Persistent Pupillary Membrane: How Does it Affect Vision?
What is Persistent Pupillary Membrane?
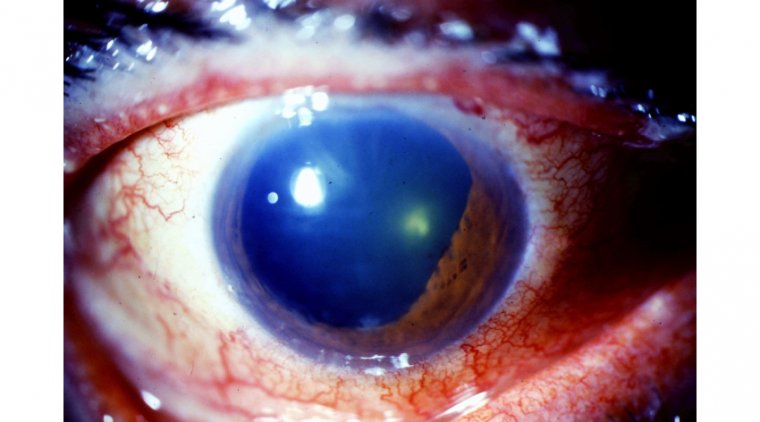
Persistent Pupillary Membrane (PPM) is a congenital eye condition that occurs when remnants of a fetal membrane persist in the eye beyond the usual developmental stage. During fetal development, the pupillary membrane is a normal structure that supplies blood to the lens of the eye. It typically dissolves and disappears as part of the normal growth process before or shortly after birth. However, in cases of PPM, remnants of this membrane remain attached to various parts of the eye, primarily the lens or iris.
The condition is relatively common and is often diagnosed in early infancy or childhood during routine eye examinations. In most instances, PPM is a benign condition that may not significantly impact vision. However, the extent to which vision is affected depends on the density and location of the membrane remnants. In rare cases, if the membrane is particularly dense or located in a way that obstructs the pupil, it can impair vision.
Classification of Persistent Pupillary Membrane
Persistent Pupillary Membrane (PPM) can be classified into three main types, each characterized by distinct features and locations of the membrane remnants. Understanding these types is essential for diagnosing and managing this congenital eye condition effectively.
1. Type 1 PPM:
Type 1 PPM is the most common and mildest form of this condition. In Type 1 PPM, fine strands or threads of the fetal pupillary membrane persist. These strands typically extend from the iris, across the pupil, and attach to the lens capsule. While these strands are usually delicate and translucent, they may not significantly affect vision. In many cases, Type 1 PPM is an incidental finding during routine eye examinations and doesn't require treatment.
2. Type 2 PPM:
Type 2 PPM is characterized by denser and more substantial membrane remnants compared to Type 1. In this type, the remnants can vary in thickness and can be seen extending from the iris to other parts of the eye, including the cornea, lens, or anterior chamber. Type 2 PPM can potentially cause more visual disturbances than Type 1 due to the greater coverage and thickness of the membrane. Depending on the location and density of the membrane, treatment may be considered to improve visual function.
3. Type 3 PPM:
Type 3 PPM is the least common and most severe form of this condition. It is distinguished by thick and opaque membrane remnants that extensively cover the anterior segment of the eye, including the iris, cornea, and lens. This type can lead to significant visual impairment and discomfort for the affected individual. Type 3 PPM often requires surgical intervention to remove the membrane and improve visual function.
.jpg)
What Causes Persistent Pupillary Membrane in the Eye?
Persistent Pupillary Membrane (PPM) is a congenital eye condition, which means it is present at birth and is primarily caused by developmental factors during fetal growth. Several factors contribute to the development of PPM:
● Incomplete Fetal Membrane Regression: During fetal development, the eye undergoes numerous complex changes to form its various structures. One of these structures is the pupillary membrane, which supplies blood to the developing lens. Normally, this membrane should start regressing and dissolving as the fetus grows. However, in cases of PPM, this regression process is incomplete, leading to the persistence of portions of the membrane.
● Genetic Factors: Genetic factors can play a role in the development of PPM. Some individuals may have a genetic predisposition that increases the likelihood of PPM. It is not uncommon for multiple family members to have a history of PPM, suggesting a hereditary component.
● Intrauterine Environmental Factors: Certain intrauterine environmental factors can contribute to the development of PPM. These factors may include exposure to toxins, infections, or other disruptions during pregnancy. They can interfere with the normal developmental processes of the eye, potentially increasing the risk of PPM.
● Abnormal Iris Development: The iris, which is the colored part of the eye, plays a significant role in the development of PPM. If there are abnormalities in the development of the iris, it can lead to the attachment of the pupillary membrane remnants to the iris itself, making it more likely for PPM to persist.
● Premature Birth: Premature infants have a higher risk of PPM. This increased risk is partly due to the fact that the pupillary membrane normally starts to regress later in gestation, so premature infants may have a higher chance of it persisting.
● Other Congenital Eye Conditions: PPM can sometimes co-occur with other congenital eye conditions. For example, it may be found in individuals with conditions like microphthalmia (abnormally small eyes) or coloboma (a gap or hole in eye structures). The presence of these conditions can further complicate the developmental processes of the eye.
Signs and Symptoms of Persistent Pupillary Membrane
Persistent Pupillary Membrane (PPM) may present with various signs and symptoms, which can vary in severity depending on the type and extent of the membrane remnants. Here are the observable signs and symptoms associated with PPM:
1. Abnormal Pupil Shape:
● One of the most common signs of PPM is an irregular or abnormal pupil shape. Instead of having a round or circular pupil, individuals with PPM may have a pupil that appears irregularly shaped due to the presence of membrane strands crossing the pupil. These strands can create notches or irregular borders.
2. Light Sensitivity (Photophobia):
● Many individuals with PPM experience increased sensitivity to light, a condition known as photophobia. The abnormal pupillary membrane remnants can cause scattered light to enter the eye, making it challenging to tolerate bright light conditions. Photophobia can lead to discomfort and squinting in bright environments.
3. Blurry Vision:
● Blurred vision is another common symptom of PPM, especially in cases where the membrane remnants are denser or cover a larger portion of the pupil. The presence of the membrane can disrupt the normal passage of light through the pupil, resulting in blurred or distorted vision.
4. Visual Disturbances:
● Depending on the location and density of the membrane remnants, individuals with PPM may experience visual disturbances such as halos, glare, or double vision. These disturbances can interfere with daily activities and reduce visual clarity.
5. Reduced Visual Acuity:
● In severe cases of PPM, where the membrane covers a significant portion of the pupil or interferes with the lens, individuals may have reduced visual acuity. This means that their ability to see fine details and objects at a distance may be compromised.
6. Strabismus (Crossed Eyes):
● PPM can sometimes be associated with strabismus, a condition in which the eyes do not align properly. Strabismus can lead to double vision and may require additional treatment beyond addressing the PPM.
Does Persistent Pupillary Membrane Affect Vision?
Persistent Pupillary Membrane (PPM) can indeed affect vision, and the extent of its impact depends on several factors, including the type and density of the membrane remnants. In cases of PPM where the membrane remnants are minimal and translucent (Type 1 PPM), the impact on visual acuity is often negligible. These fine strands may not significantly obstruct the pupil or distort the passage of light through the eye, allowing for relatively normal visual development. However, in more severe cases, such as Type 2 and Type 3 PPM, where the membrane remnants are denser and cover a larger portion of the pupil or other eye structures, there can be a notable impact on visual acuity. The interference with the normal passage of light through the eye can result in blurred vision and reduced visual clarity.
PPM, particularly when it involves thick and opaque membrane remnants, can lead to increased sensitivity to light (photophobia). The irregularly shaped pupil and scattered light entering the eye can make it challenging for individuals to tolerate bright light conditions, affecting their daily activities and quality of life. Visual disturbances, such as halos, glare, or double vision, can also occur, especially in cases of Type 2 and Type 3 PPM due to the greater interference with the visual pathway. These disturbances can be problematic for tasks that require clear vision, such as reading or driving.
How to Diagnose Persistent Pupillary Membrane
The diagnosis of Persistent Pupillary Membrane (PPM) typically involves a comprehensive eye examination and may include specialized imaging techniques. Ophthalmologists play a crucial role in confirming the presence and type of PPM. Here is an outline of the diagnostic process for PPM:
1. Medical History and Symptoms Assessment:
● The diagnostic process often begins with a thorough review of the patient's medical history and a discussion of any visual symptoms or discomfort they may be experiencing. Patients may report symptoms such as blurred vision, photophobia (light sensitivity), or visual disturbances.
2. Visual Acuity Testing:
● Visual acuity testing is conducted to assess the patient's ability to see fine details at various distances. This test is typically performed using an eye chart to measure the sharpness of vision.
3. Slit-Lamp Examination:
● A slit-lamp examination is a specialized microscope with a bright, narrow beam of light that allows the ophthalmologist to examine the structures of the eye in detail. During this examination, the ophthalmologist can visualize the pupillary area to look for any abnormalities, including the presence of membrane remnants.
4. Pupil Dilation:
● To obtain a more comprehensive view of the pupil and its surrounding structures, the ophthalmologist may use dilating eye drops to enlarge the pupil. This allows for a better assessment of any membrane remnants that may be present.
5. Imaging Techniques:
● In some cases, imaging techniques such as ultrasound or anterior segment optical coherence tomography (AS-OCT) may be used. Ultrasound can help visualize the interior of the eye and the location of the membrane remnants. AS-OCT provides detailed cross-sectional images of the anterior segment of the eye, aiding in the assessment of PPM's type and extent.
6. Confirmation by Ophthalmologist:
● The final confirmation of PPM and its classification (Type 1, Type 2, or Type 3) is typically made by the ophthalmologist based on the findings from the various examinations and imaging techniques. The ophthalmologist will assess the location, density, and impact of the membrane remnants on visual function.
7. Treatment Considerations:
● Depending on the diagnosis, the ophthalmologist will discuss treatment options, if necessary. In many cases of Type 1 PPM, no treatment may be required, and the condition can be monitored. Type 2 and Type 3 PPM, which can have a more significant impact on vision, may require surgical intervention to remove the membrane remnants and improve visual function.
8. Follow-Up Examinations:
● For individuals diagnosed with PPM, especially children, regular follow-up examinations are essential to monitor the condition's progression and ensure optimal visual development. These follow-up visits allow for timely intervention if needed.
Can Persistent Pupillary Membrane Be Treated?
Persistent Pupillary Membrane (PPM) can be treated, and the approach to treatment depends on the type and severity of the condition, as well as its impact on visual function. Here are the available treatment options for PPM:
1. Observation and Monitoring (Type 1 PPM):
● In cases of Type 1 PPM, which often involve fine and translucent membrane strands that do not significantly obstruct vision, treatment may not be necessary. Instead, the ophthalmologist may recommend regular eye examinations to monitor the condition's progression, especially in pediatric patients. Many individuals with Type 1 PPM do not experience significant visual disturbances and can lead a normal life without treatment.
2. Surgical Intervention (Type 2 and Type 3 PPM):
● Type 2 and Type 3 PPM, which involve denser and more substantial membrane remnants, may require surgical intervention, especially if they lead to visual disturbances or discomfort. Surgical removal of the membrane is typically considered to improve visual outcomes.
Surgical Techniques:
● There are various surgical techniques that ophthalmologists may employ to address Type 2 and Type 3 PPM:
● YAG Laser Membranotomy: This non-invasive procedure uses a laser to create an opening in the membrane, allowing it to separate from the iris or other structures. It is a relatively quick and effective method.
● Surgical Membrane Removal: In cases where the membrane is dense and extensive, surgical removal may be performed. This involves making small incisions in the eye to access and remove the membrane remnants.
● Iridotomy or Iridectomy: These procedures involve creating an opening in the iris to relieve any blockage caused by the membrane. They are particularly useful when the membrane is attached to the iris.
3. Strabismus Management:
● PPM can be associated with strabismus (crossed eyes), which can further affect vision. Strabismus may require treatment by an ophthalmologist, which can include corrective lenses, eye exercises, or surgical correction to align the eyes properly.
4. Management of Associated Symptoms:
● Photophobia (light sensitivity) and discomfort are common symptoms associated with PPM. These symptoms can often be managed with tinted or photochromic lenses to reduce sensitivity to bright light. Lubricating eye drops can also help alleviate discomfort caused by membrane contact with other eye structures.
Summary
Persistent Pupillary Membrane (PPM) is a congenital eye condition characterized by remnants of a fetal membrane that persist in the eye. It can impact vision and is classified into three types: Type 1, Type 2, and Type 3, with varying severity. The causes of PPM include incomplete fetal membrane regression, genetic factors, and intrauterine environmental factors.
Signs and symptoms of PPM include abnormal pupil shape, light sensitivity (photophobia), blurry vision, visual disturbances, reduced visual acuity, and potential complications like strabismus. The condition's impact on vision varies with its type and density, with Type 2 and Type 3 PPM having a more significant effect.
Diagnosing PPM involves a comprehensive eye examination, including visual acuity testing, slit-lamp examination, pupil dilation, and, if necessary, imaging techniques. Ophthalmologists play a crucial role in confirming the diagnosis and assessing the condition's severity.
Treatment options for PPM depend on the type and severity. Type 1 PPM may not require treatment but should be monitored. Surgical intervention, such as YAG laser membranotomy or surgical membrane removal, is considered for Type 2 and Type 3 PPM. Strabismus management and symptom alleviation with lenses and eye drops are also essential.
In conclusion, PPM is a congenital condition with three classification types, varying causes, and a range of signs and symptoms that can impact vision. Timely diagnosis and professional advice from ophthalmologists are crucial for appropriate management. Early intervention and tailored treatment plans can help optimize visual outcomes for individuals with PPM.
(1).jpg)