From Diagnosis to Recovery: Navigating the Journey of Ocular Syphilis
What is Ocular Syphilis?
Ocular syphilis is an inflammatory eye condition caused by the bacterium Treponema pallidum, the same organism responsible for syphilis, a sexually transmitted infection (STI). Ocular syphilis can occur at any stage of syphilis, including primary, secondary, latent, and tertiary stages. The infection can affect various structures within the eye, such as the uvea, retina, optic nerve, and the cornea, leading to a wide range of symptoms and potential vision loss if left untreated.
Although ocular syphilis is relatively rare, it is considered a serious medical condition that warrants prompt diagnosis and treatment. In recent years, there has been a resurgence of syphilis cases worldwide, which has led to increased concern about the potential for ocular complications. Early detection and appropriate treatment of both the underlying syphilis infection and its ocular manifestations are crucial to prevent long-term complications and preserve vision.
The Science of Ocular Syphilis: How It Affects the Eye
Ocular syphilis occurs when the Treponema pallidum bacterium spreads through the bloodstream and reaches the eye's tissues, causing inflammation and damage. The infection can affect various structures within the eye, leading to a range of ocular manifestations. Some of the most common ways ocular syphilis impacts the eye include:
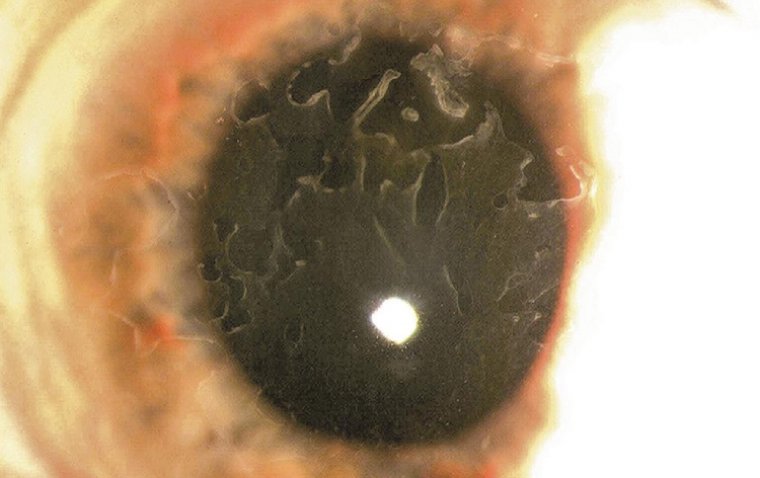
1. Uveitis: Inflammation of the uveal tract, which includes the iris, ciliary body, and choroid, is one of the most common manifestations of ocular syphilis. Uveitis can lead to symptoms such as eye pain, redness, light sensitivity, and blurred vision. If not treated promptly, it can result in complications like glaucoma, cataracts, or retinal detachment.
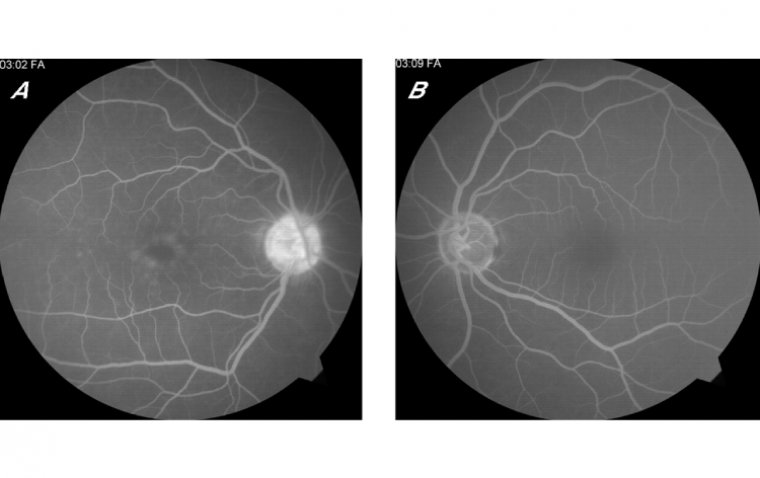
2. Retinitis: Inflammation of the retina can cause symptoms such as floaters, flashing lights, and vision loss. Retinitis due to ocular syphilis can lead to permanent damage to the retinal cells, potentially resulting in irreversible vision loss.
3. Optic neuritis: Inflammation of the optic nerve can cause sudden vision loss, usually in one eye, along with pain upon eye movement. Optic neuritis may result in permanent vision loss if left untreated.
4. Interstitial keratitis: Inflammation of the cornea may lead to corneal scarring, which can cause vision impairment or even blindness if severe. Symptoms of interstitial keratitis include eye pain, redness, tearing, and light sensitivity.
5. Vitritis: Inflammation of the vitreous humor, the gel-like substance within the eye, can cause floaters and blurred vision.
Causes of Ocular Syphilis
Ocular syphilis is caused by the bacterium Treponema pallidum, which is responsible for the sexually transmitted infection syphilis. The bacterium can infect the eye when it spreads through the bloodstream during any stage of the syphilis infection. Some factors that contribute to the development of ocular syphilis include:
● Unprotected sexual contact: Syphilis is primarily transmitted through sexual contact, including vaginal, anal, and oral sex, with an infected partner. Engaging in unprotected sex increases the risk of contracting syphilis, and subsequently, developing ocular syphilis.
● Mother-to-child transmission: Pregnant women with syphilis can pass the infection to their unborn child, which can result in congenital syphilis. Infants with congenital syphilis are at risk of developing ocular syphilis, leading to serious eye complications.
● Late-stage syphilis: Although ocular syphilis can occur at any stage of the infection, it is more likely to develop during the late or tertiary stage of syphilis. At this stage, the bacterium can infiltrate various organs and tissues, including the eyes, and cause extensive damage.
●Weakened immune system: Individuals with compromised immune systems, such as those with HIV/AIDS or those undergoing immunosuppressive treatments, may be more susceptible to developing ocular syphilis due to their reduced ability to fight off infections.
● Lack of timely treatment: Failure to diagnose and treat syphilis in its early stages can lead to a higher risk of developing ocular syphilis and other complications. Early detection and appropriate treatment of syphilis are crucial to prevent the spread of the infection and the development of severe complications, including ocular syphilis.
Signs and Symptoms of Ocular Syphilis
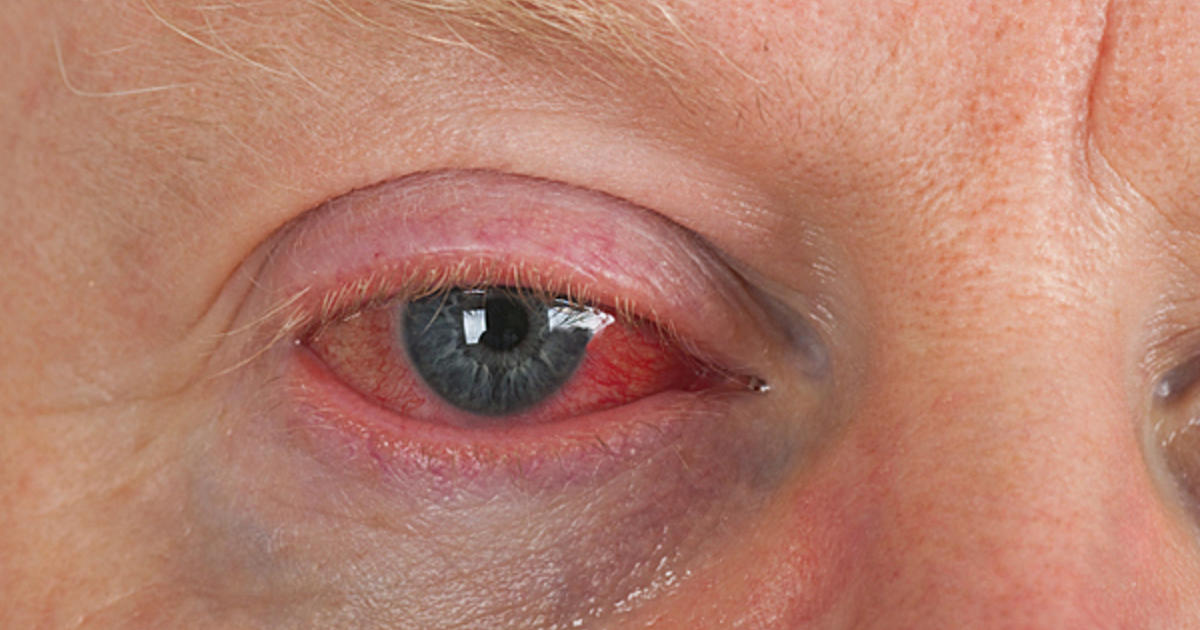
The signs and symptoms of ocular syphilis can vary depending on the specific structures within the eye that are affected by the infection. Some common symptoms include:
Eye pain: Pain or discomfort in the affected eye is a common symptom, particularly when the infection leads to uveitis or interstitial keratitis.
Redness: Inflammation caused by ocular syphilis can result in redness or bloodshot appearance of the eye.
Sensitivity to light (photophobia): Inflammation within the eye can cause increased sensitivity to light, making it uncomfortable or painful to be in bright environments.
Blurred vision: Inflammation or damage to various eye structures, such as the cornea, retina, or optic nerve, can lead to blurred or decreased vision.
Vision loss: Sudden or gradual vision loss can occur due to optic neuritis, retinitis, or severe corneal scarring.
Floaters: The presence of floaters, which appear as small specks or spots drifting across the field of vision, can be indicative of retinitis or vitritis.
Flashes of light: Individuals with retinitis may experience sudden, brief flashes of light in their field of vision.
Halos around lights: Some people with ocular syphilis may see halos or rings around lights, which can be a sign of corneal or retinal involvement.
Management of Ocular Syphilis
Effective management of ocular syphilis involves addressing both the ocular symptoms and the underlying syphilis infection. A multidisciplinary approach, including ophthalmologists and infectious disease specialists, is often necessary for optimal care. Key aspects of ocular syphilis management include:
1. Antibiotic treatment: The primary treatment for ocular syphilis is the administration of antibiotics, typically intravenous (IV) or intramuscular (IM) penicillin, to eliminate the causative bacterium, Treponema pallidum. The duration and dosage of antibiotic therapy may vary depending on the severity of the infection and the patient's overall health.
2. Corticosteroids: In some cases, corticosteroids may be prescribed to reduce inflammation and alleviate ocular symptoms. Corticosteroids can be administered orally, topically, or through injections, depending on the specific eye structures affected and the severity of the condition.Monitoring and follow-up: Regular follow-up visits with healthcare professionals are crucial for monitoring the response to treatment and ensuring the resolution of the infection. Ophthalmologic and serologic evaluations may be conducted periodically to assess the progress and effectiveness of the treatment.
3. Treatment of complications: If ocular syphilis has led to complications such as glaucoma, cataracts, or retinal detachment, additional treatments may be necessary. These can include medications to control intraocular pressure, surgical interventions to address cataracts or retinal detachment, or laser procedures to manage glaucoma.
4. HIV testing and management: As syphilis and HIV infections are often linked, it is essential to test for HIV and, if necessary, initiate appropriate treatment and management strategies for HIV-positive patients.
Prompt diagnosis and treatment of ocular syphilis are crucial for preventing long-term complications and preserving vision. Comprehensive management of the condition, including addressing the underlying syphilis infection and any ocular complications, can help optimize patient outcomes.
Procedures, Antibiotic Treatment and Follow-Up Care
Management of ocular syphilis requires a combination of appropriate procedures, antibiotic treatment, and follow-up care to ensure optimal outcomes for patients. Here's a closer look at each aspect of the management process:
1. Procedures: In some cases, ocular syphilis may require surgical or laser procedures to treat complications such as glaucoma, cataracts, or retinal detachment. These procedures may include:
● Trabeculectomy: A surgical procedure to improve drainage of aqueous humor and reduce intraocular pressure in glaucoma patients.
● Laser peripheral iridotomy: A laser procedure used to create a small hole in the iris, allowing fluid to flow more freely within the eye and helping to reduce intraocular pressure.
● Cataract surgery: A procedure to remove the clouded lens (cataract) and replace it with an artificial intraocular lens, restoring visual acuity.
2. Antibiotic treatment: The cornerstone of ocular syphilis management is antibiotic therapy to target the underlying Treponema pallidum infection. The preferred treatment is penicillin, administered either intravenously (IV) or intramuscularly (IM) for a specific duration, depending on the severity of the infection and the patient's overall health. Alternative antibiotics, such as doxycycline or ceftriaxone, may be used for patients with penicillin allergies.
3. Follow-up care: Regular follow-up visits with healthcare professionals are vital for monitoring the patient's response to treatment and ensuring the resolution of the infection. The follow-up care may involve:
● Ophthalmologic evaluations: Periodic eye exams, including visual acuity testing and a slit-lamp examination, are essential to assess the progress of the ocular condition and the effectiveness of the treatment.
● Serologic testing: Blood tests may be conducted to monitor the patient's response to antibiotic therapy and confirm the resolution of the syphilis infection.
● Additional testing and treatment: If the patient is co-infected with HIV, further testing and treatment may be necessary to manage both conditions effectively.
By incorporating appropriate procedures, antibiotic treatment, and diligent follow-up care, healthcare professionals can provide comprehensive management of ocular syphilis and help prevent long-term complications and vision loss.
Preventing Ocular Syphilis
Preventing ocular syphilis primarily involves reducing the risk of contracting syphilis, as well as early detection and treatment of the infection. Here are some key strategies to help prevent ocular syphilis:
1. Practice safe sex: Consistent and correct use of condoms during sexual activity can significantly reduce the risk of contracting syphilis and other sexually transmitted infections (STIs). Additionally, maintaining a monogamous relationship with a partner who has been tested and is known to be uninfected can further decrease the risk.
2. Get tested regularly: Regular testing for syphilis and other STIs is crucial, especially for individuals at higher risk, such as those with multiple sexual partners, men who have sex with men, or people with a history of STIs. Early detection and treatment of syphilis can help prevent complications, including ocular syphilis.
3. Seek prompt treatment for syphilis: If diagnosed with syphilis, it is essential to complete the prescribed course of antibiotics and follow all medical advice to effectively treat the infection and prevent complications. It's also crucial to notify any sexual partners, so they can also be tested and treated if necessary.
4. HIV testing and management: Since syphilis and HIV infections are often linked, it's essential to get tested for HIV and, if necessary, initiate appropriate treatment and management strategies for HIV-positive patients. This can help prevent complications, including ocular syphilis.
5. Monitor your eye health: Regular eye exams and promptly addressing any unusual ocular symptoms can help ensure early detection and treatment of any eye conditions, including ocular syphilis.
To Conclude…
Ocular syphilis is a potentially serious eye condition resulting from the spread of the Treponema pallidum bacterium to the eyes. As a complication of syphilis, it can lead to various symptoms, including vision impairment and eye inflammation. Early detection and prompt treatment of the underlying infection are crucial in managing ocular syphilis and preventing long-term complications.
A multidisciplinary approach involving ophthalmologists and infectious disease specialists ensures optimal care for patients with ocular syphilis. Treatment typically involves antibiotics, corticosteroids, and, in some cases, surgical or laser procedures to address complications such as glaucoma, cataracts, or retinal detachment. Regular follow-up care and monitoring are essential for successful treatment outcomes.
Prevention of ocular syphilis relies on reducing the risk of contracting syphilis through safe sex practices, regular testing, and prompt treatment of any diagnosed infections. Moreover, maintaining good eye health and regular eye exams can help detect and address ocular syphilis early. By raising awareness about this condition and emphasizing the importance of prevention and early intervention, we can work towards minimizing the impact of ocular syphilis on individuals and their vision.
(1).jpg)