What Is Pseudophakia?
Pseudophakia, is a Latin word, made up of two parts pseudo (fake or artificial) and phakia(lens). It is an incredible visual rehabilitation technique, where an artificial İntraocular lens is introduced into the affected eye after the extraction of a cloudy natural lens restoring vision to normal swiftly.
What are the signs that you need IOLs?
Intraocular lenses are essential when a patient experiences blurred vision, difficulty in dim light, diplopia and focusing on a distant or near object, faded colors, seeing hues of purple or blue color, uncontrolled vulnerability to glare from sunlight or headlight of vehicles, repeated changes in spectacles or contact lens prescription, need of a brighter light for near work and halos.
What to expect with IOL implantation?
IOLs after their insertion become a perpetual part of your eye. So, an eye exam will be conducted on you by an ophthalmologist, consisting of;
● Visual Acuity test to check your vision.
● A slit lamp examination to observe your iris, anterior chamber, and lens.
● A retinal exam.
● A biometry to determine the correct power of your pseudophakia lens for you.
Before your surgery, your doctor will question you about your past medical history such as diabetes, hypertension, and the use of any blood thinners, or alpha agonists like tamsulosin. Post-surgery your eye will be bandaged temporarily. You are allowed to leave the hospital after half an hour but not drive for the time being.
What are the types of pseudophakic IOLs?
Multiple types of rigid or foldable IOLs are available made from plastic, acrylic, or silicone. Your pseudophakic IOL will depend on your prescription, lifestyle, and the cost of IOL. IOLS can be placed in the anterior (between the iris and cornea) or posterior chamber (usual place of natural lens) of the eye. The most commonly used IOLs are Standard monofocal IOLs, used for correction of far vision only, some patients might need near vision spectacles afterward. Unique Toric IOLs come in handy for patients with cataracts with astigmatism.
Multifocal IOLs consist of several rings, and each ring has a different power for near, intermediate, and far vision respectively, human brains learn these rings quickly and transition between them seamlessly. Accommodative IOLs are nearest to the natural lens. These are responsive to eye muscle movements and move forwards or backward for near and distant objects respectively. Both of these reduce the need for near-vision spectacles.
Steps of IOL Implantation Procedure
This surgery is an OPD procedure of approximately 15-30 minutes. The patient is given a sedative to relieve anxiety, an anti-biotic drop, pupil dilating drops, and a local anesthetic to numb the respective eye, however, the patient is conscious during the surgery.
The operation field is sterilized with iodine. Three basic techniques could be implied namely phacoemulsification (with ultrasound waves breaking the lens), laser or extracapsular cataract extraction (the lens is removed as a whole through a large cut). The basic steps for all three are quite similar.
● Using a blade or laser a small cut is made in the clear cornea.
● A probe is introduced through the cut and the cataractous lens is broken into smaller pieces using ultrasound waves (phacoemulsification) or laser.
● A suction device is used to remove all the tiny pieces of the lens.
● The new artificial lens is placed in the anterior or posterior chamber.
● The incision is sealed.
● Eye patch is placed to guard the eye and aid in its recovery.
Complications
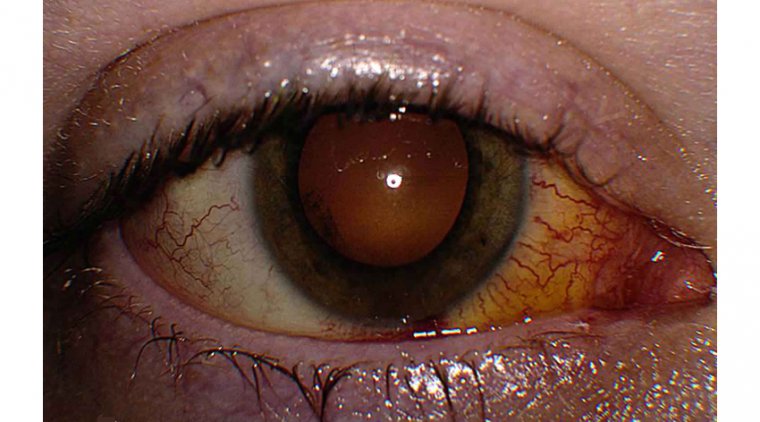
Immediately after surgery, there could be infection, extreme pain, bleeding, redness and discharge from the eyes, vision loss, fever, diplopia, increased eye pressure, and seeing the edge of the lens. Other complications include: -
● Overcorrection or under-correction of vision
● Faulty placement of the lens
● Subluxation of lens leading to blurred vision
● Angle closure in anterior chamber lens implant
● Change in shape of the pupil
● Accumulation or swelling in retina Irvine-Gass syndrome
● Retinal detachment
(1).jpg)