Schirmer's Test and Its Implications in Monitoring and Managing Dry Eyes
In the dynamic landscape of ophthalmology, the evaluation of tear production holds a central position in understanding and managing a spectrum of ocular conditions. Among the various tools available, Schirmer's Test, named after the pioneering German ophthalmologist Otto Schirmer, stands out as a fundamental and reliable method for quantifying tear production.
This comprehensive guide aims to delve deeply into the intricacies of Schirmer's Test, unraveling its significance in ophthalmology and its applications, particularly in diagnosing conditions like Dry Eye Syndrome.
What is Schirmer's Test?
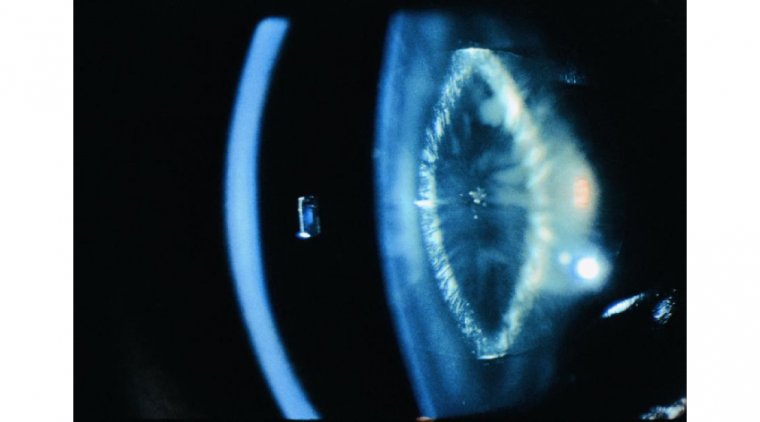
Schirmer's Test represents a cornerstone in the assessment of tear production, offering insights into the eye's ability to produce both basal and reflex tears. The test involves the strategic placement of a specialized filter paper strip into the lower eyelid, without the use of anesthesia. Over a standardized period, typically five minutes, the wetting of the strip is measured, providing a quantitative measure of tear production. This seemingly simple procedure serves as a gateway to understanding the dynamics of tear secretion.
How to Conduct and Interpret Schirmer’s Test
Conducting Schirmer's Test involves a systematic approach to ensure accuracy and reliability. The patient is asked to refrain from using topical medications that may interfere with tear production, and the test is typically performed in a controlled environment to minimize external factors. The Schirmer strip is delicately placed in the lower conjunctival sac, and the patient is instructed to keep their eyes closed to prevent excessive evaporation.
Interpreting the results involves measuring the length of wetting on the strip. A longer wetting length indicates adequate tear production, while a shorter length may suggest an insufficiency in tear secretion. It's important to note that Schirmer's Test assesses both basal and reflex tear production, providing a comprehensive overview of the eye's tear dynamics.

Clinical Significance
Dry Eye Syndrome (DES) stands as one of the most prevalent ocular conditions, affecting millions worldwide. Schirmer's Test plays a pivotal role in diagnosing and managing DES by quantifying tear production. Abnormalities in tear production can lead to a range of symptoms, including ocular discomfort, redness, and blurred vision.
Understanding the clinical significance of Schirmer's Test enables healthcare professionals to tailor treatment plans for patients more effectively. Whether in the context of DES or other ocular surface disorders, the information gleaned from Schirmer's Test guides clinicians in making informed decisions about therapeutic interventions, lubrication strategies, or more specialized treatments.
What are Some Other Applications Beyond Dry Eye?
While Schirmer's Test is synonymous with dry eye evaluation, its applications extend far beyond this common condition. The test proves invaluable in diagnosing a variety of ocular surface disorders, autoimmune diseases affecting the eyes, and systemic conditions that impact tear production.
In the realm of ocular surface disorders, conditions such as conjunctivitis, meibomian gland dysfunction, and ocular allergies can be effectively evaluated using Schirmer's Test. Additionally, the test plays a role in identifying autoimmune diseases, such as Sjögren's syndrome, where dry eyes are a prominent symptom.
Furthermore, systemic conditions like diabetes mellitus and rheumatoid arthritis can manifest with ocular symptoms related to tear production. By incorporating Schirmer's Test into the diagnostic armamentarium, healthcare professionals can enhance their ability to detect and manage a spectrum of ocular conditions, contributing to comprehensive patient care.
Advancements and Innovations
In recent years, the field of ophthalmology has witnessed notable advancements in technology that have augmented the capabilities of tear film evaluation. Digital imaging and artificial intelligence have emerged as promising tools to complement traditional methods such as Schirmer's Test.
Digital imaging systems provide a more detailed and nuanced analysis of tear dynamics, allowing for a visual representation of tear breakup patterns and facilitating a more precise evaluation of the ocular surface. Artificial intelligence algorithms, trained on vast datasets, can assist in the interpretation of tear film dynamics, potentially identifying subtle abnormalities that may escape the human eye.
These innovations not only enhance the accuracy of tear production assessment but also contribute to early detection and intervention, particularly in conditions where subtle changes in tear film dynamics may precede overt clinical symptoms. Integrating these technological advancements with Schirmer's Test offers a more holistic approach to tear film evaluation in the modern era of ophthalmology.
Practical Considerations and Tips
For healthcare professionals conducting Schirmer's Test, certain practical considerations can enhance the reliability of the results. Patient preparation is key, and ensuring that the patient refrains from using medications that could affect tear production is paramount. Additionally, conducting the test in a controlled environment minimizes external factors that could influence the results.
The discomfort associated with Schirmer's Test is a common concern for patients. Sensitizing them to the nature of the test and explaining its importance in diagnosing and managing ocular conditions can alleviate anxiety. Moreover, emphasizing the non-invasive nature of the procedure and its short duration contributes to a more positive patient experience.
Interpreting the results requires a nuanced understanding of the factors that can influence tear production. External factors such as temperature, humidity, and airflow in the testing environment can impact results. By being mindful of these variables and ensuring standardized testing conditions, healthcare professionals can obtain more accurate and reproducible results.
Summary
In conclusion, Schirmer's Test stands as an indispensable tool in the armamentarium of ophthalmic diagnostics. This comprehensive guide has provided an in-depth exploration of its fundamentals, procedural intricacies, clinical applications, and recent technological advancements. By integrating Schirmer's Test into routine eye examinations, healthcare professionals can more accurately diagnose and manage a spectrum of conditions affecting tear production.
The clinical significance of Schirmer's Test, particularly in the context of Dry Eye Syndrome, highlights its role as a frontline diagnostic tool. Beyond DES, the test's applications in diverse ocular surface disorders and systemic conditions underscore its versatility in clinical practice.
As technology continues to advance, the integration of digital imaging and artificial intelligence with Schirmer's Test propels the field of tear film evaluation into new frontiers. These innovations not only enhance the accuracy of diagnosis but also contribute to a more proactive and personalized approach to patient care.
By adhering to practical considerations and tips, healthcare professionals can ensure the reliability of Schirmer's Test results, fostering a positive patient experience and facilitating more effective management strategies.
(1).jpg)