Spotlight on Bull's Eye Maculopathy: What You Need to Know
What Is Bull’s Eye Maculopathy?
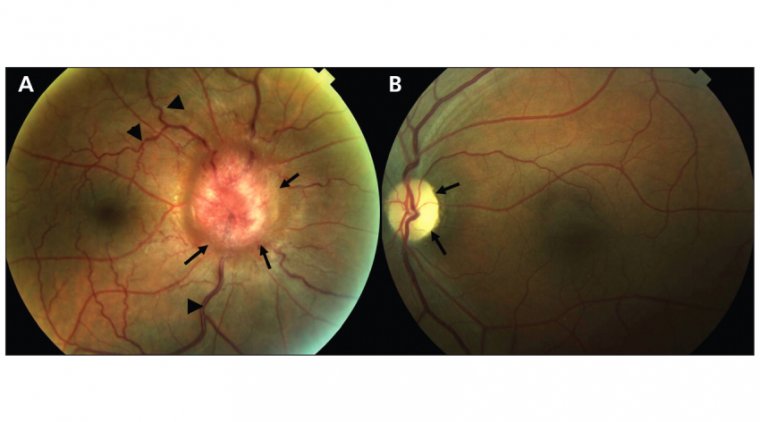
Bull's Eye Maculopathy is a specific form of retinal disease characterized by changes in the pigmentation of the macular region of the retina, often presenting as a 'bull's eye' pattern. The macula is the central area of the retina responsible for detailed, central vision. When affected, it can severely compromise a person's visual acuity, color vision, and overall quality of life.
Early recognition and management are essential for controlling Bull's Eye Maculopathy and mitigating its impact on vision. Because changes in the retina are often irreversible, identifying the condition early may help in slowing its progression. Implementing prompt management strategies, including lifestyle modifications and pharmacological treatments as appropriate, can help preserve vision and improve the patient's quality of life. Therefore, frequent eye examinations and quick action upon noticing symptoms are vital components in dealing with Bull's Eye Maculopathy.
Causes of Bull's Eye Maculopathy
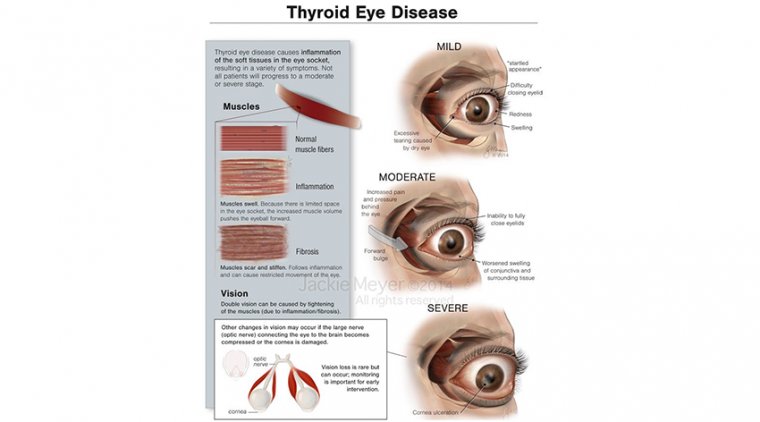
The etiology of Bull's Eye Maculopathy can be quite varied and may include both genetic and environmental factors. Some known causes include:
1. Drug toxicity: Certain medications can accumulate in the retina and cause cellular damage.
2. Genetic predispositions: Some individuals may have a hereditary predisposition to developing retinal issues.
3. Metabolic disorders: Conditions like Wilson's disease, where copper accumulates in various body tissues, can also lead to Bull's Eye Maculopathy.
4. Age-related changes: The risk of developing this condition may increase with age.
Hydroxychloroquine (Plaquenil) is one of the most common medications associated with Bull's Eye Maculopathy. Originally used for treating malaria, hydroxychloroquine is also prescribed for autoimmune diseases like lupus and rheumatoid arthritis. However, long-term use or high doses of this medication can lead to retinal toxicity and subsequent Bull's Eye Maculopathy.
The risk of maculopathy from hydroxychloroquine appears to be dose-dependent and also related to the duration of treatment. Patients taking this medication should undergo regular ophthalmic examinations, including retinal imaging and functional tests, to catch any early signs of toxicity. Once detected, discontinuation of the drug and a switch to an alternative medication—under medical supervision—can often prevent further retinal damage but may not reverse existing changes.
Symptoms and Signs of Bull's Eye Maculopathy
The symptoms of Bull's Eye Maculopathy can be subtle initially and may include:
● Blurred or distorted vision: Affected individuals may find it hard to read or recognize faces.
● Difficulty adapting to low light: A noticeable difficulty adjusting to darker environments.
● Central vision loss: As the condition primarily affects the macula, which is responsible for central vision, this can be an early sign.
● Color vision changes: Some patients may experience difficulty distinguishing between colors or notice colors appear less vibrant.
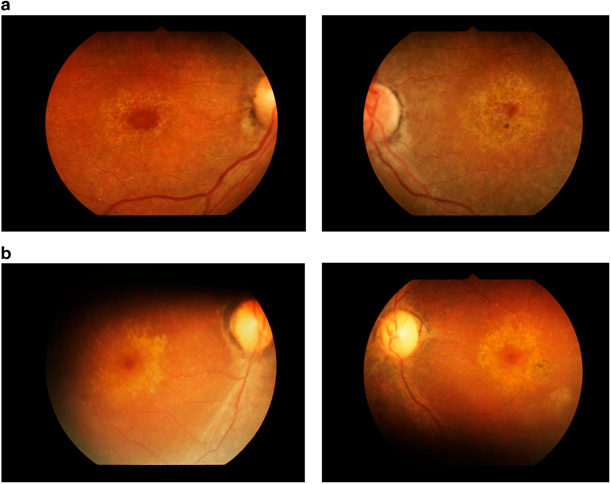
Early Symptoms vs. Advanced Stages
In the early stages of Bull's Eye Maculopathy, the symptoms are often mild and may be easily overlooked or attributed to aging or other minor vision problems. A person may not experience significant visual disturbances, but they may note subtle changes such as a slight difficulty in reading or slight distortion in central vision.
As the condition progresses to more advanced stages, the symptoms become more pronounced and debilitating:
● Central scotoma: A blind spot in the central field of vision.
● Severe loss of color vision: Colors may appear washed out or altered significantly.
● Profound loss of detail perception: Recognizing faces or reading becomes extremely difficult.
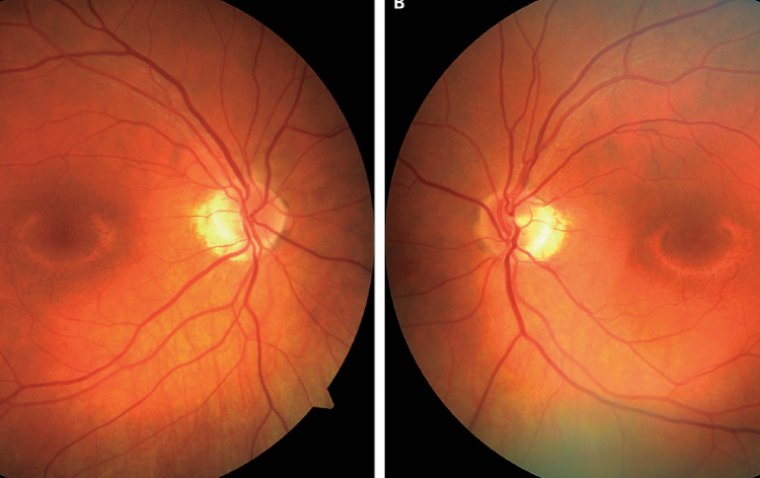
Credit: Research Gate
Diagnostic Methods for Bull’s Eye Maculopathy
The diagnosis of Bull's Eye Maculopathy typically involves a combination of clinical examination and specialized imaging tests. The process usually starts with a comprehensive eye examination where the ophthalmologist checks for any abnormalities in the eye, especially in the retina.
1. Optical Coherence Tomography (OCT)
Optical Coherence Tomography is a non-invasive imaging test that uses light waves to take cross-sectional pictures of the retina. It provides detailed images that can reveal the characteristic 'bull's eye' pattern of damage in the layers of the macula, thereby aiding in the diagnosis. OCT can also be valuable for monitoring disease progression over time.
2. Fundus Autofluorescence
Fundus autofluorescence is another non-invasive imaging technique used to evaluate retinal health. This method utilizes the natural fluorescence of certain retinal cells to create a detailed map of the retina. It can help in identifying areas where retinal cells are dying or have already died, confirming the presence of Bull's Eye Maculopathy.
3. Visual Field Testing
This helps to identify any dark or blind spots in your vision that you may not even be aware of, which can be indicative of macular issues.
4. Color Vision Testing
Since Bull's Eye Maculopathy can affect color vision, specialized tests may be conducted to assess this aspect.
5. Fluorescein Angiography
Although less commonly used, this diagnostic method involves injecting a fluorescent dye into the bloodstream and taking pictures of the retina to identify abnormal blood flow patterns or damage.
How Is Bull's Eye Maculopathy Treated?
The management of Bull's Eye Maculopathy largely depends on the underlying cause and the extent of retinal damage. Here are some of the main treatment options available:
Medical Interventions
1. Discontinuation or Dose Modification of Medications: If the condition is linked to the use of specific medications like hydroxychloroquine (Plaquenil), discontinuing or reducing the dose—under medical supervision—can sometimes slow or stop disease progression.
2. Nutritional Supplements: Some eye doctors recommend nutritional supplements that support eye health, such as lutein and zeaxanthin, although their effectiveness for this condition is not universally proven.
3. Antioxidants: Oral antioxidants like vitamin C and E have been suggested as potential treatments, but their effectiveness is still under investigation.
4. Off-label Therapies: Some medications used for other retinal diseases like age-related macular degeneration (AMD) may be considered on a case-by-case basis, but this is generally off-label use and should be approached with caution.
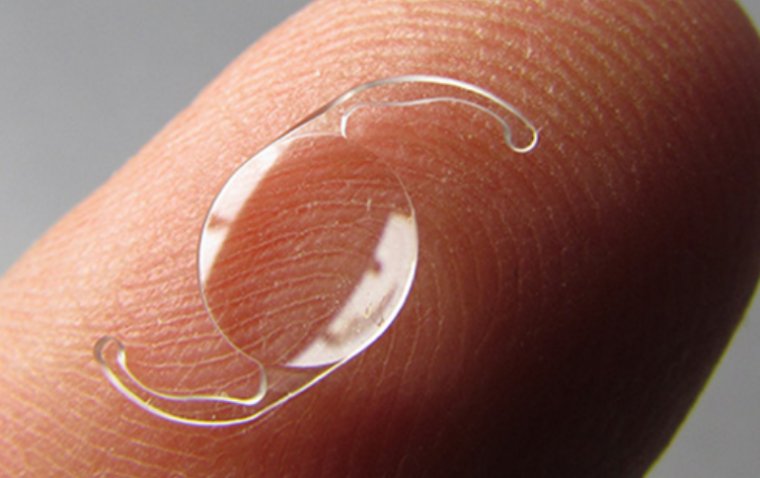
Potential Surgical Options
● Subretinal Surgery: While not commonly used for Bull's Eye Maculopathy, surgery to remove abnormal deposits or scar tissue from under the retina is an option in some cases.
● Retinal Implants: These are an emerging area of research and could become a future treatment modality.
● Stem Cell Therapy: This is an area of ongoing research and may offer future treatment possibilities.
Managing Medication-Induced Bull's Eye Maculopathy
Specific Guidance on Management
When Bull's Eye Maculopathy is suspected to be caused by medications like hydroxychloroquine (Plaquenil), specific interventions are required to minimize further damage and to manage the condition effectively.
1. Immediate Consultation: Consult your ophthalmologist as soon as you suspect or identify early signs of Bull's Eye Maculopathy. A full eye examination is essential to confirm the diagnosis.
2. Medication Review: If the medication is identified as the cause, your healthcare providers may collaborate to assess whether the medication can be discontinued or substituted with a less harmful alternative.
3. Dosage Adjustment: Sometimes, a lower dose of the medication might suffice for the treatment of the primary disease while minimizing the risk of eye toxicity. However, any changes in medication should only be made under strict medical supervision.
4. Frequent Monitoring: Patients who continue on the medication should undergo more frequent eye examinations and imaging tests like optical coherence tomography (OCT) to closely monitor the health of the retina.
Preventing Bull's Eye Maculopathy
● Informed Medication Use: Before starting medications known to cause Bull's Eye Maculopathy, such as hydroxychloroquine (Plaquenil), be well-informed about the associated risks and discuss alternatives with your healthcare provider if possible.
● Baseline Eye Examination: If you have to take such medications, a baseline ophthalmological examination is crucial for future comparisons. This is even more critical if you already have other risk factors for retinal diseases.
● Regular Monitoring: Adhere to the recommended eye examination schedule, which may include more frequent visits for high-risk patients. Monitoring is essential not just for those on medications but also for individuals who have other risk factors like age, family history, or other retinal conditions.
● Early Intervention: At the first sign of vision changes or discomfort, consult your eye care provider. The sooner you catch potential problems, the better your outcomes may be.
● Dose Management: Stick to prescribed doses of medication and never exceed the recommended dosage. High doses can increase the risk of developing Bull's Eye Maculopathy.
● Lifestyle Changes: Healthy living, including a balanced diet rich in antioxidants, might help support eye health, although it won't directly prevent Bull's Eye Maculopathy. However, general well-being can often contribute to better outcomes in various medical conditions, including eye health.
● Consult Multiple Specialists: If you're at higher risk due to medications, make sure your primary healthcare provider and ophthalmologist are in sync regarding your treatment plan.
Summary
Bull's Eye Maculopathy is a retinal disease that warrants immediate attention and ongoing management. It is often associated with the use of medications like hydroxychloroquine (Plaquenil) but can also occur due to other risk factors.
The condition usually presents with a specific pattern of retinal damage that can be detected through specialized imaging tests like optical coherence tomography (OCT). Early symptoms can be subtle and may differ significantly from those in the advanced stages, making regular eye examinations crucial.
Various treatment approaches are available, ranging from medical interventions to lifestyle changes and even surgical options in extreme cases. Managing medication-induced Bull's Eye Maculopathy involves a multidisciplinary approach, including rigorous medication monitoring.
(1).jpg)