Corneal Ectasia: Causes, Symptoms and Treatment Options
What is Corneal Ectasia?
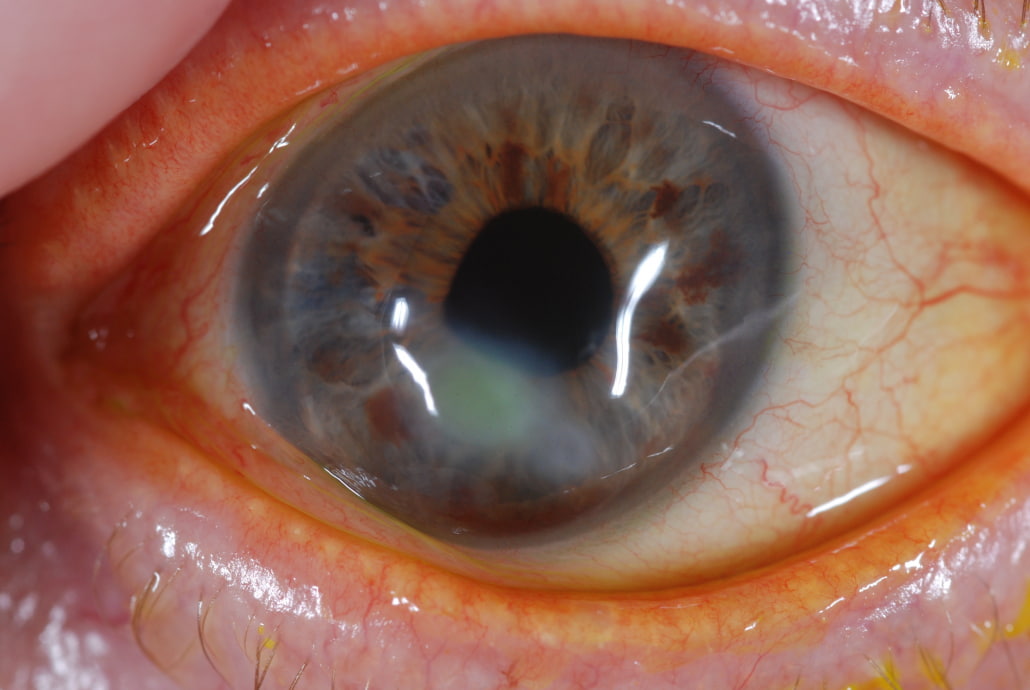
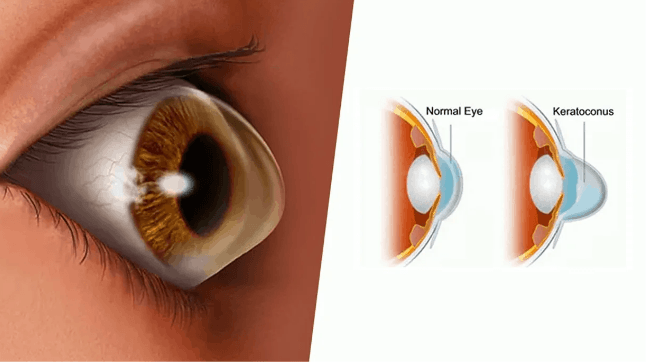
Corneal Ectasia is a progressive eye disorder characterized by the thinning and deformation of the cornea, the clear, dome-shaped surface that covers the front of the eye. This thinning leads to a bulging or protruding corneal shape, significantly impacting the cornea's ability to focus light correctly, which in turn causes visual distortion. The condition is often progressive, meaning it can worsen over time. As the cornea becomes increasingly irregular in shape and thinner, it can lead to various levels of impaired vision, from mild blurring to significant visual impairment.
Types of Corneal Ectasia
1. Keratoconus: This is the most common form of corneal ectasia, where the cornea progressively thins and begins to bulge into a cone-like shape. Keratoconus typically begins during adolescence and can progress for about a decade or more.
2. Keratoglobus: A rare form of ectasia, Keratoglobus involves generalized thinning of the entire cornea, which bulges forward in a more spherical shape. This condition is often present from birth or develops in early childhood.
3. Post-LASIK Ectasia: This occurs as a rare complication of LASIK (Laser-Assisted In Situ Keratomileusis) surgery, where the corneal structure becomes unstable and begins to protrude post-surgery, similar to keratoconus. It underscores the importance of proper patient selection and corneal thickness assessment before refractive surgery.
4. Pellucid Marginal Degeneration (PMD): PMD is characterized by a thinning of the lower half of the cornea. It generally presents later than keratoconus and can lead to irregular astigmatism.
5. Terrien’s Marginal Degeneration: This less common type of ectasia involves thinning of the corneal margin, usually at the upper periphery. Unlike other forms, it typically does not lead to significant bulging, but can cause astigmatism and vision impairment.
Causes of Corneal Ectasia
Corneal Ectasia results from a weakening of the corneal structure, leading to its abnormal protrusion or bulging. Several factors can contribute to this weakening:
● Genetic Factors: Many cases, particularly those of keratoconus, have a genetic component. Individuals with a family history of corneal ectasia are at a higher risk.
● Eye Rubbing: Chronic and vigorous eye rubbing has been linked to the progression of ectasia, likely due to the mechanical stress it places on the cornea.
● LASIK Complications: In rare cases, LASIK surgery can lead to post-LASIK ectasia. This occurs when the corneal tissue removal during the surgery weakens the structural integrity of the cornea. Patients with thinner corneas or preexisting corneal conditions are at a higher risk.
● Hormonal Changes: Hormonal fluctuations, particularly during adolescence, can contribute to the development and progression of corneal ectasia.
● Contact Lens Wear: Improper or long-term contact lens wear, especially hard or poorly fitting lenses, may be associated with the development of ectatic conditions.
Corneal Ectasia Symptoms
The symptoms of Corneal Ectasia primarily revolve around vision distortion due to the irregular shape of the cornea. Key symptoms include:
Blurred Vision: As the cornea becomes more irregular, light rays are not focused properly on the retina, leading to blurred vision.
Astigmatism: Irregular astigmatism, which cannot be corrected fully with glasses, is a common symptom due to the uneven curvature of the cornea.
Increased Sensitivity to Light and Glare: Patients often experience heightened light sensitivity and glare, particularly at night.
Ghost Images: Some individuals may see multiple ghost-like images, especially in low light conditions.
Rapid Changes in Vision: Frequent changes in visual acuity or prescription, particularly during adolescence or early adulthood, can be a sign of progressing ectasia.
Common Signs of Keratoconus: In keratoconus, which is the most common type of corneal ectasia, signs include a visible thinning or coning of the cornea, and in advanced stages, a visible scar may form at the apex of the cone.
Corneal Ectasia vs. Keratoconus
Understanding the distinction between Corneal Ectasia and Keratoconus is crucial, as it helps in accurate diagnosis and appropriate management of each condition.
1. Definition:
● Corneal Ectasia is a broad term that refers to a group of conditions characterized by the progressive thinning and deformation of the cornea, leading to visual distortion. It includes various types such as Keratoconus, Keratoglobus, Post-LASIK ectasia, and others.
● Keratoconus, on the other hand, is a specific type of corneal ectasia. It is a condition where the cornea progressively thins and bulges into a cone-like shape, primarily affecting the central or paracentral area of the cornea.
2. Cause and Progression:
● Corneal Ectasia can be caused by various factors including genetic predisposition, eye rubbing, and as a complication of corneal surgery (like LASIK).
● Keratoconus is often idiopathic but is believed to be linked to genetic factors, oxidative stress, and environmental factors like chronic eye rubbing.
3. Patterns of Thinning:
● Corneal Ectasia in general shows thinning of the corneal tissue, but the pattern can vary depending on the specific type. For instance, in post-LASIK ectasia, the thinning is often noted in the area where the corneal flap was created.
● Keratoconus typically shows a localized, cone-shaped protrusion, often more pronounced in the lower half of the cornea.
4. Associated Conditions:
● Corneal Ectasia can be associated with other eye conditions depending on its cause, such as complications from LASIK or other corneal surgeries.
● Keratoconus is sometimes associated with systemic disorders like Down syndrome, Ehlers-Danlos syndrome, and atopic diseases.
5. Visual Symptoms:
● Both conditions lead to visual impairment due to irregular astigmatism and myopia. However, the severity and progression can vary.
How to Diagnose Corneal Ectasia
Diagnosing Corneal Ectasia involves a series of tests and evaluations:
1. Patient History: Understanding the patient's vision history, family history of eye conditions, and any previous eye surgeries or trauma is essential.
2. Visual Acuity Test: This standard eye test measures the clarity of vision at various distances.
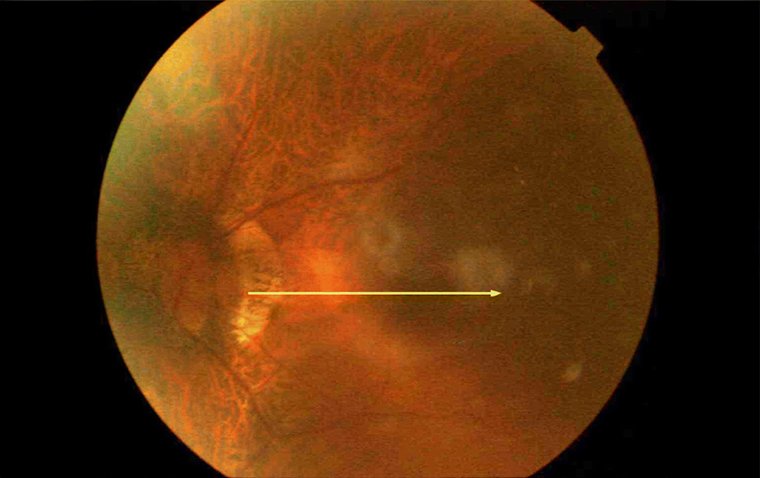
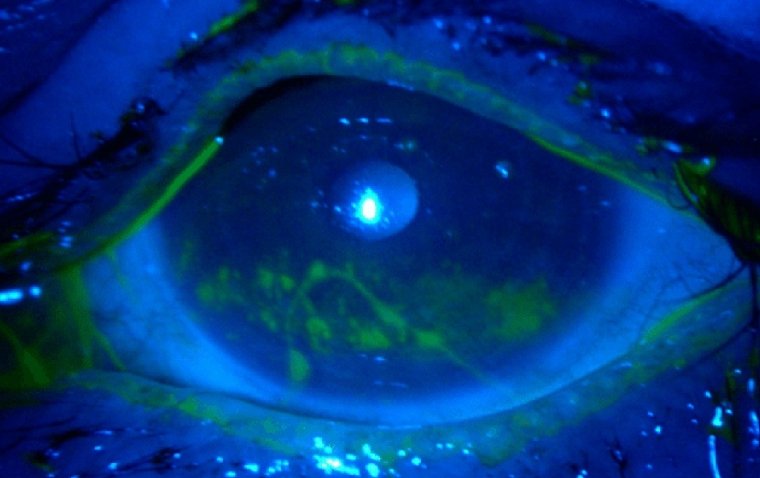
3. Slit-Lamp Examination: A detailed examination of the cornea using a slit lamp provides insights into the corneal shape, thickness, and presence of any scarring or irregularities.
4. Keratometry: This measures the curvature of the cornea's surface. In ectasia, there is often a steepening of the cornea.
5. Corneal Topography: This advanced imaging technique creates a detailed map of the cornea's surface curvature. It is crucial in diagnosing and monitoring the progression of ectasia and keratoconus.
6. Pachymetry: This test measures the thickness of the cornea. Thinning of the cornea is a key indicator of ectasia.
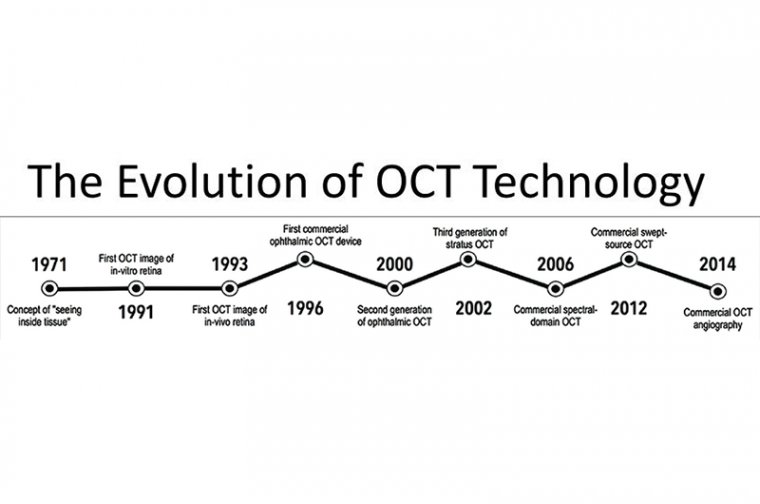
7. Ocular Coherence Tomography (OCT): OCT provides high-resolution images of the cornea and can help in assessing its structure and detecting subtle changes.
8. Genetic Testing: While not routinely done, genetic testing may be recommended
Corneal Ectasia Treatment
Managing Corneal Ectasia involves a range of treatment options, each tailored to the severity and progression of the condition:
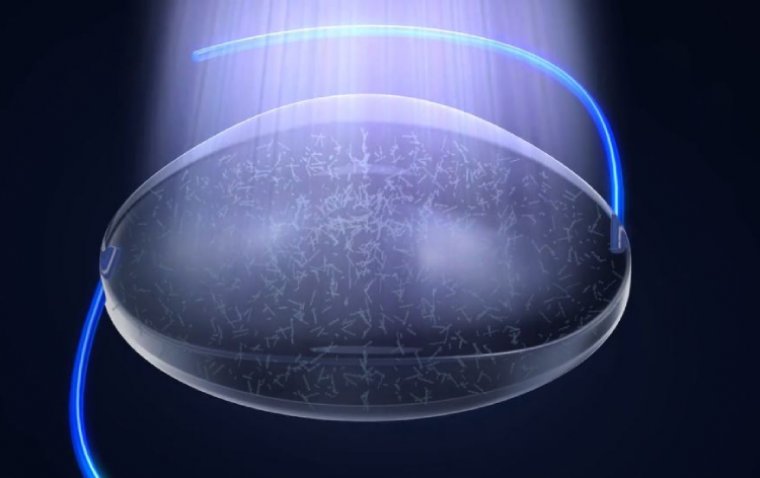
● Corneal Cross-Linking (CXL): A primary treatment, especially for keratoconus, CXL strengthens corneal tissue to halt progression. It involves applying riboflavin (vitamin B2) to the cornea and then activating it with UV light, creating additional cross-links within the corneal collagen fibers.
● Intacs: These corneal ring segments are surgically inserted into the peripheral cornea. They help flatten the cornea's cone-like shape, improving vision and potentially delaying the need for a corneal transplant.
● Surgical Interventions: In advanced cases, surgical options like penetrating keratoplasty (PK) or deep anterior lamellar keratoplasty (DALK) may be considered. These involve replacing part or all of the diseased cornea with healthy donor tissue.
● Contact Lenses: Specialized contact lenses, such as rigid gas-permeable lenses, hybrid lenses, or scleral lenses, are often the first line of treatment to correct the irregular astigmatism and improve vision.
● Topography-Guided Laser Treatment: For certain types of ectasia, particularly post-LASIK ectasia, topography-guided laser treatments can be effective in regularizing the corneal surface.
● Phakic Intraocular Lenses (IOLs): In cases with significant refractive errors, implantable lenses might be an option to improve vision without further stressing the cornea.
● Conservative Management: In early or mild cases, monitoring and managing with glasses or soft contact lenses might be sufficient.
Conclusion
In summary, Corneal Ectasia is a condition marked by progressive thinning and deformation of the cornea, leading to visual distortion and impairment. It encompasses various forms, including Keratoconus, Keratoglobus, Post-LASIK ectasia, Pellucid Marginal Degeneration, and Terrien’s Marginal Degeneration. Each type has its unique characteristics, but they all share the common feature of altering the corneal structure.
The causes of Corneal Ectasia are multifaceted, ranging from genetic predisposition to external factors such as eye rubbing and complications from LASIK surgery. Symptoms typically involve blurred vision, increased light sensitivity, and visual distortions, often leading to a significant impact on daily life.
For diagnosis, a combination of patient history, visual acuity tests, slit-lamp examinations, keratometry, corneal topography, and pachymetry are utilized. These diagnostic tools are essential in not only confirming the presence of ectasia but also in determining its progression and the most effective treatment approach.
Treatment options vary based on the severity and type of ectasia, including corneal cross-linking, Intacs, specialized contact lenses, and in advanced cases, surgical interventions such as corneal transplants. Corneal cross-linking is particularly effective in halting the progression of ectasia, especially in conditions like keratoconus. Intacs and contact lenses are non-invasive options that can significantly improve vision by reshaping the cornea or correcting irregular astigmatism. In severe cases, surgical interventions offer a more definitive solution, although they come with greater risks and a longer recovery period.
References:
(1).jpg)