Can Eye Pressure Fluctuate? Understanding Intraocular Pressure Variations
Intraocular pressure (IOP) is a critical measurement in eye health, often associated with eye conditions like glaucoma. This pressure is the force exerted by the aqueous humor, the fluid inside the eye, on the ocular structures. Traditionally, eye pressure has been considered relatively stable, but recent research has shed light on its potential fluctuations. Understanding the factors contributing to IOP variations, their significance, and the implications for eye health can aid in better management and preservation of vision.
Factors Contributing to Eye Pressure Fluctuations
Several factors can lead to fluctuations in intraocular pressure, both in healthy individuals and those with eye conditions. Some of these factors include:
1. Diurnal Variation: A common type of fluctuation, diurnal variations cause IOP levels to be higher in the morning and decrease throughout the day. This pattern is influenced by factors such as body position changes, circadian rhythms, and fluid dynamics within the eye.
2. Physical Activity: Certain physical activities, such as bending over, lifting heavy objects, or vigorous exercise, can briefly elevate IOP. For individuals with glaucoma, such spikes in pressure can be of concern.
3. Eye Rubbing: Vigorous eye rubbing can temporarily increase IOP. Allergic reactions or itchy eyes may prompt individuals to rub their eyes more frequently, potentially contributing to fluctuations.
4. Medication and Eye Drops: Some medications, particularly corticosteroids, can influence eye pressure. Similarly, the use of eye drops, such as those used to dilate the pupils, can temporarily impact IOP.
The Significance of Fluctuating Eye Pressure
While some degree of IOP fluctuation is considered normal, sustained or significant variations may hold implications for eye health, particularly in individuals with pre-existing conditions like glaucoma. For those with glaucoma, consistently high or fluctuating eye pressure can contribute to optic nerve damage, leading to progressive vision loss. Consequently, regular monitoring and assessment of IOP are paramount in glaucoma management, as changes in pressure may necessitate adjustments to the treatment plan.
Importance of Regular Eye Exams
Routine and comprehensive eye examinations are instrumental in evaluating IOP and detecting any fluctuations. Eye care professionals employ tonometry, a non-invasive technique, to accurately measure intraocular pressure. Monitoring IOP over time enables healthcare providers to identify trends and gauge the effectiveness of glaucoma treatments.
Management and Treatment
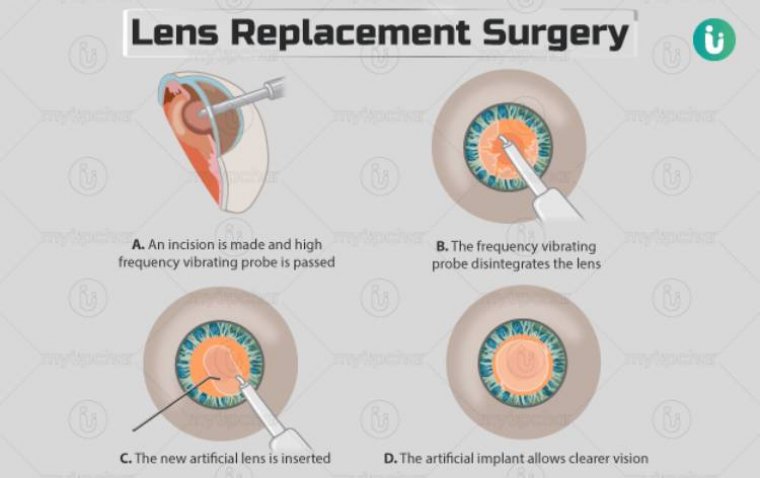
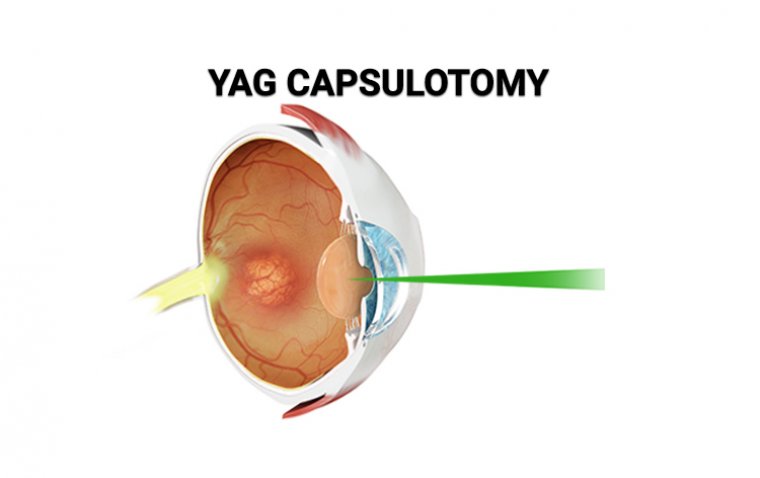
For individuals at risk of glaucoma or other conditions where IOP plays a significant role, maintaining stable eye pressure is of utmost importance. Eye care professionals may recommend various treatment approaches, including medication, eye drops, or surgery, to effectively control IOP and prevent further vision loss. Additionally, lifestyle modifications, such as stress reduction and avoiding activities that elevate eye pressure, can complement medical interventions.
Summary
Eye pressure can indeed fluctuate due to various factors, including diurnal variations, physical activities, and eye rubbing. While some fluctuations are normal, sustained or significant variations may have implications for eye health, particularly in individuals with glaucoma. Regular eye exams and close monitoring of IOP are vital for early detection, effective management, and preservation of vision. Working closely with eye care professionals can help ensure optimal eye health and well-being for individuals at risk of IOP fluctuations.
(1).jpg)