Corneal Edema: Causes, Symptoms, and Treatment Strategies
What Is Corneal Edema?
Corneal edema refers to the swelling of the cornea, the transparent, dome-shaped layer at the front of the eye. This swelling typically results from an abnormal accumulation of fluid within the corneal layers, disrupting its usual function. The condition can be a sign of other underlying eye problems and may significantly impair vision if not treated appropriately.
The cornea plays an essential role in vision by focusing light onto the retina, which then transmits visual signals to the brain. A healthy cornea is critical for clear vision, and its natural water content is tightly regulated. However, various factors can interfere with this balance, leading to fluid buildup and, consequently, corneal edema.
Causes of Corneal Edema
Corneal edema is a multifactorial condition, and several primary and secondary factors can contribute to its development.
Primary Causes
1. Endothelial Cell Dysfunction: The endothelial cells lining the inner surface of the cornea help to pump out excess fluid. Dysfunction or a decrease in the number of these cells can lead to fluid retention and corneal edema.
2. Trauma: Physical injuries to the eye, like blunt force trauma or chemical burns, can disrupt the natural fluid balance in the cornea, leading to swelling.
3. Surgical Complications: Eye surgeries like cataract extraction can sometimes result in corneal edema due to either mechanical disruption or endothelial cell loss.
Secondary Causes
1. Glaucoma: Elevated intraocular pressure in conditions like glaucoma can damage the corneal endothelium, making it less efficient at regulating fluid balance.
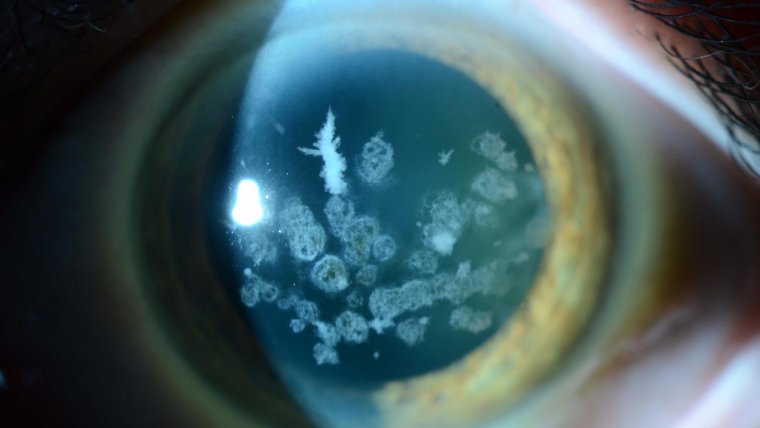
2. Fuchs' Dystrophy: This genetic disorder affects the corneal endothelium and can gradually lead to corneal edema over time.
3. Inflammatory Disorders: Conditions like uveitis can cause inflammation that affects various eye structures, including the cornea, potentially leading to edema.
Corneal Edema After Cataract Surgery
Corneal edema following cataract surgery is a recognized complication, though it's generally temporary and resolves as the eye heals. During cataract surgery, the eye's natural lens is removed and replaced with an artificial intraocular lens. While highly effective, this surgery involves manipulating the eye structures, which can sometimes cause trauma to the corneal endothelial cells.
Key Factors
1. Surgical Technique: The skill and technique employed by the surgeon can impact the likelihood of developing corneal edema. Advanced techniques are generally less invasive and minimize trauma to the corneal endothelium.
2. Instrumentation: The type of instruments and surgical devices used can also influence endothelial cell loss. High-quality, precise instruments tend to reduce complications.
3. Surgical Time: Prolonged surgical procedures may increase the risk of corneal edema as they can cause greater stress to the endothelial cells.
Management
1. Observation: Mild cases usually resolve on their own as the eye heals. Close monitoring is required to ensure that the condition improves.
2. Topical Medication: Ophthalmic solutions like hypertonic saline can help draw out excess fluid from the cornea.
3. Follow-Up: Regular postoperative check-ups are crucial for monitoring the resolution of the edema and preventing any long-term complications.
Symptoms of Corneal Edema
Corneal edema manifests in a variety of ways that can disrupt normal vision and cause significant discomfort. Recognizing these symptoms is crucial for timely diagnosis and intervention.
● Blurred Vision: One of the most common signs of corneal edema is a blurred or hazy vision. The accumulation of fluid in the corneal layers scatters light entering the eye, leading to diminished visual acuity.
● Eye Discomfort: Individuals may experience a sense of fullness, pressure, or pain in the eye. The sensation can range from a minor irritation to significant discomfort that impacts daily activities.
● Halos Around Lights: Another hallmark symptom is the perception of halos or auras around light sources. This phenomenon can be especially noticeable in low-light or nighttime conditions.
● Photophobia: Sensitivity to light is often reported and can exacerbate other symptoms like pain and blurred vision.
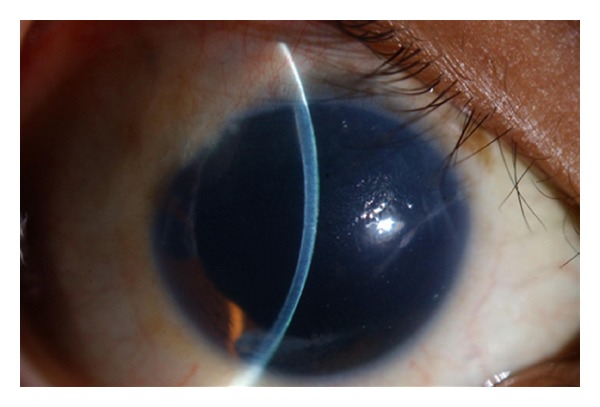
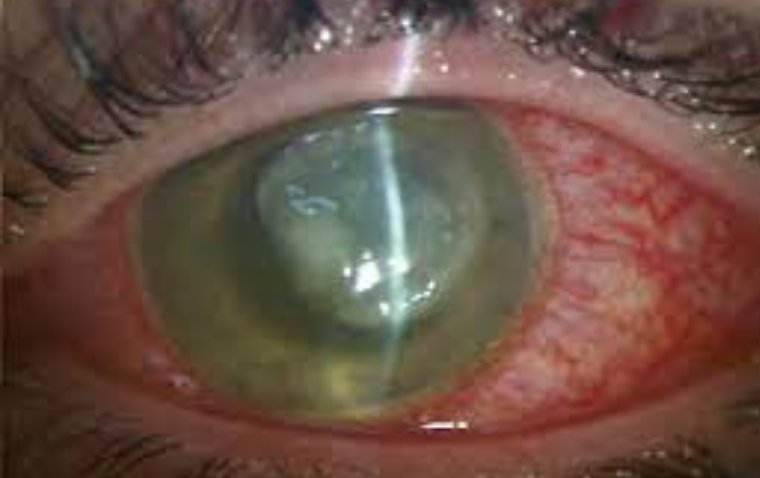
Clinical picture on presentation showing corneal edema Credit: Research Gate
Severity-Based Variations
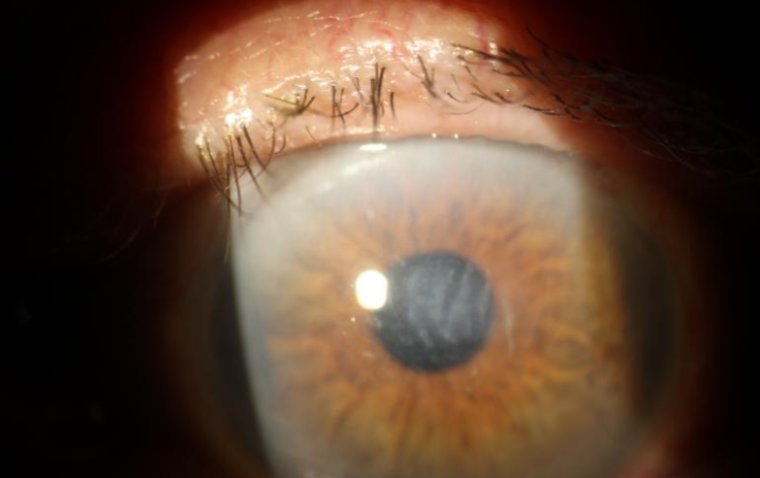
● Mild Cases: In mild instances of corneal edema, symptoms may only occur in certain conditions like dim lighting or upon waking up. Vision often improves throughout the day as the cornea adjusts.
● Moderate to Severe Cases: In more severe cases, the symptoms can be constant and significantly impair visual function, requiring immediate medical intervention to prevent further complications.
How to Diagnose Corneal Edema
Proper diagnosis of corneal edema is crucial for effective treatment and management. Various diagnostic techniques are employed to confirm the presence and extent of edema, as well as to identify the underlying cause.
Diagnostic Methods
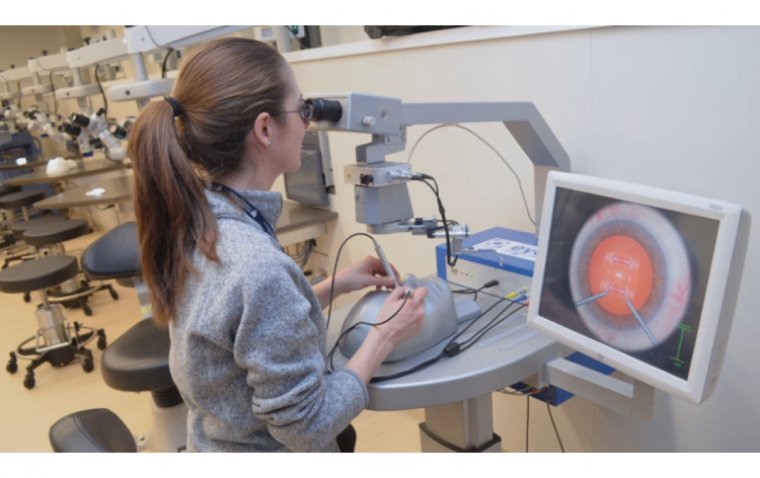
1. Slit-Lamp Examination: This is often the first step in diagnosing corneal edema. A slit-lamp microscope is used to illuminate and magnify the cornea, allowing the eye care provider to assess its condition and look for signs of fluid accumulation.
2. Corneal Pachymetry: This test measures the thickness of the cornea using ultrasound technology. An increased corneal thickness often indicates edema.
3. Endothelial Cell Count: A specular microscope is used to count the number of endothelial cells in the cornea. A low cell count suggests endothelial dysfunction, which could be the root cause of the edema.
4. Additional Tests: In some cases, additional tests like corneal tomography may be recommended for a more detailed assessment.
How Is Corneal Edema Treated?
Treatment of corneal edema varies depending on the underlying cause and severity of the condition. Here is an overview of both conservative and advanced treatment options:
Conservative Treatments
Eye Drops: Ophthalmic solutions like artificial tears or lubricants can provide relief from the symptoms of corneal edema, although they don't directly treat the cause.
Hypertonic Solutions: These are specialized eye drops with a higher salt concentration. They draw excess fluid out of the cornea, helping to reduce swelling.
Lifestyle Adjustments: In some cases, simple lifestyle changes like reducing screen time or avoiding smoky or windy environments can alleviate symptoms.
Advanced Treatments
1. Corneal Transplantation: For severe cases of corneal edema that don't respond to conservative treatments, a corneal transplant may be recommended. There are different types of corneal transplantation:
● Penetrating Keratoplasty (PK): This involves replacing the entire cornea with a healthy donor cornea. PK is a more invasive option and is generally reserved for the most severe cases.
● Descemet's Stripping Endothelial Keratoplasty (DSEK): In this procedure, only the innermost layer of the cornea is replaced. DSEK is less invasive than PK and offers a quicker recovery time.
2. Bandage Contact Lenses: In some instances, a special type of contact lens may be used to promote healing and provide symptom relief.
3. Surgical Drainage: In rare cases, small incisions may be made in the cornea to allow for fluid drainage.
4. Pharmacologic Agents: Medications like corticosteroids may be prescribed to manage underlying inflammatory conditions that contribute to corneal edema.
Preventive Measures
Preventing corneal edema primarily involves proactive eye care, as well as the management of any underlying conditions that may put you at risk. Below are some tips to help you minimize the chances of developing corneal edema:
Protecting Your Eyes from Trauma
Safety Gear: Always wear appropriate eye protection, like safety goggles or sunglasses, when engaged in activities that pose a risk of eye injury, such as sports, DIY projects, or exposure to harmful chemicals.
Eye Hygiene: Practice good eye hygiene, including frequent hand washing and avoiding touching or rubbing your eyes with unclean hands.
Managing Underlying Conditions
Control Glaucoma: If you have glaucoma, it's crucial to manage it effectively to minimize the risk of corneal edema. Follow your ophthalmologist's advice and medication regimen meticulously.
Fuchs' Dystrophy: For those with Fuchs' dystrophy or other corneal diseases, regular check-ups can help monitor for signs of corneal edema before it becomes problematic.
Systemic Diseases: Conditions like diabetes can have an impact on eye health. Properly managing these conditions can reduce the risk of developing corneal edema.
Emerging Research and Innovations
In recent years, there has been significant progress in the understanding and management of corneal edema, leading to several exciting developments:
New Treatment Modalities
● Descemet Membrane Endothelial Keratoplasty (DMEK): While not entirely new, the technique's refinements have made it more successful in treating corneal edema with faster recovery periods and better visual outcomes compared to traditional methods.
● Topical Therapies: Advances in pharmacology have led to more effective topical medications. Eye drops containing novel agents are under investigation, aiming to reduce corneal edema more efficiently.
● Gene Therapy: Research is underway to explore the potential of gene therapy in treating corneal edema caused by genetic conditions like Fuchs' dystrophy.
● Endothelial Cell Transplant: Novel methods of culturing corneal endothelial cells and transplanting them into the affected eye are being researched. This could eventually offer a less invasive alternative to full corneal transplantation.
Drug Therapies
● Anti-inflammatory Drugs: New formulations of anti-inflammatory drugs are being explored for their effectiveness in reducing corneal edema post-surgery or injury.
● Molecular Target Therapy: By understanding the molecular pathways involved in fluid regulation within the cornea, researchers are developing drugs that could target specific mechanisms, thereby offering more effective treatments.
Diagnostic Advancements
● Advanced Imaging Techniques: Tools like optical coherence tomography (OCT) have become more refined, providing clinicians with better ways to diagnose and monitor the condition of the cornea.
● Artificial Intelligence: Machine learning algorithms are being developed to analyze diagnostic images more quickly and accurately, aiding in the early detection and treatment of corneal edema.
Summary
Corneal Edema is a condition that involves the buildup of fluid in the cornea, affecting vision and overall eye health. Its causes can range from endothelial cell dysfunction and trauma to secondary issues like glaucoma and Fuchs' dystrophy. Symptoms include blurred vision, eye discomfort, and seeing halos around lights.
Accurate diagnosis, often involving slit-lamp examination, corneal pachymetry, and endothelial cell counts, is crucial for effective treatment. While conservative treatments like eye drops and lifestyle adjustments often help manage mild cases, more severe instances may require surgical interventions such as corneal transplantation.
Preventive measures include protecting the eyes from trauma and adhering to post-operative care guidelines. In terms of future perspectives, the field is witnessing emerging research and innovations in both diagnostic and treatment modalities, providing hope for more effective and less invasive solutions.
(1).jpg)