The Role of IOL Exchange in Optimizing Visual Clarity
What is IOL Exchange?
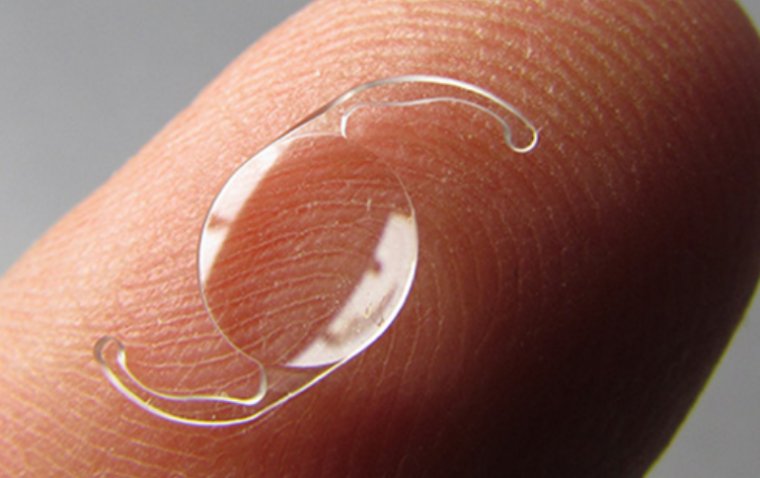
Intraocular lens (IOL) exchange is a surgical procedure that involves the removal of a previously implanted IOL and its replacement with a new lens. This procedure is predominantly undertaken to optimize visual clarity and correct issues stemming from the initial IOL implantation. The purpose of IOL exchange can vary, encompassing a range of corrective measures for complications such as incorrect lens power, lens decentration or dislocation, and IOL opacification, each of which can significantly impair visual acuity and quality of life.
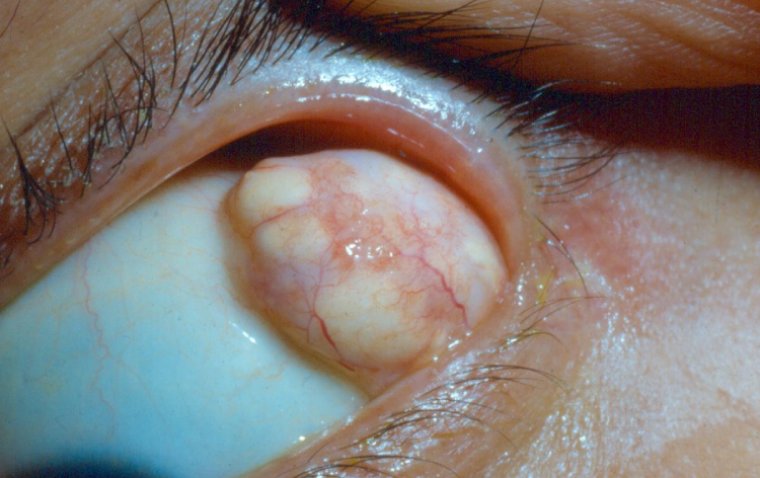
The decision to proceed with an IOL exchange takes into account several critical factors, including the potential for improved vision, the risks associated with reoperation, and the overall health of the patient’s eye. Incorrect IOL power can result from miscalculations during the pre-operative assessment or changes in the eye post-surgery. Decentration or dislocation of the lens may be due to surgical errors, trauma, or weaknesses in the capsular bag or zonules that support the lens. Opacification of the lens, on the other hand, can occur over time due to biochemical changes within the eye, affecting the clarity of the IOL material.
Indications for IOL Exchange
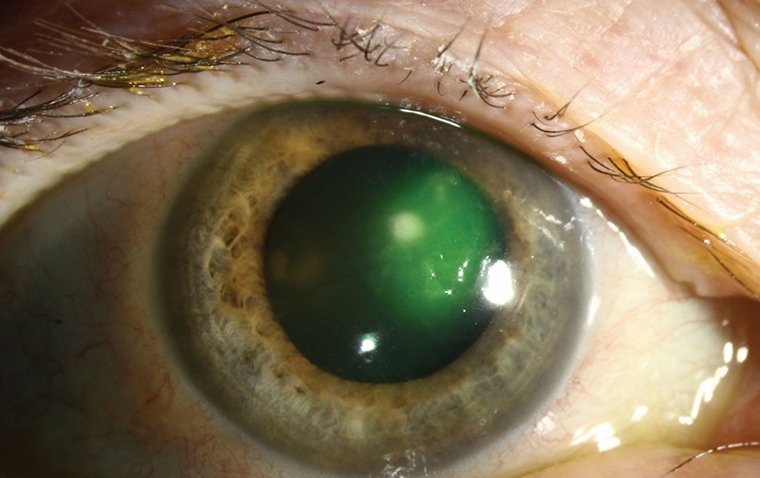
IOL exchange is warranted in various scenarios, each presenting unique challenges and considerations. Indications for this procedure include refractive errors due to incorrect IOL power, which can lead to dissatisfaction with visual outcomes; IOL decentration or dislocation, which can cause significant visual disturbances such as double vision or halos; and IOL opacification, which results in a progressive decline in visual clarity.
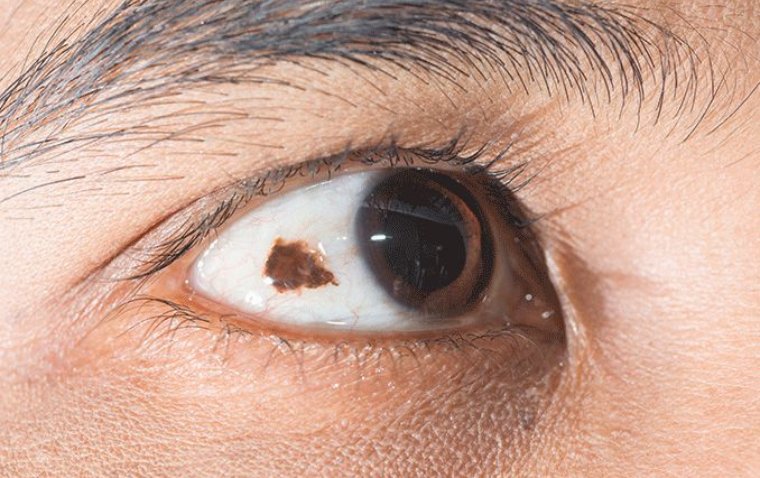
Patient factors play a pivotal role in determining the appropriateness of IOL exchange. These factors include the patient’s overall ocular health, the presence of comorbid conditions such as diabetic retinopathy or macular degeneration, and the potential for visual improvement. The patient’s ability to undergo another surgical procedure, their lifestyle needs, and their specific visual requirements are also critical considerations. A thorough evaluation ensures that the benefits of the exchange outweigh the risks and that the patient’s expectations are realistically aligned with the potential outcomes.
Pre-operative Evaluation
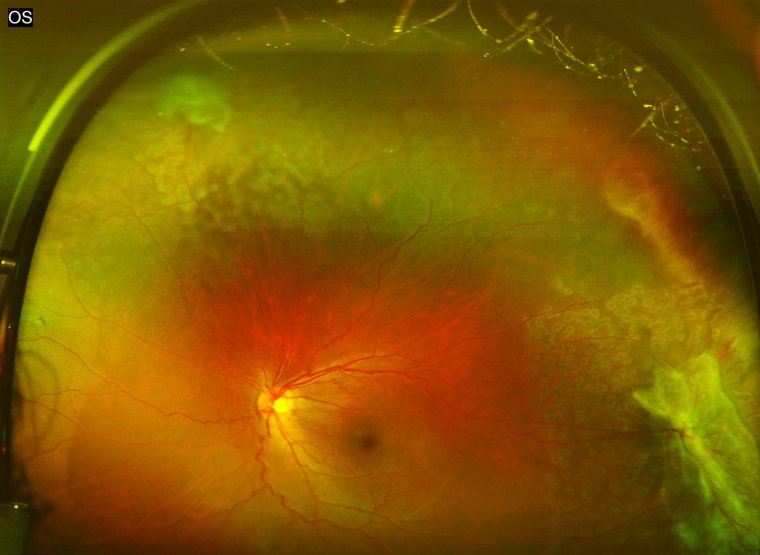
A comprehensive pre-operative evaluation is crucial to the success of an IOL exchange procedure. This evaluation entails a thorough assessment of the patient’s ocular health, focusing on the anterior and posterior segments of the eye to identify any conditions that could affect the surgery’s outcome.
Diagnostic tests play a fundamental role in this phase, with biometry being essential for determining the correct power of the new IOL. Keratometry measures the curvature of the cornea, essential for selecting the appropriate lens and anticipating post-operative refractive status. Additionally, ultrasound imaging, including B-scan or ultrasound biomicroscopy (UBM), may be required to assess the position and stability of the existing IOL and the integrity of the capsular bag.
Surgical Techniques for IOL Exchange
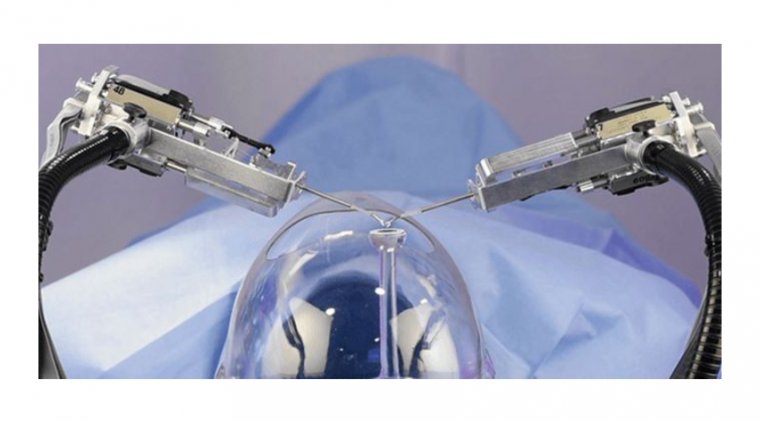
The surgical approach to IOL exchange can vary based on the type of initial implant, the reason for exchange, and the patient's specific anatomical considerations. The procedure generally falls into two main approaches: anterior and posterior. The anterior approach involves accessing the IOL through an incision made in the cornea, typically used when the IOL is situated in the sulcus or has dislocated anteriorly. This method requires precise surgical skill to avoid damage to the corneal endothelium and surrounding ocular structures.
The posterior approach, on the other hand, is preferred if the IOL is encapsulated within the capsular bag and there's a need for posterior segment examination or intervention. This technique may involve a pars plana vitrectomy to manage vitreous prolapse or to stabilize the eye for IOL placement.
A step-by-step guide to the exchange procedure involves careful planning and execution. Initially, the surgeon assesses the stability and position of the existing IOL, followed by making a decision on the incision site and technique for lens removal. Specialized tools and equipment, such as viscoelastics, forceps, and intraocular scissors, are essential for safely extracting the old IOL and implanting the new one, minimizing the risk of intraoperative complications.
Risks and Complications
1. Minor Complications
● Corneal edema (swelling of the cornea)
● Minor bleeding
● Post-operative inflammation
2. Serious Complications
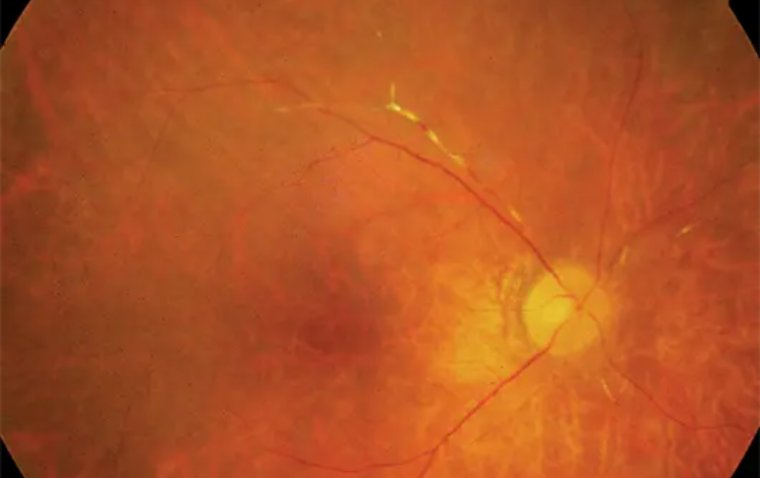
● Retinal detachment
● Infection (endophthalmitis)
● IOL dislocation or decentration
● Cystoid macular edema
● Anterior capsule contraction syndrome
● Persistent ocular pain
Mitigation Strategies
1. Employ meticulous surgical technique to minimize tissue trauma.
2. Conduct thorough pre-operative assessments to identify potential risk factors.
3. Select patients carefully, considering their overall health and ocular conditions.
4. Use antibiotics promptly to treat or prevent infections.
5. Manage elevated intraocular pressure with appropriate medication.
6. Perform surgical interventions for severe complications such as retinal detachment or IOL malpositioning.
Benefits and Outcomes
The primary goal of IOL exchange is to enhance visual clarity and patient satisfaction. Successful IOL exchange can lead to significant improvements in visual acuity, reduction in refractive errors, and resolution of symptoms caused by the initial IOL, such as glare or halos. The impact on the patient’s quality of life can be profound, often allowing them to return to their daily activities with improved vision and confidence.
Patient satisfaction post-IOL exchange is closely linked to the alignment of pre-operative expectations with post-operative outcomes. Clear communication about the realistic goals of surgery and potential limitations is essential in achieving this alignment.
Post-operative Care
Effective post-operative care is crucial for ensuring a smooth recovery and optimal outcomes following an IOL exchange. Detailed instructions for post-operative care typically include the use of antibiotic and anti-inflammatory eye drops to prevent infection and reduce inflammation. Regular follow-up visits are scheduled to monitor the healing process, assess the positioning of the new IOL, and identify any early signs of complications.
Educating patients on the importance of adhering to medication schedules, avoiding activities that may put undue pressure on the eye, and recognizing signs of potential complications is a key part of post-operative care. Addressing patient concerns promptly and providing reassurance can help ensure a positive recovery experience.
Emerging Trends and Innovations
The field of IOL exchange is continually evolving, with advancements in surgical techniques, IOL materials, and diagnostic equipment enhancing the safety and efficacy of the procedure. Recent innovations include the development of more biocompatible lens materials that reduce the risk of opacification and the use of advanced imaging technologies for precise IOL positioning.
Future developments may focus on minimally invasive techniques for IOL exchange, the integration of smart lens technology capable of adjusting focus dynamically, and further improvements in IOL designs to cater to a wider range of refractive errors and patient needs.
Summary
IOL exchange plays a critical role in optimizing visual clarity for patients experiencing issues with their initial lens implants. By carefully considering the indications for surgery, employing meticulous surgical techniques, and providing comprehensive post-operative care, ophthalmologists can significantly improve visual outcomes and patient satisfaction. As the field continues to advance, new techniques and technologies promise to enhance the safety and effectiveness of IOL exchange, offering hope for even better results in the future.
Reference:
(1).jpg)