Chronic Progressive External Ophthalmoplegia (CPEO)
What is Chronic Progressive External Ophthalmoplegia?
Chronic Progressive External Ophthalmoplegia (CPEO) is a neurological disorder characterized primarily by the gradual weakening of the eye muscles. Classified under mitochondrial myopathies, CPEO stems from abnormalities in the mitochondria, which are the energy-producing structures within cells. This disorder is progressive, meaning that the symptoms typically worsen over time.
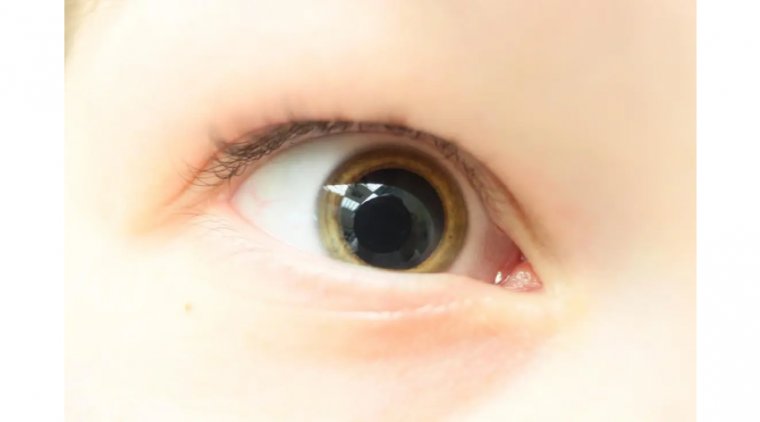
The hallmark of CPEO is the progressive weakening of the external ocular muscles, the muscles that control eye movements. As these muscles become increasingly weakened, individuals with CPEO often experience symptoms such as ptosis (drooping of the eyelids), difficulty in moving the eyes, and, in some cases, double vision (diplopia). The term 'external' distinguishes the condition from diseases affecting the internal ocular muscles responsible for controlling the pupil and lens.
Causes and Risk Factors of Chronic Progressive External Ophthalmoplegia
Causes of Chronic Progressive External Ophthalmoplegia
1. Mitochondrial DNA Mutations: The most common cause of CPEO is mutations in the mitochondrial DNA. Unlike nuclear DNA, which is inherited from both parents, mitochondrial DNA is inherited exclusively from the mother. Mutations in mtDNA can impair the mitochondria's ability to produce energy, particularly affecting tissues with high energy demands, like muscle tissues.
2. Kearns-Sayre Syndrome (KSS): CPEO can be a feature of Kearns-Sayre Syndrome, a more severe mitochondrial disorder that begins in childhood. KSS is also associated with mtDNA deletions.
3. Secondary to Other Mitochondrial Disorders: In some cases, CPEO can occur as part of other mitochondrial syndromes, which might involve additional symptoms affecting different body systems.
Risk Factors Associated with Chronic Progressive External Ophthalmoplegia
● Genetic Factors: The primary risk factor for CPEO is a family history of mitochondrial diseases. The maternal inheritance pattern of mtDNA means that if the mother carries mtDNA mutations, there is a risk of passing these to her children.
● Age of Onset: While CPEO can appear at any age, it typically manifests in young adulthood. The progression of symptoms is usually slow.
● Environmental Factors: There is ongoing research into whether environmental factors might contribute to the manifestation or progression of mitochondrial diseases like CPEO. However, this area is still not fully understood.
● Associated Systemic Disorders: Individuals with systemic disorders linked to mitochondrial dysfunction might have a higher risk of developing CPEO as part of their condition.
Symptoms of Chronic Progressive External Ophthalmoplegia
Chronic Progressive External Ophthalmoplegia (CPEO) presents with a distinctive set of symptoms primarily affecting the eyes, although the severity and progression can vary among individuals. The characteristic features of CPEO include:
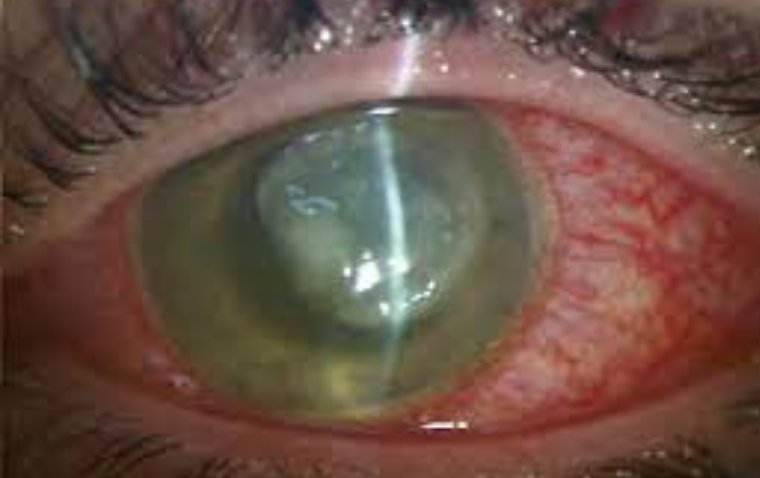
1. Ptosis (Drooping Eyelids): One of the most noticeable symptoms of CPEO is ptosis, where the upper eyelids droop. This occurs due to the weakening of the levator muscles, which are responsible for lifting the eyelids. Ptosis in CPEO is typically bilateral and progressive. As the condition advances, the drooping may become severe enough to impair vision.
2. Ophthalmoplegia (Eye Muscle Weakness): CPEO involves the gradual weakening of the extraocular muscles that control eye movement. This leads to ophthalmoplegia, where patients have difficulty moving their eyes. The weakness usually affects all directions of eye movement and can lead to fixed, straight-ahead gaze.
3. Double Vision (Diplopia): As the eye muscles weaken unevenly, patients may experience double vision. This occurs because the eyes are no longer able to move in coordination, leading to misalignment and the perception of two images of a single object. However, as the disease progresses and eye movements become more limited, double vision may actually improve or disappear because the eyes no longer move enough to cause significant misalignment.
4. Slow Progression: The symptoms of CPEO typically develop slowly over years. Initially, the symptoms might be mild and only gradually become more noticeable.
5. Possible Systemic Involvement: In some cases, CPEO can be part of a broader systemic mitochondrial disorder, which may present additional symptoms such as muscle weakness in other parts of the body, hearing loss, or neurological deficits.
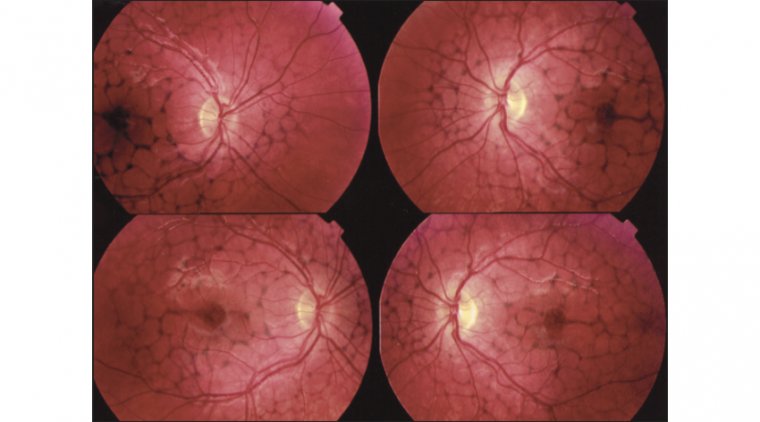
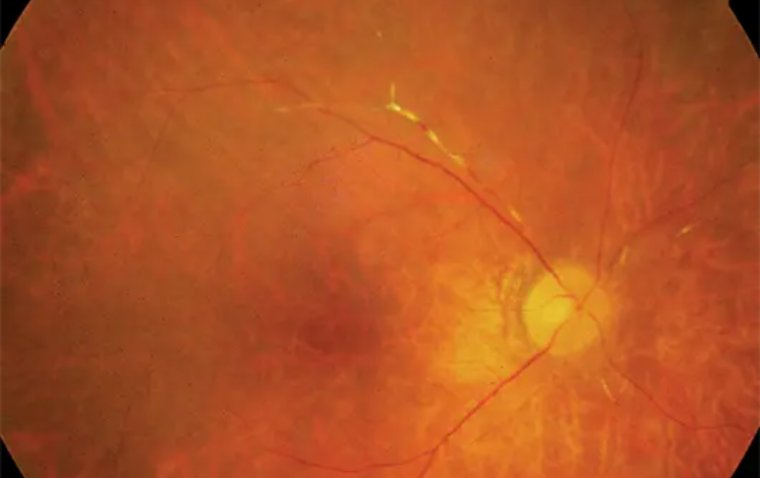
6. Rarely, Retinal or Cardiac Involvement: Although less common, some individuals with CPEO may experience retinal changes or cardiac conduction defects, depending on the extent of mitochondrial dysfunction.

Diagnosis and Medical Evaluation
The diagnosis of Chronic Progressive External Ophthalmoplegia (CPEO) is a multifaceted process that involves a combination of clinical evaluation, ophthalmologic examinations, muscle biopsies, and genetic testing. Given the progressive and variable nature of CPEO, establishing an accurate diagnosis is essential for appropriate management and treatment. Here's an overview of the diagnostic process:
Ophthalmologic Examination
● Clinical Assessment: The first step often involves a detailed clinical evaluation, focusing on the patient's symptoms, medical history, and family history. The presence of characteristic symptoms such as ptosis and ophthalmoplegia is a key indicator.
● External Eye Examination: This includes an assessment of eyelid function and eye movement. Special attention is given to the degree of ptosis and the range of ocular motility.
● Slit-Lamp Examination: To assess the health of the anterior segment of the eye, ensuring that the symptoms are not related to other ocular conditions.
Muscle Biopsy
● Histological Analysis: A muscle biopsy, usually taken from a limb rather than the eye muscles, is a crucial diagnostic tool. Histological analysis can reveal ragged red fibers, a hallmark of mitochondrial dysfunction.
● Electron Microscopy: This can provide detailed images of the muscle tissue, revealing abnormalities in the mitochondria.
● Enzyme Assays: To assess mitochondrial function, enzyme assays might be performed on the muscle tissue.
Genetic Testing
● Mitochondrial DNA Analysis: Since CPEO is often associated with mitochondrial DNA mutations, genetic testing can be a valuable diagnostic tool. This can identify specific genetic mutations known to cause mitochondrial disorders.
● Nuclear DNA Testing: In some cases, nuclear genes affecting mitochondrial function may also be involved, necessitating broader genetic testing.
Additional Diagnostic Criteria
● Electrophysiological Tests: Tests like electromyography (EMG) can assess the electrical activity of muscles and nerves, which might be altered in mitochondrial myopathies.
● Cardiac Evaluation: Given the potential for cardiac involvement in mitochondrial disorders, a cardiac evaluation including ECG and echocardiography may be recommended.
● Systemic Assessment: If systemic symptoms are present, further evaluations to assess other potentially affected organs (like the brain, peripheral nerves, or muscles) may be necessary.
● Exclusion of Other Conditions: It's also important to rule out other conditions that might mimic the symptoms of CPEO, such as myasthenia gravis or other ocular motility disorders.
How is CPEO Treated?
Chronic Progressive External Ophthalmoplegia (CPEO) is a condition with no definitive cure, so treatment primarily focuses on managing symptoms, improving quality of life, and addressing any complications that arise. Here are some of the management strategies and treatment approaches for CPEO:
1. Symptomatic Relief
● Ptosis Surgery: For patients with significant ptosis impairing vision, surgical interventions such as blepharoplasty or ptosis repair can be beneficial. These surgeries aim to lift the eyelids to improve the visual field.
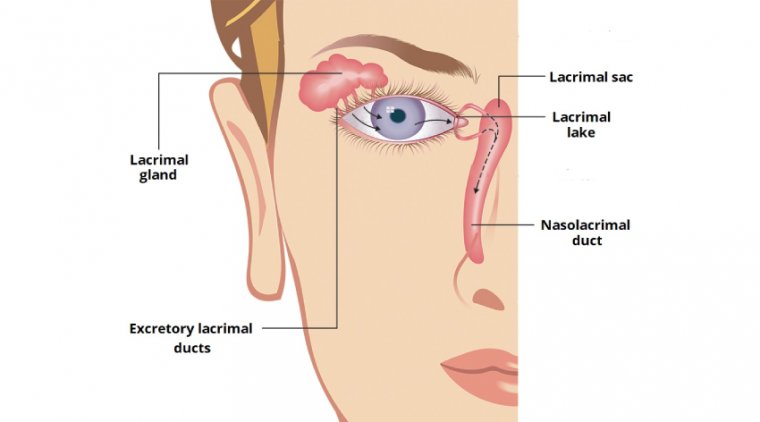
● Palliative Eyecare: Artificial tears and lubricating ointments can be used to manage symptoms of dry eyes, which are common due to incomplete blinking and reduced tear production.
● Prism Glasses: For those with diplopia (double vision), prism glasses can help alleviate this symptom by aligning the visual images.
2. Physical Therapy
● Eye Muscle Exercises: Although limited in effectiveness for CPEO, exercises may be recommended to maintain as much muscle function as possible.
● General Physical Therapy: For patients with muscle weakness beyond the ocular muscles, physical therapy can help maintain muscle strength and flexibility.
3. Mitochondrial Disease Management
● Vitamin Supplements: Although there is limited evidence, some clinicians recommend supplements like Coenzyme Q10, vitamin K, and vitamin C, which are thought to support mitochondrial function.
● Regular Exercise: Aerobic exercise might be beneficial in improving overall muscle function and endurance.
● Nutritional Support: A balanced diet, potentially with the guidance of a nutritionist, can support overall health and energy levels.
● Monitoring and Managing Complications: Regular monitoring for potential complications, especially cardiac involvement, is crucial. This might involve routine ECGs and cardiology consultations.
● Genetic Counseling: As CPEO can have genetic implications, genetic counseling may be recommended for patients and their families to understand the inheritance patterns and risks.
● Ongoing Research and Experimental Therapies: Participation in clinical trials for new treatments or therapies may be an option for some patients.
4. Multidisciplinary Care
● Regular Ophthalmologic Evaluations: Ongoing assessments by an ophthalmologist are crucial for monitoring the progression of ocular symptoms and adjusting treatment as necessary.
● Coordination with Other Specialists: Since CPEO can be part of a broader mitochondrial disorder, care may involve a team of specialists, including neurologists, cardiologists, and geneticists.
Complications Associated with CPEO
While Chronic Progressive External Ophthalmoplegia (CPEO) primarily affects the muscles controlling eye movements and eyelid function, it can also be associated with several other complications, especially when it is part of a broader systemic mitochondrial disorder. These complications can significantly impact the quality of life and overall health of individuals with CPEO.
Respiratory Challenges
● Respiratory Muscle Weakness: In some cases, CPEO can affect the muscles involved in respiration. This can lead to weakened breathing, reduced lung capacity, and difficulty in clearing airway secretions, increasing the risk of respiratory infections.
● Sleep Apnea: There is an increased risk of sleep apnea in individuals with muscle weakness, including those with CPEO. Sleep apnea can lead to fragmented sleep, daytime sleepiness, and further exacerbate any respiratory weakness.
Swallowing Difficulties
● Oropharyngeal Dysphagia: Muscle weakness can extend to the oropharyngeal muscles, leading to difficulties in swallowing (dysphagia). This can result in challenges with eating and drinking, increasing the risk of aspiration and malnutrition.
Other Secondary Health Issues
● Cardiac Involvement: Some individuals with CPEO may experience cardiac complications, such as conduction abnormalities and cardiomyopathy. Regular cardiac evaluations are important to monitor and manage these risks.
● Hearing Loss: Sensorineural hearing loss is another possible complication, necessitating regular auditory assessments and interventions as needed.
● Gastrointestinal Issues: Mitochondrial dysfunction can affect the smooth muscles of the gastrointestinal tract, leading to problems like constipation, gastroparesis, and abdominal discomfort.
● Endocrine Disorders: There is an increased incidence of endocrine disorders such as diabetes mellitus and thyroid dysfunction in individuals with mitochondrial diseases, including those with CPEO.
● Fatigue and Exercise Intolerance: Generalized muscle weakness can lead to significant fatigue and reduced tolerance for physical activity, impacting daily life activities.
● Cognitive and Neurological Issues: Although less common, some individuals might experience cognitive impairments, mood disorders, or other neurological complications.
Research and Advancements in CPEO
The field of Chronic Progressive External Ophthalmoplegia (CPEO) and mitochondrial diseases, in general, is an area of active research, with ongoing efforts aimed at better understanding the disease mechanism and developing more effective treatments. Here are some key areas of research and advancements:
1. Understanding Mitochondrial Dysfunction: A significant focus of research is to gain a deeper understanding of how mitochondrial DNA mutations lead to the symptoms of CPEO. This involves studying the cellular and molecular pathways affected by these mutations.
2. Epidemiological Studies: Research is being conducted to understand the prevalence, risk factors, and natural history of CPEO. This helps in better characterizing the disease and its variations among different populations.
3. Biomarkers Identification: Identifying biomarkers for CPEO is an important research goal. Biomarkers can aid in early diagnosis, monitoring disease progression, and evaluating treatment efficacy.
Potential Gene Therapy Advancements
● Mitochondrial Gene Therapy: Since CPEO is a mitochondrial genetic disorder, gene therapy targeting the mitochondria is a promising area of research. Efforts are being made to develop techniques to introduce healthy DNA into mitochondria or to compensate for the defective genes.
● Nuclear Gene Targeting: Another approach is targeting nuclear genes that influence mitochondrial function. By modifying these genes, it may be possible to alleviate the effects of mitochondrial DNA mutations.
● Personalized Medicine: Advances in genetics are paving the way for more personalized approaches to treatment, where therapies are tailored based on an individual’s specific genetic makeup.
Recent Developments in CPEO Treatment
1. New Medications: Researchers are testing various drugs and supplements that might improve mitochondrial function or protect cells from the damage caused by dysfunctional mitochondria.
2. Stem Cell Research: There is ongoing research into the use of stem cells to treat mitochondrial disorders. This includes the potential to replace damaged cells with healthy ones.
3. Advanced Surgical Techniques: Advancements in surgical techniques for ptosis and strabismus associated with CPEO are continually evolving, aiming to provide better functional and aesthetic outcomes.
4. Clinical Trials: Several clinical trials are underway exploring novel therapeutic approaches, including pharmacological treatments and lifestyle interventions.
5. International Collaboration: There is increased collaboration internationally, with registries and databases being developed to share information, clinical findings, and best practices among researchers and clinicians globally.
Conclusion
In summary, Chronic Progressive External Ophthalmoplegia (CPEO) is a complex condition characterized by progressive weakness of the eye muscles, often accompanied by systemic manifestations due to its mitochondrial origins. While the primary symptoms include ptosis and limited eye movement, the potential for respiratory challenges, swallowing difficulties, and other secondary health issues necessitates a comprehensive and multidisciplinary approach to care.
It's important for individuals with CPEO to engage with supportive communities and healthcare professionals who understand the intricacies of this condition. Resources such as patient advocacy groups, specialized healthcare providers, and up-to-date medical information are invaluable in navigating the challenges of CPEO. Emphasis on early diagnosis, regular monitoring of potential complications, and personalized management strategies can significantly improve quality of life. Individuals living with CPEO are encouraged to stay informed, seek support, and actively participate in their healthcare journey.
References:
https://eyewiki.org/Chronic_Progressive_External_Ophthalmoplegia_(CPEO)
(1).jpg)