Pseudoexfoliation Syndrome: Understanding Causes, Diagnosis, and Treatment
About Pseudoexfoliation Syndrome
Pseudoexfoliation syndrome (PEX) is a systemic disorder characterized by the abnormal production and accumulation of fibrous extracellular material in various parts of the body, including the eyes. This condition is most commonly known for its impact on ocular health, where these deposits commonly accumulate on the lens, iris, and other structures within the eye's front (anterior) segment.
PEX is a significant risk factor for a variety of ocular conditions, such as glaucoma, lens dislocation, and cataract, and can complicate cataract surgery. Moreover, it has a widespread prevalence, being reported in all races and regions worldwide, although it is more commonly seen in individuals over 60.
In the context of ocular health, understanding PEX is crucial, as it can have far-reaching effects on vision and overall eye function. Recognizing the causes, symptoms, and available treatment options can help those affected manage the condition more effectively.
Causes and Risk Factors of Pseudoexfoliation Syndrome
The exact cause of pseudoexfoliation syndrome (PEX) is yet to be fully understood. However, both genetic and environmental factors seem to play crucial roles in its development.
Research has linked certain genetic predispositions to the condition, highlighting a particular gene (LOXL1) that's believed to be associated with PEX. While this gene is common in the general population, specific variants appear more frequently in people with PEX, suggesting a genetic component to the syndrome. It's worth noting that not everyone with these gene variants will develop PEX, indicating that other factors may also contribute.
In terms of environmental factors, some studies have found associations between PEX and exposure to specific climatic conditions, such as high UV radiation. Others have suggested links with cardiovascular diseases, hearing loss, and cerebrovascular diseases.
It's important to remember that these findings are based on associations, and more research is needed to fully establish causal relationships. Furthermore, age is a significant risk factor for PEX, with the syndrome being more prevalent in individuals over 60.
Identifying Pseudoexfoliation Syndrome: Diagnosis and Symptoms
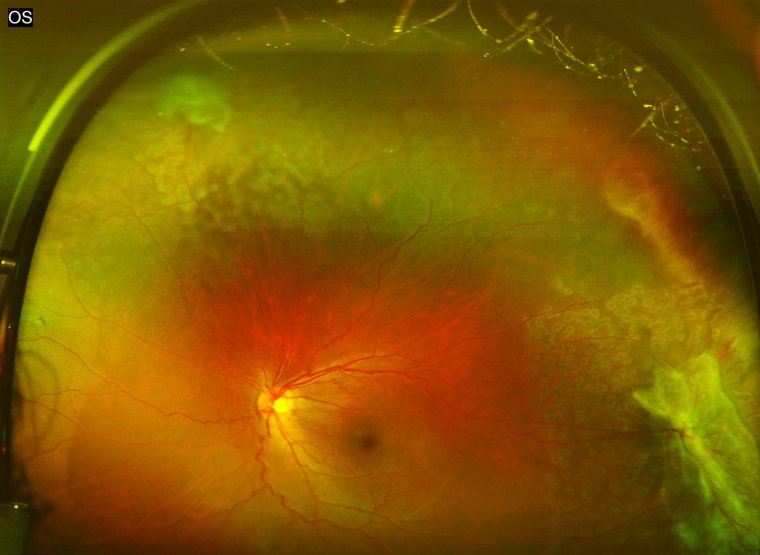
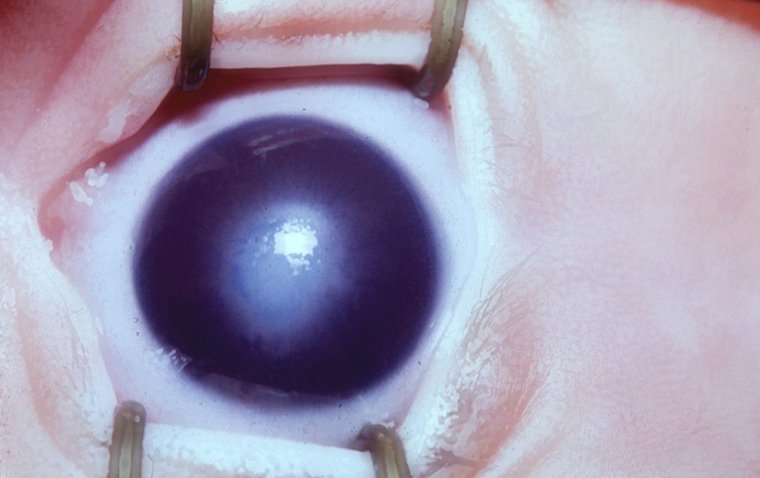
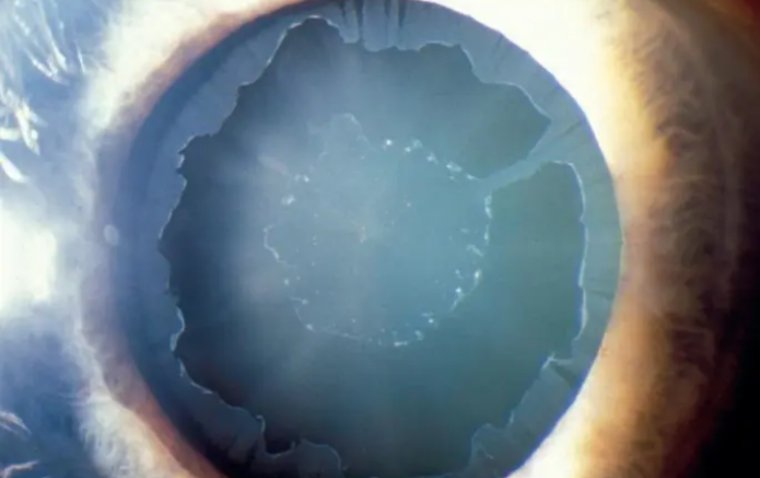
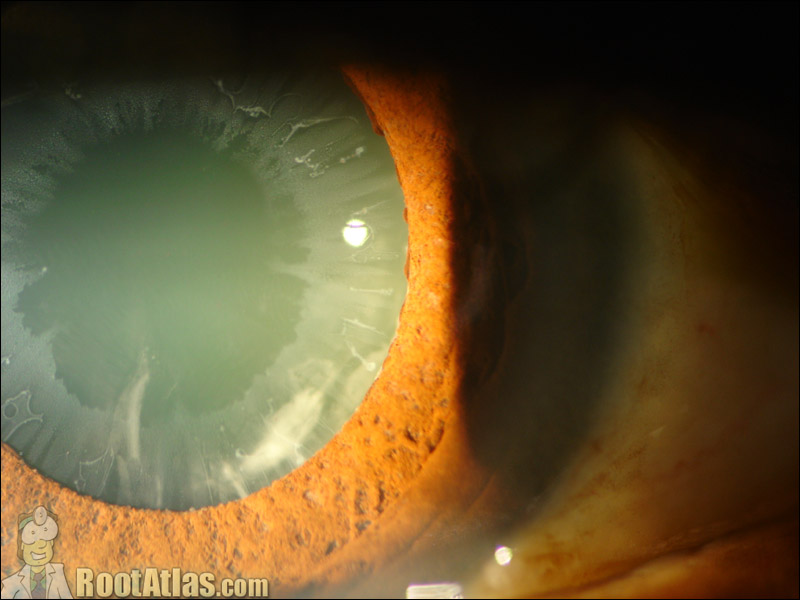
Diagnosis of pseudoexfoliation syndrome (PEX) usually involves a comprehensive eye examination conducted by an ophthalmologist. The most characteristic symptom of PEX is the presence of white, flaky material on the lens and the structures of the front part of the eye. This material is often observed during a slit-lamp examination - a test that uses a special microscope and light source to examine different parts of the eye.
In addition to the white deposits, patients with PEX may exhibit symptoms related to other eye conditions, such as glaucoma or cataracts, which are frequently associated with PEX. Increased intraocular pressure, a key indicator of glaucoma, may be present, while signs of cataracts include clouding of the lens and blurred vision.
It's important to note that PEX can be asymptomatic in its early stages, meaning individuals may not experience any noticeable symptoms until the condition has advanced. This makes regular eye exams crucial, especially for older adults and those with a family history of PEX or related eye conditions.
Associated Eye Conditions and Complications
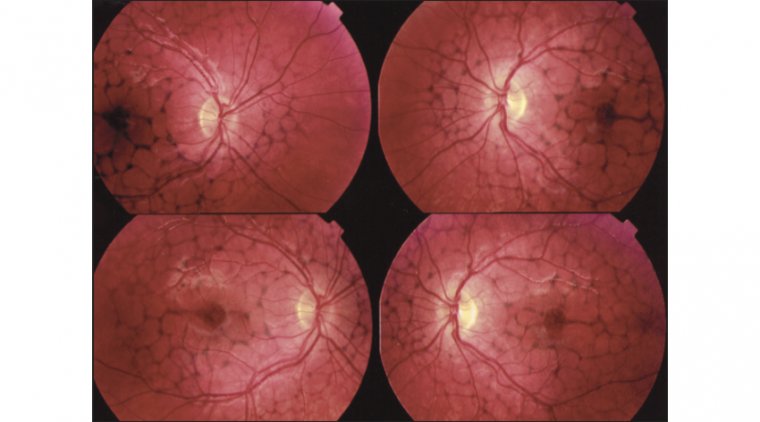
Pseudoexfoliation syndrome (PEX) is associated with a number of eye conditions and potential complications that can significantly affect ocular health. It is most notably linked with pseudoexfoliation glaucoma, which is a type of secondary open-angle glaucoma. The white, flaky material characteristic of PEX can block the eye's drainage system, leading to increased intraocular pressure, a hallmark of glaucoma. This can cause optic nerve damage and, if left untreated, vision loss.
Additionally, PEX is often associated with cataracts. The presence of pseudoexfoliative material can interfere with the normal functioning of the lens, causing it to become cloudy over time. Cataracts in PEX patients are known to progress more rapidly and can make cataract surgery more challenging due to weakened zonular fibers, which secure the lens in place.
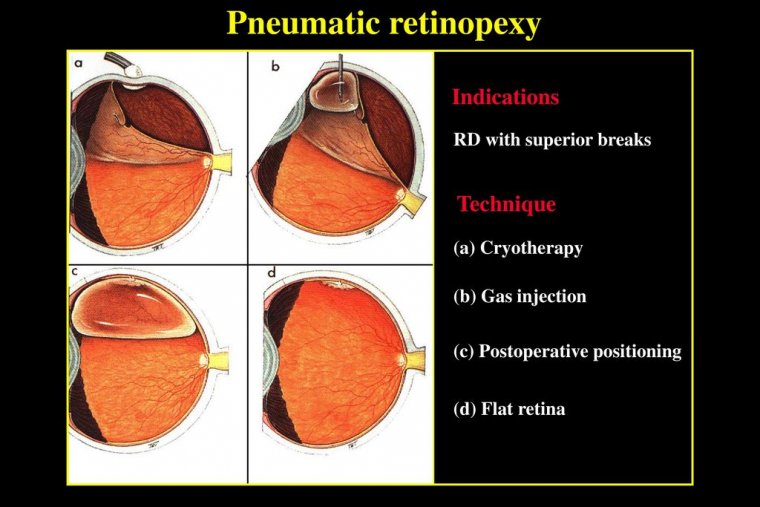
Further, PEX can lead to complications such as lens subluxation or dislocation, due to the weakening of the fibers holding the lens. In rare cases, it can cause complications in the cornea and retina, leading to conditions such as keratopathy and retinal vein occlusion.
Treatment Approaches for Pseudoexfoliation Syndrome
The management of pseudoexfoliation syndrome (PEX) primarily focuses on the treatment of associated conditions and potential complications, such as pseudoexfoliation glaucoma and cataracts. Regular monitoring is crucial to detect these associated conditions early, as PEX itself does not have specific treatments.
In the case of pseudoexfoliation glaucoma, the first line of treatment typically involves the use of topical eye medications to lower intraocular pressure. These medications function by reducing the production of aqueous humor (the eye's clear fluid) or by improving its outflow. Examples of these drugs include beta-blockers, prostaglandin analogs, and carbonic anhydrase inhibitors. However, if these are insufficient to control intraocular pressure, oral medications or surgical interventions may be necessary.
For patients with cataracts linked to PEX, cataract surgery is often required. However, due to the potential for zonular weakness and lens instability, surgeons often take extra precautions during the operation, such as using special devices to stabilize the lens during surgery.
Furthermore, there is ongoing research into understanding the underlying mechanisms of PEX and developing targeted treatment strategies. This includes exploring the role of antioxidants and other medications that might help to reduce the production of pseudoexfoliative material.
Preventative Measures and Lifestyle Recommendations
While the exact cause of pseudoexfoliation syndrome (PEX) is unknown and specific preventative measures have not been established, maintaining overall eye health can be beneficial. Regular eye exams are vital, particularly for those in the high-risk category, such as individuals of Nordic descent and the elderly. These regular check-ups can lead to early detection and treatment of any associated conditions like glaucoma or cataracts, thus preventing further complications.
Lifestyle adjustments that promote general eye health can also be beneficial. This includes wearing sunglasses to protect the eyes from harmful UV rays, maintaining a balanced diet rich in fruits, vegetables, and fish (which are high in antioxidants and omega-3 fatty acids), and managing systemic health conditions like diabetes and hypertension that can affect eye health.
Research and Future Directions
Research into pseudoexfoliation syndrome is currently an active field, with scientists striving to unravel the genetic and environmental factors that contribute to its development. Some studies are examining the role of oxidative stress in PEX, which could lead to new treatment strategies aimed at reducing oxidative damage in the eye.
Genetic research is another promising area, with some studies identifying specific genes that may increase susceptibility to PEX. This could lead to improved screening methods and potentially even gene therapies in the future.
Furthermore, advanced imaging techniques are being studied for their ability to detect PEX at its earliest stages, which could lead to earlier intervention and better patient outcomes.
Summary
Pseudoexfoliation syndrome (PEX) is a multifactorial condition marked by distinctive microscopic deposits on the front part of the eye lens and other areas. Its cause remains uncertain, but both genetic and environmental factors are thought to play a role. Early detection is critical in managing this condition, as it's often associated with other eye diseases, including glaucoma and cataracts.
Regular comprehensive eye examinations, particularly for individuals within the high-risk groups, are essential for early identification of PEX and its associated conditions. Although there's no definitive cure for PEX, various treatment options are available that primarily target associated conditions and aim to prevent further complications. This includes both medical and surgical interventions, which can help manage intraocular pressure and mitigate the risk of vision loss.
Living a lifestyle that promotes good eye health, alongside adhering to professional eye care recommendations, can contribute significantly towards managing this condition. Meanwhile, scientific research continues to uncover more about PEX, offering hope for more advanced diagnostic tools and effective treatment strategies in the future.
It's crucial to consult with eye care professionals to ensure personalized treatment and management strategies. Their advice can be invaluable in navigating the complexities of PEX and enhancing the overall quality of life for those affected by this condition.
(1).jpg)