Seeing Clearly Again: Vitrectomy Surgery for Floaters
Introduction to Floaters and Vitrectomy
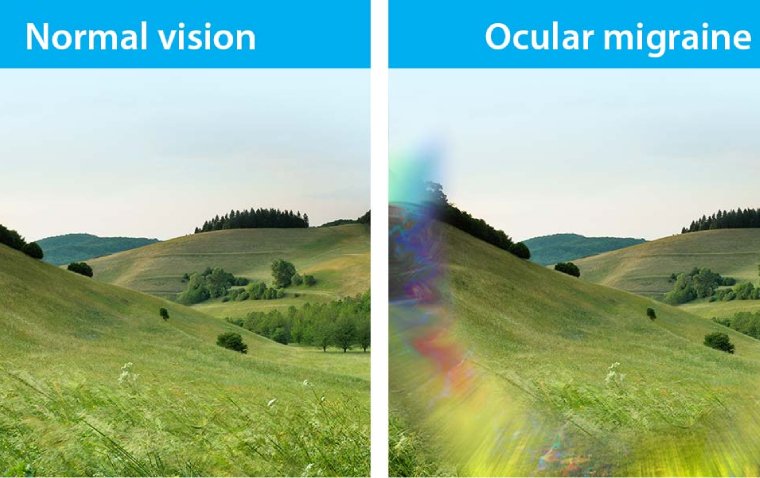
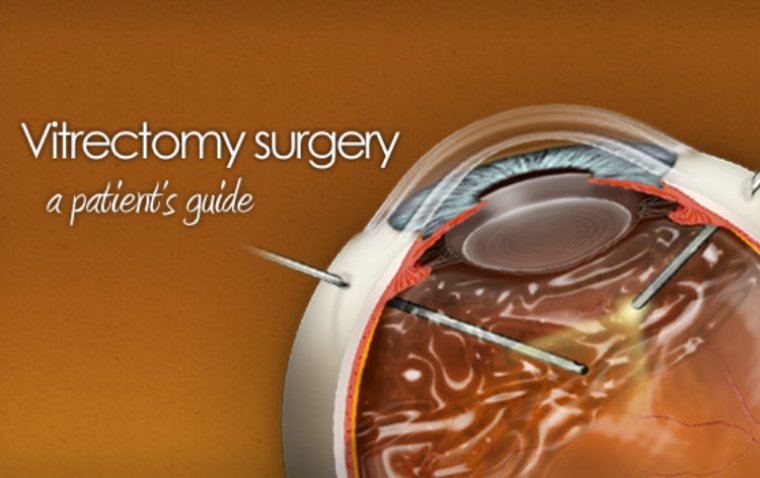
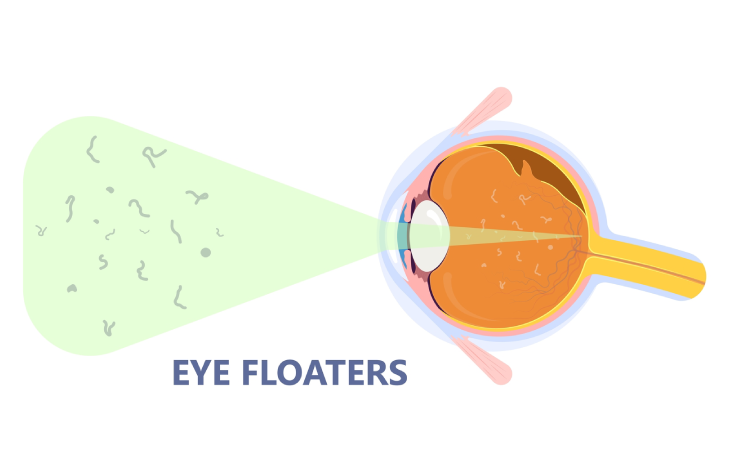
Eye floaters are small, shadowy shapes that drift across your field of vision. While typically benign, they can be bothersome and impact visual clarity. Floaters result from changes in the vitreous humor, the gel-like substance filling the eye's interior. For those significantly affected, a surgical intervention known as vitrectomy offers a solution. This procedure involves the removal of the vitreous humor, along with the floaters, to restore clear vision.
What is Vitrectomy for Floaters?
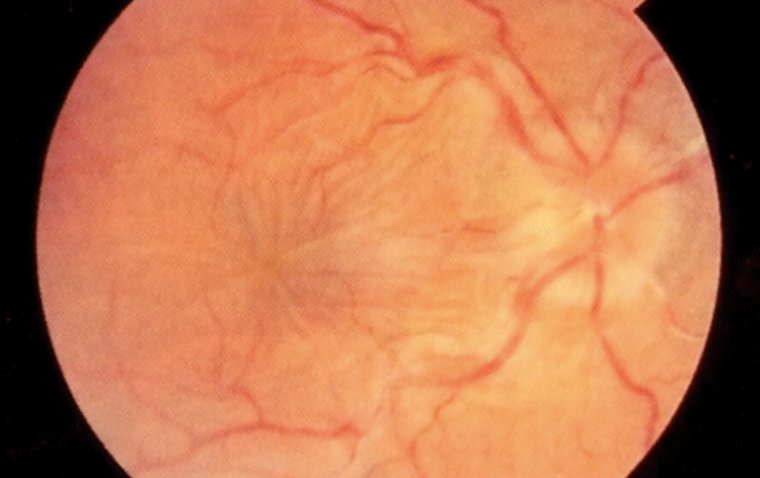
Vitrectomy is a surgical technique designed to address vision problems caused by eye floaters. The procedure is delicate, focusing on the vitreous humor, a clear, gel-like substance that helps maintain the eye's shape. Over time, this vitreous can liquefy, causing collagen fibers to clump together and cast shadows on the retina, perceived as floaters. Vitrectomy surgically removes this vitreous, thereby eliminating the bothersome floaters and improving vision quality.
What Can You Expect from the Vitrectomy Procedure?
The vitrectomy procedure, while intricate, is a well-established and effective treatment for floaters. The surgery begins with the administration of anesthesia, ensuring patient comfort and immobility during the procedure. The type of anesthesia used may vary, ranging from local to general, depending on the patient's specific case and overall health.
Once the anesthesia takes effect, the ophthalmic surgeon makes precise, tiny incisions in the sclera, the eye's white outer layer. These incisions are strategically placed to allow access to the vitreous humor without damaging surrounding tissues. Specialized microsurgical instruments, such as a vitrector, are then inserted through these incisions. The vitrector delicately cuts and suctions out the vitreous humor along with the floaters. This process is meticulously performed to ensure complete removal of the floaters while maintaining the integrity of the retina and other vital eye structures.
During the removal of the vitreous, the surgeon may replace it with a saline solution, a gas bubble, or a silicone oil, depending on the specific needs of the patient. This replacement helps maintain the eye's shape and support the retina post-surgery.
After the vitrectomy, the incisions are closed with tiny stitches or may be left to self-seal, depending on the size and nature of the incisions. The surgeon then applies a sterile dressing and an eye shield to protect the eye as it begins the healing process.
The procedure is typically performed on an outpatient basis, meaning most patients can return home the same day. The duration of the surgery varies but generally takes around one to two hours. It is crucial for patients to have a responsible adult accompany them after the surgery, as the effects of anesthesia may temporarily impair their ability to drive or operate machinery.
Potential Risks and Complications
● Infection: One of the most common risks associated with any surgery, including vitrectomy, is the possibility of infection. Despite the sterile environment and precautionary measures, there's always a slight chance that bacteria can enter the eye, leading to infections which may require additional treatment.
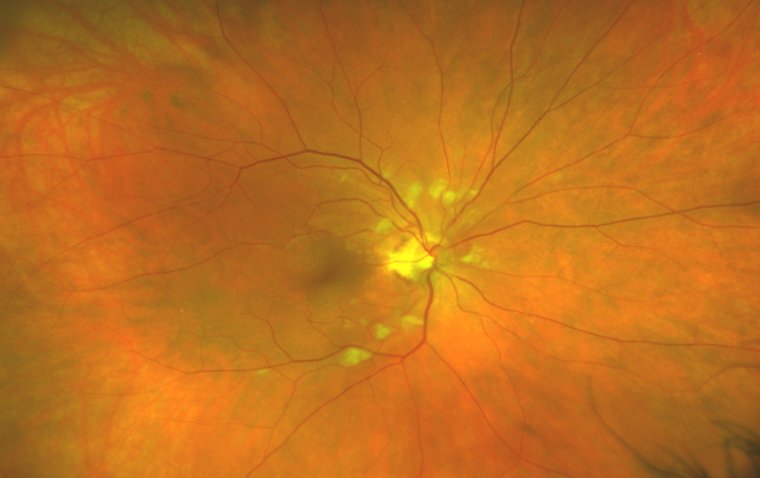
● Retinal Tears or Detachment: The procedure involves manipulation near the retina, which can sometimes lead to tears or even detachment. This serious complication might require further surgical intervention to repair the retina.
● Development of Cataracts: Patients undergoing vitrectomy, especially those who are older, have an increased risk of cataract development. The surgery can accelerate the natural process of cataract formation, potentially leading to the need for cataract surgery in the future.
● Changes in Eye Pressure: Fluctuations in intraocular pressure (IOP) can occur after vitrectomy. Both increased and decreased IOP can pose risks to the health of the eye and vision, requiring careful monitoring and management.
● Bleeding Inside the Eye: There is a risk of bleeding during or after the surgery, which can affect vision. This bleeding usually resolves on its own but in rare cases, might need additional treatment.
● Swelling or Edema: Post-operative swelling or edema, especially in the cornea or retina, can temporarily impair vision. While most cases of swelling resolve with time, some may need medical intervention.
● Anesthesia Complications: Although rare, there are risks associated with anesthesia, including allergic reactions or other anesthesia-related complications.
● Vision Changes or Loss: In rare cases, patients may experience changes in their vision, including a decrease in visual acuity. In very rare instances, there can be a significant loss of vision.
● Delayed Healing: Some patients may experience delayed healing or prolonged discomfort after the surgery, which can impact their daily activities and quality of life.
Recovery and Post-Operative Care
Post-vitrectomy recovery is critical for optimal results. Patients may experience mild discomfort, temporary vision changes, or sensitivity to light. Follow-up appointments are essential to monitor healing and eye pressure.
1. Initial 24-48 Hours Post-Surgery: During this period, it's normal for patients to experience mild to moderate discomfort. The eye may feel itchy or sore, and this can be managed with prescribed pain relievers. Rest is crucial, and patients should avoid any activities that strain the eyes, such as reading or watching TV for prolonged periods.
2. Managing Sensitivity to Light: Increased sensitivity to light is common after vitrectomy. Wearing sunglasses when outdoors or in brightly lit areas can help ease discomfort.
3. Use of Eye Drops: Patients will be prescribed eye drops to prevent infection, reduce inflammation, and help in the healing process. It's essential to use these drops exactly as directed by the surgeon.
4. Activity Restrictions: For a specified period, usually a few weeks, patients should avoid strenuous activities, heavy lifting, and bending over, as these actions can increase eye pressure and hinder the healing process.
5. Sleeping Position: Depending on the specific details of the surgery, the surgeon might recommend sleeping in a certain position, such as on your back or with your head elevated, to facilitate proper healing.
6. Avoiding Water in the Eye: It's important to keep the operated eye protected from water to prevent infection. This means avoiding swimming and being cautious while showering or washing the face for a certain period post-surgery.
7. Monitoring for Complications: Patients should be vigilant for signs of complications, such as increased pain, redness, swelling, or a sudden decrease in vision, and should contact their ophthalmologist immediately if these occur.
8. Follow-up Appointments: Regular follow-up appointments are crucial to monitor the healing process, check for any complications, and adjust treatment as needed. These appointments provide an opportunity for patients to discuss any concerns or questions they have about their recovery.
9. Gradual Return to Normal Activities: Patients can usually start returning to their normal daily activities, including work, as advised by their surgeon, typically within a few weeks post-surgery. However, the exact timeline varies based on individual recovery and the nature of their work.
10. Patient Education: Understanding the healing process and having realistic expectations about recovery timelines and outcomes is important for patient satisfaction and adherence to post-operative care instructions.
Summary
Vitrectomy for floaters is a specialized surgical procedure offering relief for those significantly impacted by these visual disturbances. While it comes with potential risks, the procedure generally results in improved visual clarity. As with any medical intervention, a thorough discussion with a qualified ophthalmologist is essential to weigh the benefits against the risks. With proper care and adherence to post-operative guidelines, patients can expect a gradual return to clearer, more comfortable vision.
(1).jpg)