Understanding Ocular Torticollis: Causes and Symptoms
What Is Ocular Torticollis?
Ocular torticollis, sometimes referred to as ocular "twisted neck," is a condition where an individual adopts an abnormal head or neck position to compensate for an eye misalignment or vision disorder. The purpose of this unusual posture is to maximize visual clarity and minimize symptoms like double vision.
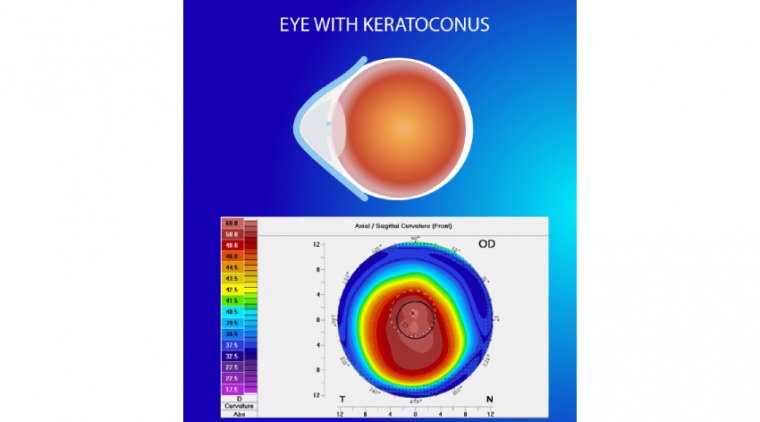
The eye misalignment in question could result from conditions such as strabismus (misaligned eyes), nystagmus (uncontrolled eye movements), or significant refractive errors like astigmatism. The abnormal posture associated with ocular torticollis varies and can involve tilting the head to one side, tucking the chin down, or turning the head in a particular direction.
The continual adaptation to this atypical posture may result in physical discomfort, social unease, and, in severe cases, musculoskeletal changes. For this reason, understanding and addressing ocular torticollis is crucial in promoting optimal eye health and overall quality of life.
Causes and Risk Factors of Ocular Torticollis
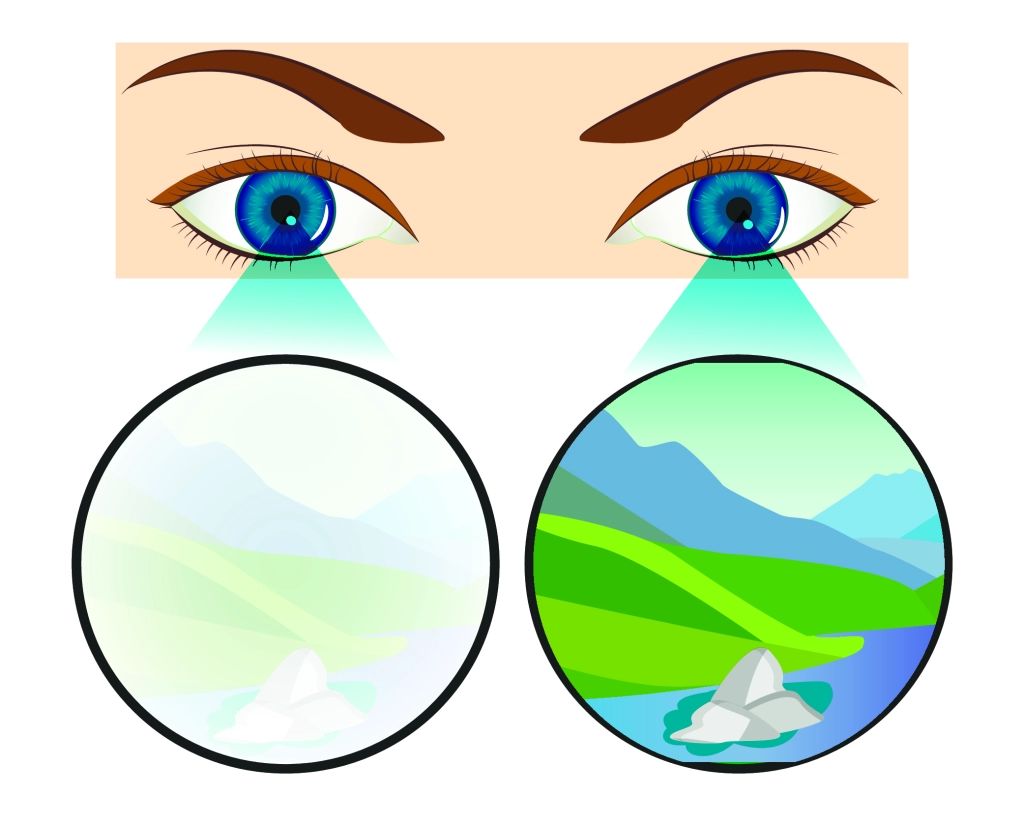
Ocular torticollis is typically a response to an underlying eye or vision problem. One of the most common causes is strabismus, a condition characterized by eye misalignment. In strabismus, the eyes do not look in the same direction at the same time, leading to double vision or blurred vision. To avoid these visual disturbances, an individual may tilt or turn their head to align their eyes better.
Another possible cause is an imbalance in the eye muscles, whether due to a congenital issue or as a result of ocular trauma. In such cases, the abnormal head posture helps align the eyes to achieve single and clear vision. Other eye conditions, like nystagmus or high refractive errors, may also lead to ocular torticollis.
Beyond ocular conditions, neurological disorders such as cerebral palsy, stroke, or tumors can also result in ocular torticollis. These conditions can impact the nerves controlling eye movements, leading to eye misalignment or other vision problems.
Risk factors for ocular torticollis may include a family history of eye misalignment or neurological disorders, premature birth, history of eye injuries, or certain systemic diseases. Understanding the potential causes and risk factors can help in early detection and appropriate management of ocular torticollis.
Symptoms and Diagnosis of Ocular Torticollis
The most recognizable symptom of ocular torticollis is an abnormal head posture, which can manifest as tilting, turning, or thrusting of the head. The specific posture often depends on the underlying cause. For instance, a person may tilt their head to the side to compensate for vertical misalignment of the eyes or turn their head to minimize the impact of nystagmus.
Other symptoms may include eye strain, blurred vision, or double vision. In children, parents or caregivers may notice a persistent head tilt or turn, and in some cases, developmental delays or learning difficulties due to the vision impairment.
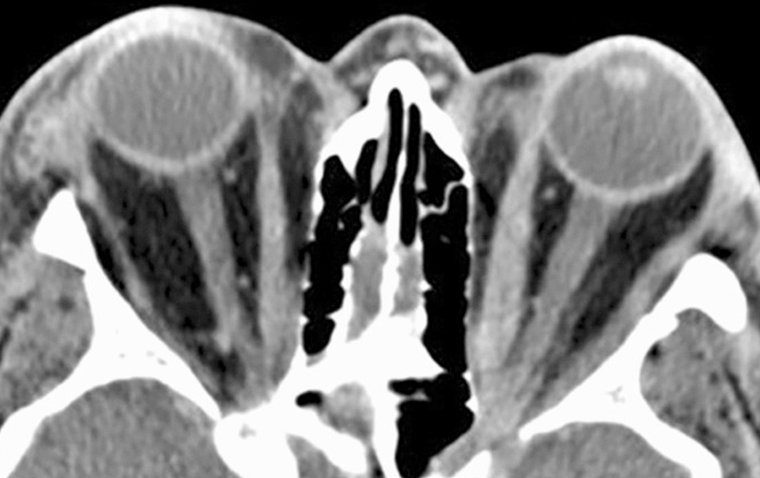
Diagnosing ocular torticollis involves a comprehensive eye examination. An ophthalmologist or optometrist will assess visual acuity, eye alignment and movement, and the overall health of the eyes. Specialized tests like a cover test (to detect strabismus) or ocular motility test (to assess eye movements) may be employed.
In some cases, additional diagnostic tests such as imaging studies or neurological evaluations may be required to rule out or identify any underlying neurological conditions. A thorough diagnosis is crucial as it not only confirms ocular torticollis but also helps pinpoint the underlying cause, paving the way for targeted and effective treatment.
How to Treat Ocular Torticollis
The treatment for ocular torticollis primarily aims to address the underlying cause. The choice of treatment depends on the specific cause, the severity of symptoms, and the individual's overall health.
Corrective lenses or contact lenses may be prescribed to correct refractive errors, while eye muscle exercises or vision therapy can help manage certain types of strabismus and improve eye coordination.
Prism glasses are another treatment option. Prisms can help realign the images seen by each eye, allowing the eyes to work together more effectively and reducing the need for head tilting or turning.
In more severe cases, or when conservative treatments are not effective, surgery may be considered. Surgical procedures can adjust the length or position of eye muscles to improve alignment. Surgery can be very effective but, like any invasive procedure, comes with potential risks, including infection, bleeding, or overcorrection.
Early intervention is crucial for successful treatment and to prevent complications, such as chronic neck pain or musculoskeletal changes. An individualized treatment plan, tailored to the specific needs of the patient, often offers the best outcomes. Regular follow-ups and adjustments to the treatment plan are usually necessary to ensure continued success and to address any potential issues promptly.
It's important for patients and caregivers to discuss with their eye care professional the benefits, risks, and success rates associated with each treatment modality to make an informed decision.
- Rehabilitation and Therapy
Vision therapy and rehabilitation programs play a crucial role in managing ocular torticollis. These tailored programs include specific exercises designed to improve eye coordination, enhance visual skills, and ultimately, reduce the need for abnormal head postures.
These exercises often involve activities that challenge the eye muscles, encouraging them to work together more effectively. For example, pencil pushups, where a pencil is moved back and forth in front of the eyes, can help strengthen the eye muscles and improve their coordination.
In some cases, computer-assisted vision therapy may be used, using software to provide engaging and interactive activities that work on improving eye alignment, depth perception, and visual tracking.
The use of prisms and filters, along with specific eye movement tasks, can also be part of a vision therapy program. These techniques aim to reduce double vision and improve the ability of the eyes to work together, reducing the need for compensatory head postures.
In addition to vision therapy, physical therapy can also be beneficial, particularly in cases where prolonged abnormal head posture has led to neck stiffness or musculoskeletal changes. Physical therapy can help restore normal neck motion and alleviate any associated discomfort.
- Lifestyle Management and Support
Managing ocular torticollis in daily life often involves a combination of medical treatment and practical lifestyle adjustments. Here are some tips that may help:
● Ergonomic Adjustments: Whether it's at work, school, or home, ensure your environment is set up to minimize strain on your eyes and neck. This could involve adjusting the height of your computer monitor, ensuring adequate lighting, or using large-print or high-contrast materials to reduce eye strain.
● Head Positioning: It's important to be mindful of your head position throughout the day. Try to maintain a neutral head position as much as possible, and avoid positions that cause neck strain or exacerbate your symptoms.
● Use of Supportive Devices: Depending on the cause of your ocular torticollis, certain supportive devices can be beneficial. For example, prism glasses can help align your eyes and reduce the need for head tilting or turning. Similarly, using magnifying devices can help if you have difficulty reading or doing close work.
● Regular Breaks: Taking frequent breaks from tasks that require intense focus can help reduce eye strain and discomfort. During these breaks, simple neck and shoulder stretches can also help alleviate any tension buildup.
● Seek Support: Living with ocular torticollis can be challenging, but you don't have to do it alone. Support groups, whether in-person or online, can provide a space to share experiences, tips, and encouragement.
Summary
Ocular torticollis is a condition characterized by abnormal head or neck posture due to eye misalignment or visual disturbances. The root cause can vary, including strabismus, eye muscle imbalance, or neurological disorders. Recognizing symptoms such as unusual head tilting or turning is essential for early diagnosis.
Treatment options for ocular torticollis are diverse, from corrective lenses and prism glasses to surgical interventions, depending on the underlying cause. Rehabilitation and therapy, such as vision therapy exercises, can significantly improve eye coordination and reduce abnormal head posture.
Managing this condition in daily life can be enhanced by practical steps such as ergonomic adjustments, regular breaks, and supportive devices. However, it's crucial to remember that these strategies should be part of a comprehensive treatment plan developed with a healthcare provider.
Overall, while ocular torticollis can impact individuals' quality of life, a combination of appropriate medical treatment, lifestyle modifications, and support can lead to improved visual health and well-being.
(1).jpg)