Inflammatory Glaucoma: An Overview of a Complex Condition
What Is Inflammatory Glaucoma?
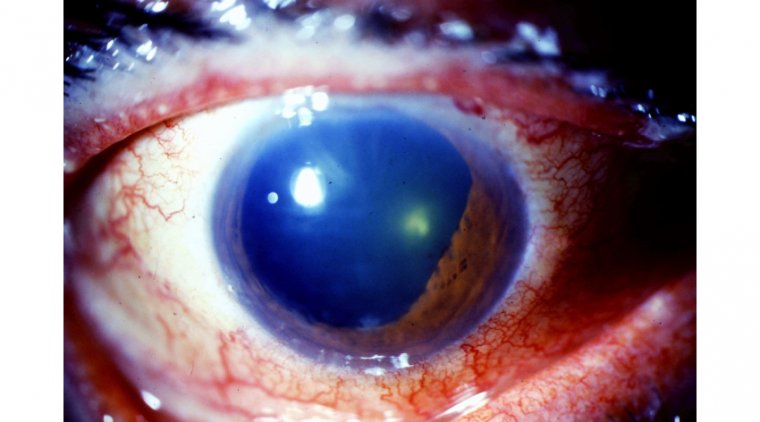
Inflammatory Glaucoma, also defined as Uveitic Glaucoma, is a disorder in which persistent or recurring IOP elevation results in morphological and physiological alterations of optic disc typical of primary open-angle Glaucoma. Inflammation of the ocular tissues is the cause of continuous or repeated elevations in intraocular pressure (IOP) in inflammatory Glaucoma. Extreme cases of elevated intraocular pressure may accompany optic nerve cupping, neuroretinal rim loss, and visual field abnormalities.
Uveitic Glaucoma can be observed in the subsequent inflammatory disorders:
●Posner-Schlossman syndrome
●Fuch’s heterochromic Iridocyclitis
●Syphilis
●Sarcoidosis
●Juvenile Rheumatoid Arthritis
●Herpes Simplex Kerato-uveitis
●Varicella Zoster Iridocyclitis
●Vogt-Koyanagi-Harada Syndrome
●Ocular Toxoplasmosis
●Scleritis and Episcleritis
Diagnosis Of Inflammatory Glaucoma
Diagnosis of inflammatory Glaucoma is clinical. Any patient with recurrent or bilateral uveitis should have an ocular or systemic etiology investigated. It is necessary to do an appropriate systemic evaluation, focusing on arthritis, infections, mucosa or skin lesions, and respiratory symptoms. All patients may benefit from a complete blood count and syphilis serology, while those of African heritage may need angiotensin-converting enzyme test and a chest X-ray.
Following points must be kept in mind during diagnosis of inflammatory glaucoma:
●Ocular History
●Systemic History (Including infective, inflammatory, or autoimmune conditions)
●Visual acuity and refraction
●Slit Lamp Examination
●Tonometry
●Gonioscopy
●OCT-RNFL to determine damage by Glaucoma
Signs And Symptoms of Inflammatory Glaucoma
General Clinical Features:
●Blurred Vision
●Ocular pain
●Brow ache
●Photophobia
●Coloured haloes
●Elevated IOP
●Optic nerve head changes
Specific Clinical Features:
Clinical Features and Treatment of Inflammatory Glaucoma depend on its type, as each type has its own pathophysiology.
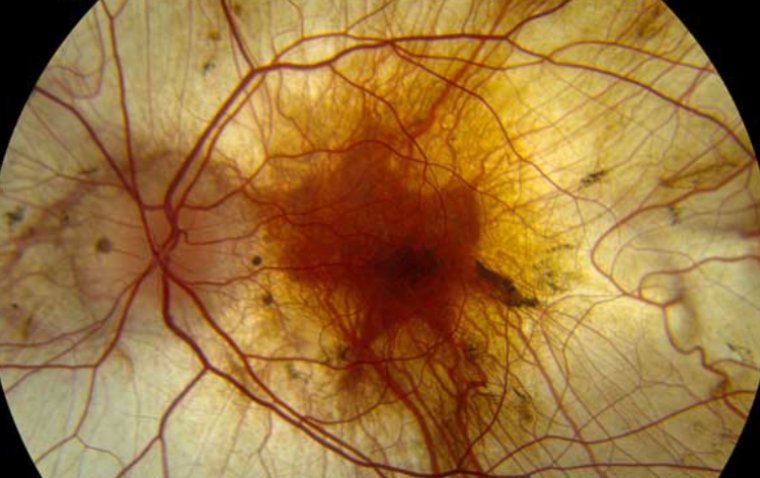
Open-Angle type: This type of inflammatory Glaucoma is due to acute trabeculitis causing inflammation and edema of the trabecular meshwork. Following signs might be observed in its cases:
●Flares and cells in the AC
●Posterior Synechiae
●Keratic precipitates (KP)
●Irregular and small pupil
●Mashed potato-like membrane in the trabecular
Angle-Closure type: Chronic anterior uveitis causes deposition and contraction of inflammatory debris in the anterior angle. This inflammatory condition causes pulling of the iris over the trabecula and 360° PS (seclusio pupillae), which causes angle closure and obstruction to aqueous humour flow. Following signs might be observed in its cases:
●Shallow AC
●Signs of previous inflammatory episodes
●360-degree posterior synechiae
Secondary to Posner-Schlossman syndrome:
●Painless decrease visual acuity with haloes
●White-eye
●Raise of IOP (may go around 40-80mmHg)
●No synechiae
●Occasional cells/KPs
●Open-angle
Secondary to Fuch’s heterochromaic Iridocyclitis
●Decrease in VA due to cataract (posterior cortical/subcapsular)
●Floaters
●White stellate KPs over corneal endothelium
●Mild flare
●Iris heterochromia
●Open-angle +/- NVA
How Can It Be Treated?
Treatment of inflammatory Glaucoma depends upon three pillars.
1. Treatment of inflammation: The primary objectives of inflammatory treatment are to give symptomatic relief, prevent the formation of posterior synechiae, and decrease the intensity and frequency of bouts or exacerbations of uveitis.
●Corticosteroids (Topical,Intravitreal,Systemic,Periocular)
●Cycloplegics
●Antimetabolites like methotrexate
●T cell suppressors like cyclosporine
●Cytotoxic agents like cyclophosphamide
2. Treatment of Glaucoma by antiglaucoma therapy:
●Beta Blockers
●Carbonic Anhydrase Inhibitors
●Selective alpha 2 adrenergic agonists
●Prostaglandins analogs
●Miotics
●Hyperosmotic agents
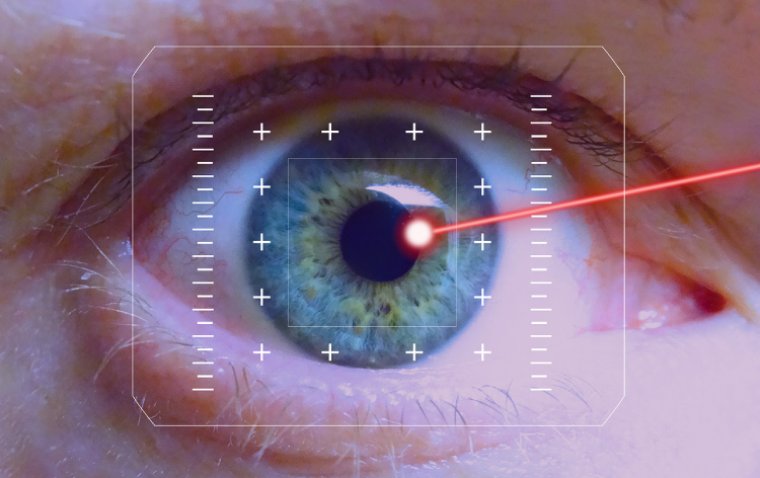
3. Surgical Treatment
Ophthalmologists should avoid intraocular surgery in eyes with current inflammation. However, when medical treatment is ineffective, surgery may be necessary. It is best to perform as minor surgery as possible in these situations. Recent research has proven the following techniques to be of some value:
●Laser Iridotomy
●Antimetabolite Therapy in association with trabeculectomy
Author: Dr. Muhammad Saad, Resident Ophthalmologist at Al-Shifa Trust Eye Hospital in Rawalpindi, Pakistan
(1).jpg)