Breakthrough Study Reveals Promising Treatment for Corneal Endothelial Disease
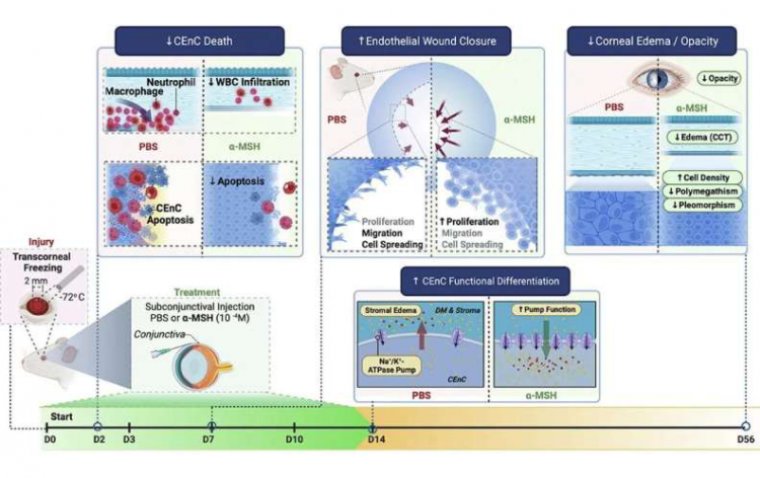
In a groundbreaking study published in The American Journal of Pathology, researchers at Mass Eye and Ear of the Harvard Medical School Department of Ophthalmology have unveiled a novel therapeutic approach using the neuropeptide α-melanocyte–stimulating hormone (α-MSH) to promote corneal healing and restore normal eye function in degenerating and diseased corneas.
Corneal endothelial disease, a condition leading to corneal swelling and potential blindness, poses a significant medical challenge due to the lack of available therapies. Currently, corneal transplantation stands as the most common type of transplant performed. The urgent need for safe and effective medical strategies to prevent and reverse persistent corneal edema has driven researchers to explore innovative treatments for corneal endothelial cell (CenC) loss following injury.
The study focused on the local administration of α-MSH and its impact on persistent corneal edema and endothelial regeneration in a well-established model of injury-induced endothelial decompensation. The results underscore the remarkable therapeutic potential of activating the melanocortin pathway using α-MSH, paving the way for new avenues in ocular therapy.
Lead investigator Dr. Reza Dana, Director of the Cornea and Refractive Surgery Service at Mass Eye and Ear and Claes H. Dohlman Professor of Ophthalmology at Harvard Medical School, emphasizes the transformative effects of α-MSH: "Our data, demonstrating the potent therapeutic effects of α-MSH through melanocortin receptor agonism, provide compelling evidence for the therapeutic potential of this pathway for a wide array of ocular disorders."
α-MSH, an evolutionarily conserved neuropeptide derived from pro-opiomelanocortin, exhibits diverse functions through various melanocortin receptors in different tissues. The study's findings highlight the multifaceted benefits of α-MSH administration, including the prevention of corneal endothelial cell death, restoration of normal endothelial function, normalization of corneal thickness post-severe injury, and promotion of corneal cell regeneration.
Currently, interventions for preventing corneal edema following ocular injury are limited to topical hypertonic saline and topical anti-inflammatory drugs. However, these approaches have demonstrated limited efficacy and do not address CEnC decompensation. The study's revelations open up promising prospects for addressing the unmet needs of patients with corneal endothelial disease and offer hope for more effective and targeted treatments in the future.
Reference
Hamid Alemi et al, The Neuropeptide α-Melanocyte–Stimulating Hormone Prevents Persistent Corneal Edema following Injury, The American Journal of Pathology (2023). DOI: 10.1016/j.ajpath.2023.09.007
(1).jpg)