Sickle Cell Retinopathy: Understanding the Condition
When it comes to sickle cell disease, the complications can be as multifaceted as the condition itself, with sickle cell retinopathy taking center stage in the realm of vision-related issues. This eye-opening complication targets the retina, potentially clouding the world of those affected.
In this article, we'll shine a light on sickle cell retinopathy, delving deep into its causes, symptoms, and progression. Furthermore, we'll explore methods of diagnosis and the various management strategies available to help patients maintain their visual clarity in the face of this challenging condition.
What is Sickle Cell Retinopathy?
Sickle cell retinopathy is a vision-threatening complication that arises from sickle cell disease, a genetic disorder that affects red blood cells. In individuals with sickle cell disease, the red blood cells become abnormally shaped, resembling a crescent or sickle. These misshapen cells can obstruct blood vessels, leading to a variety of complications, including those that impact the retina – the light-sensitive tissue at the back of the eye.
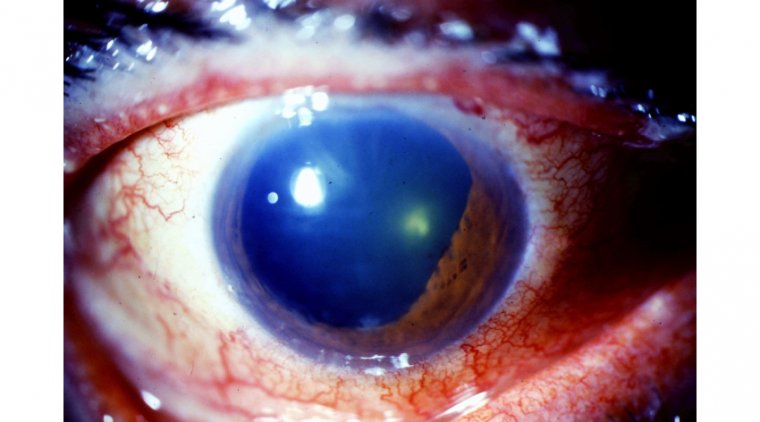
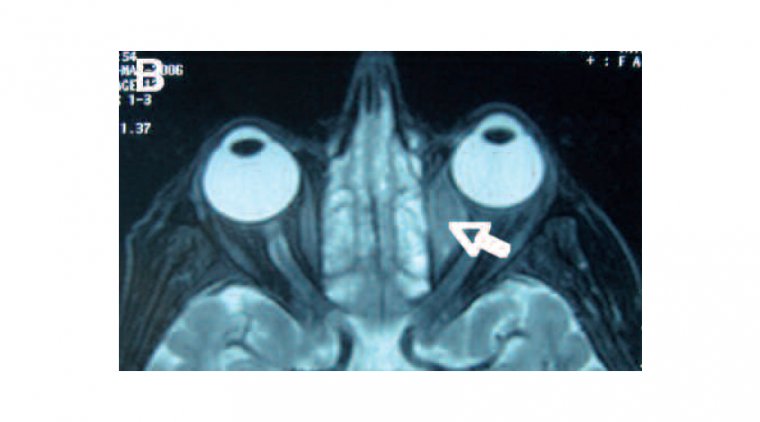
Sickle cell retinopathy occurs when the blood vessels supplying the retina become blocked, leading to insufficient oxygen delivery and subsequent damage to the retinal tissue. Over time, this damage can impair vision and, in severe cases, even result in blindness. Sickle cell retinopathy is a progressive condition that can manifest in various stages, ranging from mild retinal changes to more severe complications such as retinal detachment.
What are the Different Types of Cickle Cell Retinopathy?
Sickle cell retinopathy can present in various forms and severity levels. The Goldberg classification system is widely used to categorize the condition into five distinct stages, each reflecting the progression and severity of the disease:
- Stage 1 - Peripheral arteriolar occlusions: This initial stage is characterized by the blockage of small blood vessels (arterioles) in the peripheral retina. The occlusions may be difficult to detect and typically cause no symptoms.
- Stage 2 - Peripheral arteriovenous anastomoses: As the disease progresses, new blood vessels begin to form in response to the blocked arterioles. These new vessels create abnormal connections between arteries and veins (anastomoses) in the peripheral retina.
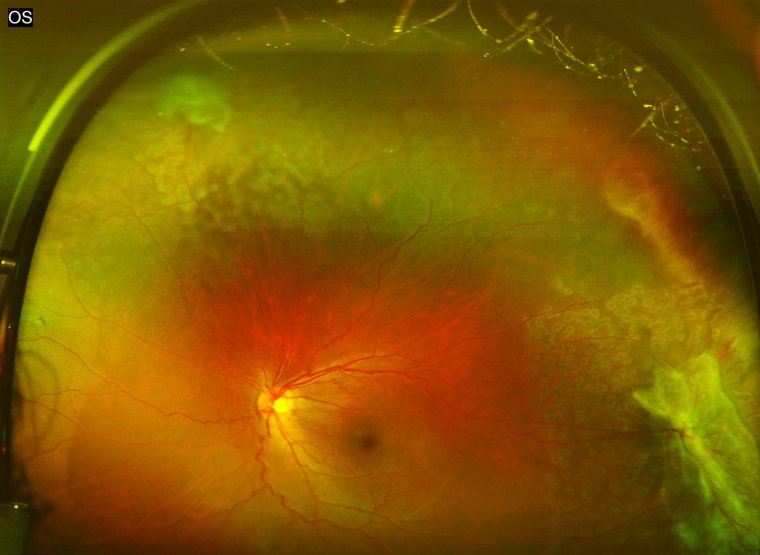
- Stage 3 - Neovascular proliferation: During this stage, the abnormal blood vessels proliferate and form a network known as "sea fan" neovascularization. These fragile vessels are prone to leakage and bleeding, which can lead to vision problems.
- Stage 4 - Vitreous hemorrhage: The fragile new blood vessels can rupture and bleed into the vitreous humor, the clear gel-like substance that fills the space between the lens and the retina. A vitreous hemorrhage can cause sudden vision loss or floaters (small spots or cobweb-like shapes) in the visual field.
- Stage 5 - Retinal detachment: The most severe stage, retinal detachment occurs when scar tissue from the bleeding and neovascularization pulls the retina away from its normal position. This detachment can lead to severe vision loss or even blindness if not treated promptly.
What are the Causes and Risk Factors of Sickle Cell Retinopathy?
In individuals with sickle cell disease, abnormal hemoglobin causes red blood cells to become misshapen, resembling a crescent or sickle shape. These deformed cells can obstruct blood flow, leading to various complications, including sickle cell retinopathy.
The risk factors for developing sickle cell retinopathy are mainly related to the type of sickle cell disease and the severity of the condition. Some factors that may influence the development and progression of sickle cell retinopathy include:
- Sickle cell genotype: Patients with certain genotypes, such as HbSS (homozygous sickle cell anemia) and HbSC (heterozygous sickle cell-hemoglobin C disease), are at a higher risk of developing retinopathy compared to those with other genotypes.
- Age: Sickle cell retinopathy tends to be more common and severe in adults, as the risk increases with age. However, children with sickle cell disease can also develop retinopathy.
- Disease severity: Patients with more severe sickle cell disease manifestations are at a higher risk of developing retinopathy.
- Hypoxia: Reduced oxygen levels in the blood (hypoxia) can contribute to retinopathy development by causing ischemia (inadequate blood supply) in the retina.
- Other risk factors: Certain factors, such as high blood pressure, anemia, or a history of retinal complications, may increase the likelihood of sickle cell retinopathy.
What are the Symptoms of Sickle Cell Retinopathy?
Sickle cell retinopathy can manifest in various ways, and the symptoms may range from mild to severe. In some cases, individuals may not experience any noticeable symptoms, especially in the early stages of the condition. However, as sickle cell retinopathy progresses, the following symptoms may arise:
- Floaters: Patients may see small, dark specks or spots drifting in their field of vision. These floaters are caused by the accumulation of blood cells or vitreous debris within the eye.
- Blurred vision: A reduction in visual acuity or clarity can occur as a result of retinal damage or swelling.
- Visual field loss: Some patients may experience a loss of peripheral vision or "tunnel vision" due to damage in the peripheral retina.
- Flashes of light: Patients might see sudden flashes of light, typically in their peripheral vision, which can be an indication of retinal traction or detachment.
- Sudden vision loss: In severe cases, individuals may experience sudden, painless vision loss due to complications such as vitreous hemorrhage or retinal detachment.
Treatment Options for Sickle Cell Retinopathy
Although there is no cure for sickle cell retinopathy, various treatment options are available to manage the condition, alleviate symptoms, and prevent further vision loss. The choice of treatment depends on the severity and type of retinopathy, as well as the patient's overall health. Some of the most common treatment options include:
- Observation and monitoring: In cases of mild retinopathy with no significant impact on vision, doctors may opt for regular monitoring through comprehensive eye examinations to track the progression of the condition.
- Laser photocoagulation: This procedure involves using a laser to create small burns in the peripheral retina, which helps seal off leaking blood vessels and reduce retinal swelling. Laser photocoagulation can help prevent the progression of proliferative sickle cell retinopathy and reduce the risk of vision loss.
- Intravitreal injections: Medications, such as anti-vascular endothelial growth factor (anti-VEGF) agents, can be injected directly into the vitreous cavity of the eye to inhibit the growth of abnormal blood vessels and decrease retinal swelling.
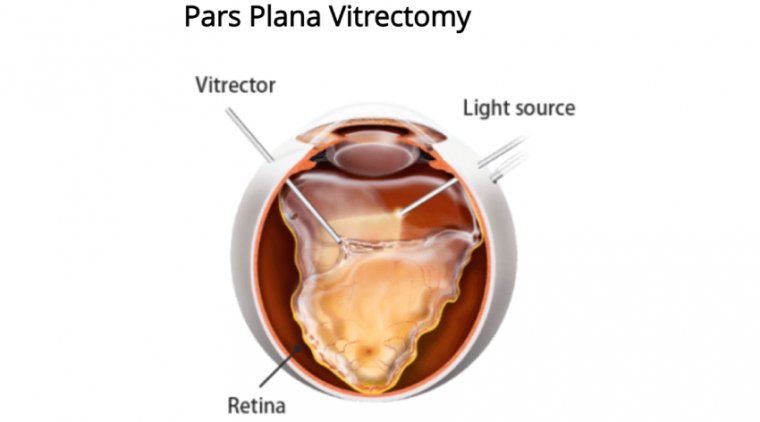
- Vitrectomy: In cases of advanced retinopathy with complications such as vitreous hemorrhage or retinal detachment, a vitrectomy may be necessary. This surgical procedure involves removing the vitreous gel from the eye and replacing it with a saline solution, allowing the surgeon to repair any retinal damage.
- Managing underlying sickle cell disease: Addressing the root cause of sickle cell retinopathy is essential to prevent further complications. Patients should work closely with their healthcare team to manage their sickle cell disease through medications, blood transfusions, or other treatments as advised.
What are the Benefits and Risks of Each Treatment Option?
Observation and monitoring:
| Benefits | Risks |
| Non-invasive approach for mild cases | May not prevent further vision loss in more severe cases |
| Allows for early detection of disease progression | Delayed treatment could lead to worsening of the condition |
Laser photocoagulation:
| Benefits | Risks |
| Effective in preventing the progression of proliferative retinopathy | Potential for retinal scarring or burns |
| Reduces the risk of vision loss | May cause temporary or permanent loss of peripheral vision |
Intravitreal injections:
| Benefits | Risks |
| Inhibits the growth of abnormal blood vessels | Possible side effects such as eye pain, infection, or inflammation |
| Decreases retinal swelling | Risk of retinal detachment or elevated intraocular pressure |
Vitrectomy:
| Benefits | Risks |
| Effective for treating advanced retinopathy with complications | Invasive surgical procedure with potential complications |
| Can repair retinal damage and clear vitreous hemorrhage | Risk of infection, retinal detachment, or elevated intraocular pressure |
Managing underlying sickle cell disease:
| Benefits | Risks |
| Addresses the root cause of sickle cell retinopathy | Side effects and risks associated with sickle cell disease treatments, such as blood transfusions or medications |
| Prevents further complications |
Patients should discuss the benefits and risks of each treatment option with their healthcare provider and ophthalmologist to make an informed decision based on their individual needs and the severity of their sickle cell retinopathy.
Lifestyle Changes and Management
While there is no cure for sickle cell retinopathy, certain lifestyle changes and management strategies can help minimize the risk of complications and improve overall eye health. Here are some recommendations:
Regular Eye Examinations
Schedule regular comprehensive eye exams with an ophthalmologist experienced in managing sickle cell retinopathy. Early detection and monitoring of the condition can help prevent vision loss.
Manage Underlying Sickle Cell Disease
Work closely with your healthcare provider to manage your sickle cell disease. This may include medications, blood transfusions, or other treatments to reduce the frequency and severity of sickle cell crises.
Maintain a Healthy Lifestyle
Eating a balanced diet, exercising regularly, and getting enough sleep can help improve overall health and well-being, which may contribute to better eye health.
Stay Well-hydrated
Dehydration can increase the risk of sickle cell crises, which can worsen retinopathy. Drink plenty of water and avoid excessive caffeine and alcohol consumption.
Avoid High Altitudes and Extreme Temperatures
Both high altitudes and extreme temperatures can trigger sickle cell crises. If possible, avoid these conditions or take necessary precautions when exposed to them.
Avoid Smoking
Smoking can have detrimental effects on blood circulation and overall health, potentially worsening sickle cell retinopathy. Quitting smoking can improve your overall health and reduce the risk of complications.
Manage Stress
High levels of stress can negatively impact your overall health and potentially worsen sickle cell retinopathy. Practice stress-reducing techniques such as meditation, yoga, or deep breathing exercises to help manage stress.
Educate Yourself and Others
Learn as much as you can about sickle cell retinopathy and sickle cell disease. Share your knowledge with friends, family, and support groups to raise awareness and help others facing similar challenges.
Conclusion
Sickle cell retinopathy is a serious complication of sickle cell disease that affects the retina, potentially leading to vision loss if left untreated. It is essential for individuals with sickle cell disease to be aware of the different types of retinopathy, as well as the causes, risk factors, and symptoms associated with the condition. Early detection and intervention through regular eye examinations are crucial in preventing and managing complications.
There are various treatment options available, each with its own benefits and risks. Working closely with healthcare professionals experienced in managing sickle cell retinopathy will help determine the most appropriate course of action. Additionally, adopting specific lifestyle changes and management strategies can contribute to better eye health and overall well-being.
In conclusion, understanding and managing sickle cell retinopathy is crucial for individuals with sickle cell disease. By staying informed, proactively addressing the condition, and making the necessary lifestyle adjustments, those affected can minimize the risk of complications and maintain their vision.
(1).jpg)