilizing a femtosecond pulsed laser:
• Ultrafast, high-energy light bursts allowed precise targeting of melanoma cells.
• Minimized damage to surrounding healthy tissue ensured a safer treatment approach.
While the results are promising, the researchers emphasize the need for further investigation, including studies with humanized mice and subsequent clinical trials, before the approach can be applied to patients. Efforts are also underway to develop specialized tools, such as an adapted ophthalmoscope for treating ocular tumors, to support future clinical applications.
7. Stem Cell Breakthrough Restores Human Vision in Regenerative Medicine Milestone
.jpg)
Researchers at Osaka University in Japan have successfully completed the first human trial using induced pluripotent stem-cell (iPSC)-derived corneal epithelium to treat limbal stem cell deficiency (LSCD). This pioneering approach marks a significant step forward in vision restoration for patients with severe ocular conditions.
The study, titled "Induced pluripotent stem-cell-derived corneal epithelium for transplant surgery: a single-arm, open-label, first-in-human interventional study in Japan," was published in The Lancet. Researchers transplanted iPSC-derived corneal epithelial sheets (iCEPS) to address LSCD, offering a promising new avenue for regenerative eye care.
The iCEPS were developed using a specialized technique that mimics natural eye development, resulting in functional corneal cells with preserved structural integrity and reduced immunogenicity. This innovative method could eliminate the need for HLA matching and minimize the extensive immunosuppression typically required with traditional grafts.
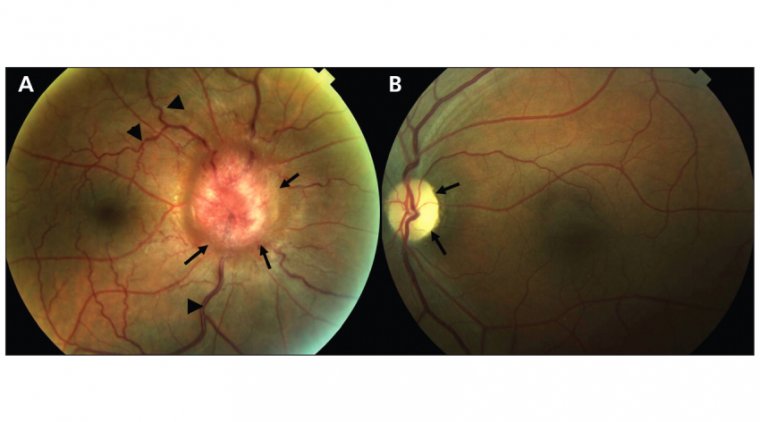
8. Nerve Regrowth Breakthrough Could Offer Hope for Blindness Treatment
.jpg)
Researchers at the University of Connecticut have made a breakthrough discovery in regenerating injured optic nerves, a common cause of blindness linked to trauma and glaucoma. Published in Experimental Neurology, the study demonstrates how an injectable peptide can stimulate dense regrowth of optic nerve fibers in mice, extending to the optic chiasm, a critical brain region for vision processing. This innovative approach offers hope for treating vision loss caused by blunt trauma and glaucoma, the second leading cause of blindness worldwide, according to the CDC.
The team, led by Dr. Ephraim Trakhtenberg of the UConn School of Medicine, identified peptides derived from fibronectin, a protein known to encourage nerve regeneration. The small peptides can be injected directly into the eye, bypassing the need for inflammatory stimuli that initially inspired the research. In trials, the peptide treatment significantly improved nerve cell survival and regrowth through the injury site, with promising results when combined with gene therapy. Longer trials are planned to evaluate whether these regenerated fibers can reach vision-processing brain regions and restore visual function.
This research represents a significant step forward in addressing optic nerve damage caused by injuries and diseases like glaucoma. With further investigation and eventual human trials, fibronectin-derived peptides could potentially become a viable treatment for millions of patients worldwide, offering hope for restoring vision where current options remain limited.
9. Novel Treatment Dramatically Slows Down Progression of AMD, RP
.jpg)
A breakthrough study has introduced a promising advancement in the treatment of age-related macular degeneration (AMD) and retinitis pigmentosa, two leading causes of vision loss. Researchers have developed a hydrogel-based drug delivery system that integrates anti-inflammatory agents targeting the inflammatory factor EZH2, a key contributor to retinal degeneration. By addressing the inflammation responsible for photoreceptor cell damage, this innovative approach offers a more efficient alternative to traditional intraocular injections, which require frequent re-administration due to limited drug retention.
The hydrogel, formulated with hyaluronic acid, mimics the mechanical and optical properties of the eye’s vitreous humor, ensuring gradual degradation tailored to individual patient needs. When tested in mice with retinal degeneration, the hydrogel demonstrated a 6.1% reduction in retinal inflammatory factors and a fourfold increase in photoreceptor cell protection, significantly slowing disease progression. Its inflammation-responsive design facilitates sustained drug release, reducing the need for repeated injections and offering a more patient-friendly solution.
This groundbreaking technology, spearheaded by Dr. Maesoon Im and collaborators at Kyung Hee University and Seoul National University, could revolutionize the management of retinal diseases. Beyond enhancing quality of life by reducing hospital visits, the system holds potential for broader applications in other retinal conditions. Future plans include digitizing treatment parameters for commercialization and further assessing the long-term stability of this innovative drug delivery platform.
10. Trinity College Researchers Develop Promising Gene Therapy for Glaucoma and AMD
.jpg)
Researchers at Trinity College Dublin have developed a promising gene therapy to treat glaucoma and dry age-related macular degeneration (AMD). Using an enhanced gene, eNdi1, delivered via an approved viral vector, the therapy aims to improve mitochondrial function in retinal cells. In animal models, it effectively protected retinal ganglion cells (RGCs) and improved their function, while in human cells, it increased oxygen consumption and ATP production, addressing key mechanisms underlying these conditions.
Glaucoma, a complex optic neuropathy affecting approximately 80 million people worldwide, has limited treatment success with current options like eye drops, surgery, or laser therapy. Highlighting the disease’s complexity, Dr. Sophia Millington-Ward emphasized the urgent need for targeted therapies. The new gene therapy offers a potential breakthrough by enhancing mitochondrial activity, reducing harmful reactive oxygen species, and safeguarding RGCs. Professor Jane Farrar underscored the importance of broad therapies capable of treating large patient populations to offset high development costs.
To advance this innovation, the research team has founded Vzarii Therapeutics, focusing on clinical translation for both glaucoma and dry AMD. With support from organizations including Science Foundation Ireland and Health Research Board Ireland, their efforts aim to expedite human trials, bringing this groundbreaking therapy closer to patients and addressing a critical gap in ocular treatment options.
A Vision of the Future
With each groundbreaking discovery, the future of ophthalmology shines brighter. From cutting-edge therapies to advanced insights into ocular biology, these innovations are paving the way for more effective treatments and an improved quality of life for those living with eye diseases. The relentless collaboration of researchers and scientists worldwide continues to push the boundaries of possibility in eye care, bringing hope to millions across the globe.
(1).jpg)