In Light Of Managing Retrobulbar Hemorrhage
Retrobulbar hemorrhage (RBH) is a rapidly progressive, sight-threatening emergency that results in an accumulation of blood in the retrobulbar space.
The blood accumulation can lead to an increased IOP that may result in stretching of the optic nerve and blockage of ocular perfusion leading to venous and/or arterial occlusive process.
RBH can occur due to orbital trauma, complication of eyelid or orbital surgery, or any process that can affect blood supply to the eye, such as arteriovenous malformations, orbital varicosities, or lymphangiomas. It can be potentiated by the use of anticoagulation medication.
The diagnosis of RBH is clinical and depends on the history of the patient. Diagnostic clues of RBH include severe pain, difficulty opening the lids, proptosis and/or loss of vision.
If patients are victims of trauma, periorbital ecchymosis and eyelid hematoma may be seen.
Due to the severity of RBH and the possibility of vision loss, imaging modalities are usually not recommended for initial diagnostic purposes, as this is a clinical diagnosis and treatment must be prompt.
However, a CT scan can be useful to visualize the orbits, particularly to rule out concomitant injuries in cases of trauma or when the origin of the bleeding is unknown.
Retrobulbar haemorrhage (RBH) is an ocular emergency that occurs due to arterial bleeding in the orbital cavity behind the eye.
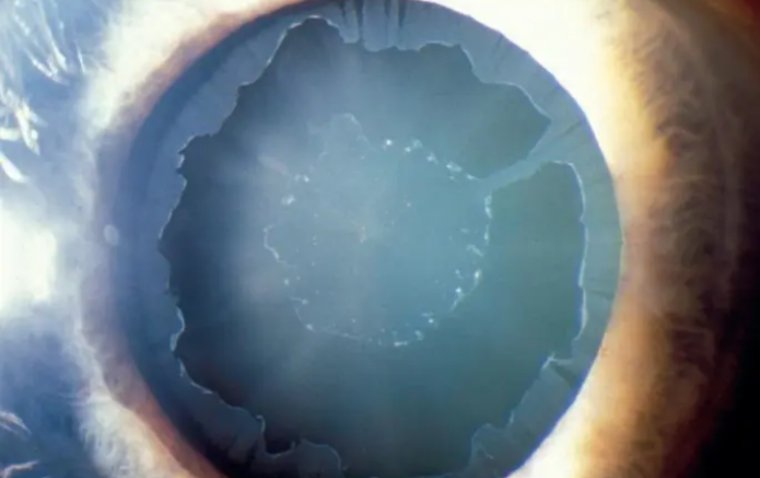
As the orbit is predominantly an enclosed space, the increasing blood volume leads to an increase in intraorbital and intraocular pressure, referred to as orbital compression syndrome.
The overall incidence of RBH is lower than 1%, while the incidence of RBH in orbital trauma is 3.6%. However, despite a low rate of occurrence, the lack of immediate management can lead to major morbidity for the patient, most notably irreversible visual loss.
Most commonly, RBH can occur following facial trauma resulting in orbital fractures, eyelid surgery (lower blepharoplasty, retrobulbar anesthesia) and / or retrobulbar / peribulbar injections.
Pathophysiology
RBH develops due to rupture of any of the orbital arteries such as the infraorbital artery, anterior ethmoidal artery or posterior ethmoidal artery that can cause an increase in intraorbital pressure and a reduction in the perfusion of the optic nerve.
This ischaemia can cause atrophy of the optic nerve and lead to irreversible vision loss.
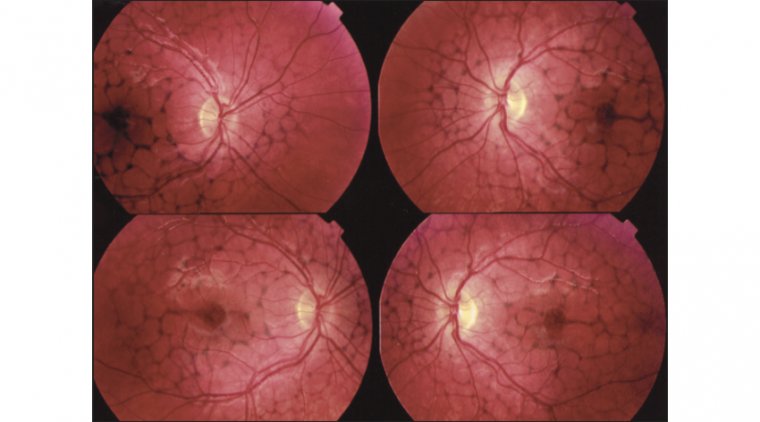
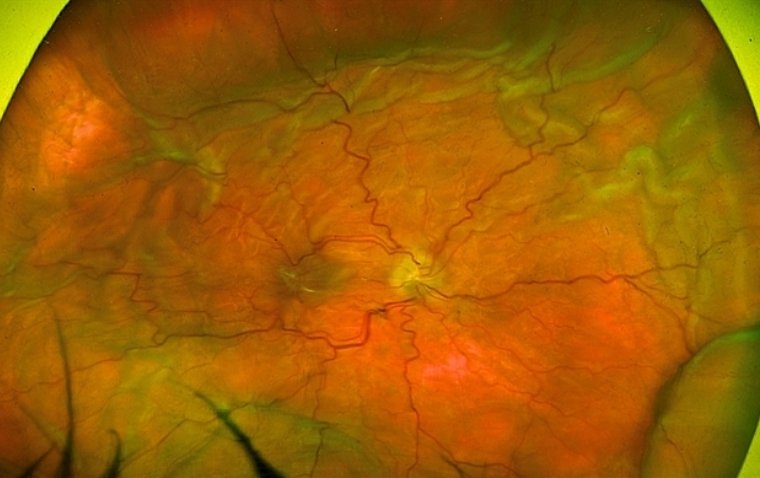
The clinical features of RBH include proptosis, eye pain, reduced visual acuity, ophthalmoplegia, periorbital oedema, subconjunctival ecchymosis, “Cherry red” macula in retina, oedematous and pale optic disc and relative afferent pupillary defect (RAPD).
If these signs are not recognised early, the outcome can be devastating leaving a person visually impaired or blind in that eye. Prevention, recognition and intervention are therefore imperative.
Management
Although a computerised tomography (CT) scan of the orbits is the diagnostic test of choice, management should not be delayed waiting for investigation.
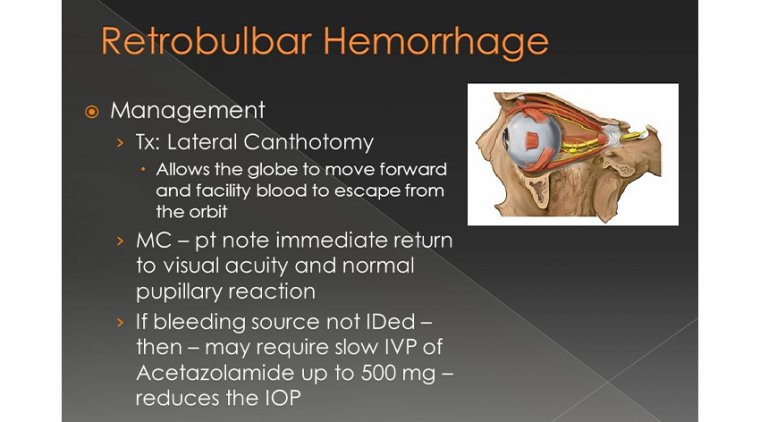
Management is based on the clinical presentation of the patient. If signs of visual compromise and a tense globe is observed, the patient should undergo an emergency lateral canthotomy / lateral cantholysis procedure.
If no signs of visual compromise, manage conservatively with close observation, refer to ophthalmology and medical management can be commenced concurrently.
Conservative Management
- Admit patient
- Position in a head-up position
- Monitor visual acuity, intraocular pressure (IOP) and RAPD every 15 minutes for two hours, then 30 minutes for the next four hours, then hourly.
Medical Management
• Acetazolamide
- Adult, oral/IV, initial dose of 250-500mg. Maintenance, 250mg every four hours as required, to a maximum of 1g daily (see Acetazolamide Prescribing and Administration Guideline)
- Used to reduce intraocular pressure
- Confirm no allergies to sulfa medications
- Mannitol
- Adult 1-2g/kg (5-10mL/kg of 20% solution) intravenously over 30 to 60 mins (see Mannitol Infusion Procedure). Administer with caution to patients with renal / heart disease or severe dehydration
- Used to reduce the volume of vitreous.
Surgical Management
In the surgical management of RBH, patients with visual compromise should have a lateral canthotomy / lateral cantholysis procedure done.
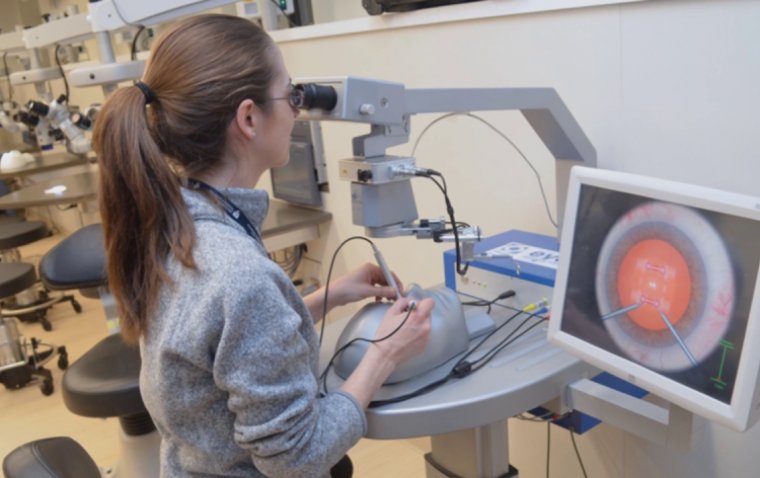
- Lateral canthotomy: take blunt tipped scissors and cut the lateral canthus skin all the way to the bony orbit, with the blades straddling the lateral canthus.
- Lateral cantholysis (inferior crus): use forceps to pull the outer edge of the lower lid out to expose the lateral canthal tendon. Then identify the inferior crus of the lateral canthal tendon inferolaterally.
Using blunt tipped scissors place one blade on either side of the inferior crus of the lateral canthal tendon. When it is cut, the lower lid should become more relaxed. A cantholysis is usually adequate to decompress the orbit.
If not, consider whether you have properly cut the inferior crus or if you need to cut the superior crus.
The following equipment are required to perform a lateral canthotomy / lateral cantholysis procedure:
- Sterile gloves, gauze, face shield, gown and drapes
- Antiseptic solution (chlorhexidine or Betadine)
- Local anaesthetic (2% lignocaine with 1:200,000 adrenaline) into lateral canthus
- Syringe (3ml) with small injection needles available (27-30 gauge)
- Irrigation fluid (normal saline or water)
- Artery forceps
- Sterile curved scissors or iris scissors (whatever is available in the A/E on the day)
- Forceps (at least 0.3mm teeth)
- Antibiotic ointment (chloramphenicol).
After a lateral canthotomy / cantholysis procedure the patient’s eye may be left to spontaneously granulate and heal or may be electively repaired. Incisions heal on their own with minimal scarring.
Apply ointment 1% Chloramphenicol to the eye and cover with a sterile dressing to prevent infection. Ice packs may be used in the days following canthotomy to reduce pain and inflammation.
RBH is a site-threatening emergency, if the symptoms of visual compromise are identified early and treatment is started promptly, patients will have the best chance of recovery.
Although the incidence of RBH may appear to be insignificant, the misdiagnosis or mismanagement can be disastrous due to the risk of permanent blindness.
(1).jpg)