Diagnosis and Testing for Salzmann's Nodular Degeneration
What Is Salzmann’s Nodular Degeneration?
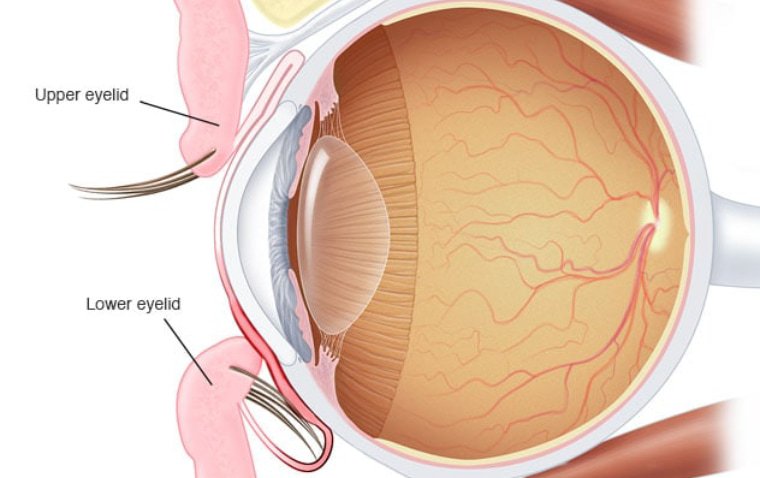
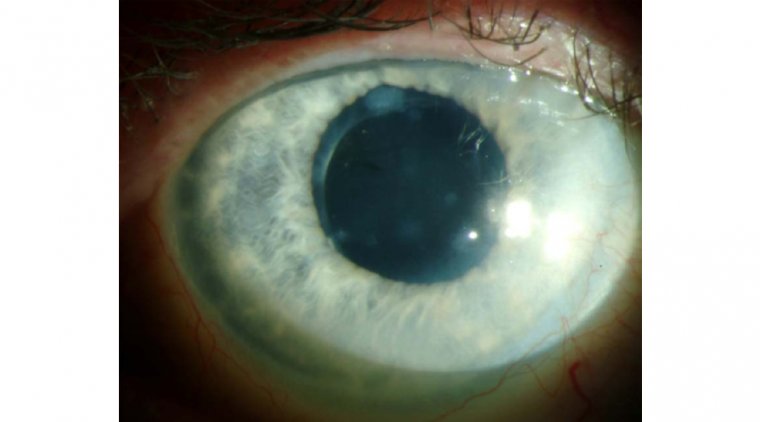
Salzmann Nodular degeneration is an asymmetric, noninflammatory and slowly progressive condition associated with the formation of fibrous outgrowths in any part of cornea. It is usually secondary to phlyctenular or trachomatous keratitis, it appears as 1-3 mm gray-white to bluish nodules beneath the cornea epithelium or anterior to Bowman's layer of the cornea. These raised nodules may be found in the mid-peripheral cornea or close to the limbus.
Causes of Salzmann’s Nodular Degeneration
Salzmann’s nodular degeneration is considered to be a disease of unknown etiology with no certainly known causes, however, there are a few conditions associated with risk of causing it:
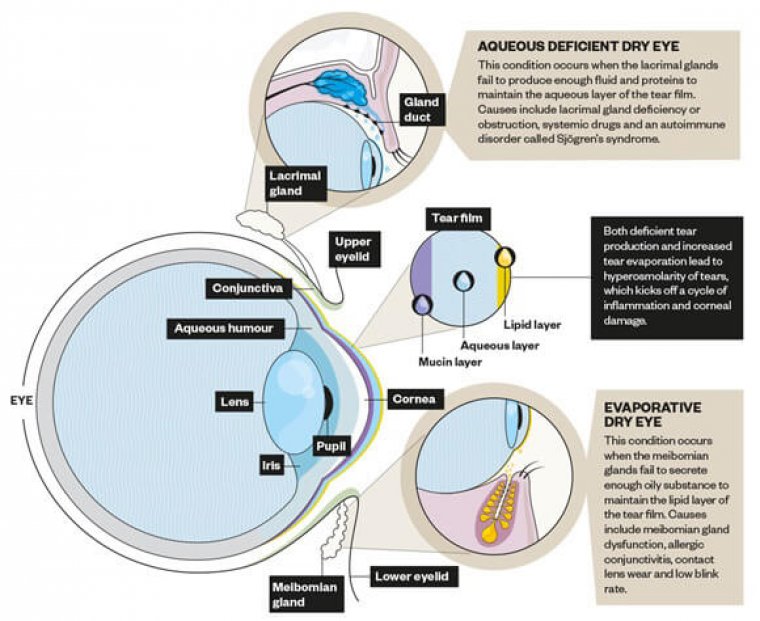
●Meibomian gland dysfunction (MGD)
●Contact lens wear (especially hard contact lenses)
●Keratoconjunctivitis sicca causing dry eyes
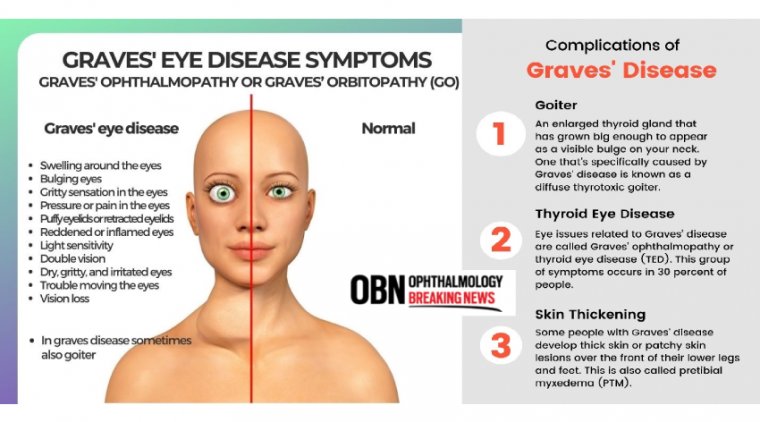
●Exposure keratitis
●Trauma to eyes
●Chronic inflammatory diseases of cornea (ocular surface)
●Peripheral vascularization and pterygium
Symptoms of Salzmann’s Nodular Degeneration
Generally, this condition affects more women than men. It is observed most commonly in later years of life like the late fifties. Symptoms appear on the basis of stages of the disease, earlier stages are subtle and asymptomatic, causing almost zero harm or trouble to the patient. Mild nodules located in the periphery or cornea are often asymptomatic. As the disease progresses it manifests as:
●Foreign body sensation due to the unequal wetting of the cornea in the nodular area
●Diminished and distorted vision
●Irregular astigmatism resulting in blurred vision.
●Frequent prescription changes
●Inability to have the best-corrected vision
●Multiple images or shadows of images
●Irritation, dryness, grittiness and rarely pain
Diagnosing Salzmann’s Nodular Degeneration
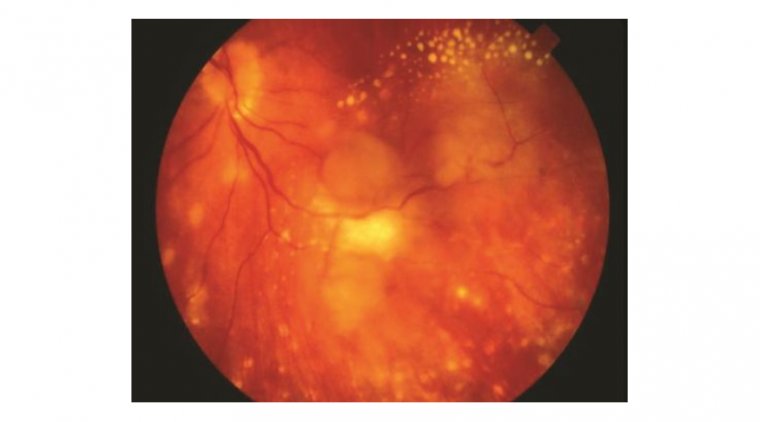
In its earliest of stages, Salzmann’s nodules are subtle and not very bothersome for the patient. In advanced stages for diagnostic purposes, several techniques are employed:
●The first step is usually a slit lamp examination of the eyes of the patient
●Ancillary testing includes corneal curvature
●Corneal topography and tomography
●Measurement of the corneal thickness (pachymetry).
●Anterior segment optical coherence tomography (AS-OCT)
Salzmann’s Nodular Degeneration Treatment
Salzmann Nodular degeneration does not have a definite treatment. It is either managed conservatively or surgically.
Conservative treatment
In conservative management of Salzmann’s nodular degeneration, treating the very cause of it will resolve the issue. As an example, in Meibomian Gland Disease, before surgical treatment of nodules, eyelid hygiene is maintained and doxycycline is given to treat MGD.). Other measures include;
●Proper ocular lubrication.
●Wearing glasses.
●Steroid eye drops as prescribed by the doctor
●Warm compresses
●Not using Contact lenses for quite some time, and re-fitting of contact lenses.
Surgical treatment
Popular and successful surgical excision of Salzmann Nodular degeneration options include: -
●Superficial keratectomy (SK)
●Phototherapeutic keratectomy (PTK)
●These surgical procedures are accompanied by the application of the anti-scarring agent called mitomycin C.
●Mitomycin-C will reduce the frequency and severity of recurrences after the excision of nodules.
●The most accurate way of preventing any future ocular erosions, causing Salzmann’s nodular degeneration, is to lubricate eyes every night for a minimum 3-6 months.
How to Prevent Salzmann's Nodular Degeneration
Since the exact cause of Salzmann's nodular degeneration is not fully understood, there are no specific preventive measures known. However, some general eye health practices and lifestyle habits may help maintain good eye health and reduce the risk of certain eye conditions:
1. Regular Eye Exams: Undergo routine comprehensive eye exams with an eye care professional. Regular eye exams can help detect any early signs of eye conditions and allow for timely intervention.
2. Avoid Eye Irritants: Protect your eyes from irritants such as smoke, dust, and harsh chemicals. Use protective eyewear when necessary, especially in work or outdoor environments with potential eye hazards.
3. Proper Contact Lens Care: If you wear contact lenses, follow the prescribed cleaning and wearing schedule provided by your eye care professional. Improper contact lens use can increase the risk of eye infections and complications.
4. Maintain a Healthy Diet: Eating a balanced diet rich in antioxidants and nutrients can promote overall eye health. Include foods like leafy greens, fish high in omega-3 fatty acids, citrus fruits, and carrots in your diet.
5. Practice Good Hygiene: Wash your hands regularly and avoid touching your eyes with unclean hands to reduce the risk of eye infections.
6. Manage Pre-existing Eye Conditions: If you have any pre-existing eye conditions, follow your eye care professional's recommendations for managing and treating them to reduce the risk of complications.
It's essential to consult with an eye care professional for personalized advice on maintaining your eye health and addressing any specific concerns. Additionally, please note that medical research and recommendations may evolve over time, so it's always best to stay informed with the latest information and guidelines from reputable sources.
(1).jpg)