Understanding Leber's Hereditary Optic Neuropathy (LHON)
As we gaze into the intricate tapestry of ophthalmic disorders, we encounter some conditions that seem to put us in the spotlight of a thriller movie. Such is the case with Leber's Hereditary Optic Neuropathy (LHON), a condition whose plot intertwines genetics, vision, and mystery. In our quest to demystify LHON, we delve into its genetic roots, explore its symptomatology, uncover the tools for its diagnosis, and light the way for its treatment and management.
What Is Leber's Hereditary Optic Neuropathy?
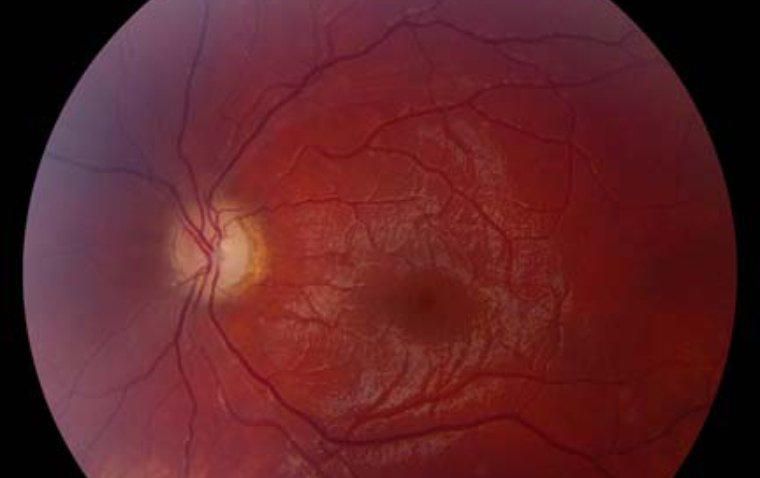
Leber's Hereditary Optic Neuropathy (LHON) is a rare, inherited mitochondrial disorder that predominantly affects the optic nerve, leading to acute or subacute loss of central vision. This disease usually begins in one eye, with the other eye commonly affected within weeks to months.
Genetics of LHON
LHON is primarily caused by mutations in one of the three genes located in the mitochondrial DNA: MT-ND1, MT-ND4, and MT-ND6. These genes are crucial for the functioning of the mitochondria, the energy-generating centers of the cell. Mutations can affect the ability of the mitochondria to produce energy, leading to the impairment and eventual death of retinal ganglion cells and optic nerve fibers.
Symptoms and Diagnosis of LHON
- Early signs and symptoms of LHON
The course of LHON often begins with an insidious onset of symptoms that may initially seem innocuous. The defining feature of LHON is painless central vision loss, which typically emerges suddenly and usually during young adulthood. However, it's important to note that LHON can manifest at any age, from childhood to late adulthood.
Symptoms typically begin in one eye, with the other eye often affected within a few weeks to several months. While central vision loss is the hallmark of the disease, there are other signs and symptoms that may accompany or precede it:
● Decreased color vision or color blindness: Patients may find it challenging to distinguish between colors, particularly red and green.
● Blurry or cloudy vision: Images may appear unfocused or hazy.
● Flashing lights or floaters: Some individuals might perceive flashing lights or floating specks.
● Difficulty adapting to low-light conditions: Patients may find it increasingly difficult to navigate in dimly lit environments.
Diagnostic Tests and Procedures Used to Diagnose LHON
Diagnosing LHON involves a combination of clinical evaluation, family history, and several diagnostic tests. The goal is to identify the characteristic signs of the disease and confirm the presence of pathogenic mitochondrial DNA mutations.
1. Clinical Evaluation and Family History: An ophthalmologist will perform a comprehensive eye examination and take a detailed family history. The sudden onset of bilateral vision loss in a young adult, especially a male, raises the suspicion of LHON.
2. Molecular Genetic Testing: To confirm the diagnosis, molecular genetic testing is performed to identify the three primary mitochondrial DNA mutations associated with LHON. These mutations affect the MT-ND1, MT-ND4, and MT-ND6 genes.
3. Visual Field Testing: This test assesses the patient's peripheral vision and can detect the central or cecocentral scotoma typically present in LHON.
4. Optical Coherence Tomography (OCT): OCT is a non-invasive imaging test that uses light waves to take cross-section pictures of the retina. It can demonstrate the characteristic pattern of retinal nerve fiber layer (RNFL) loss in LHON.
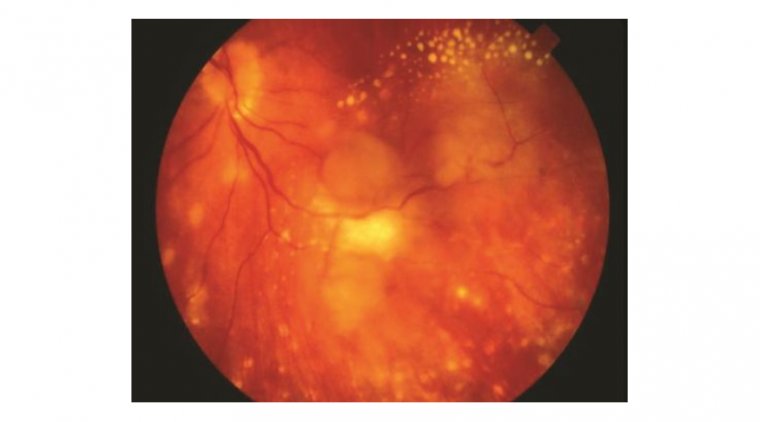
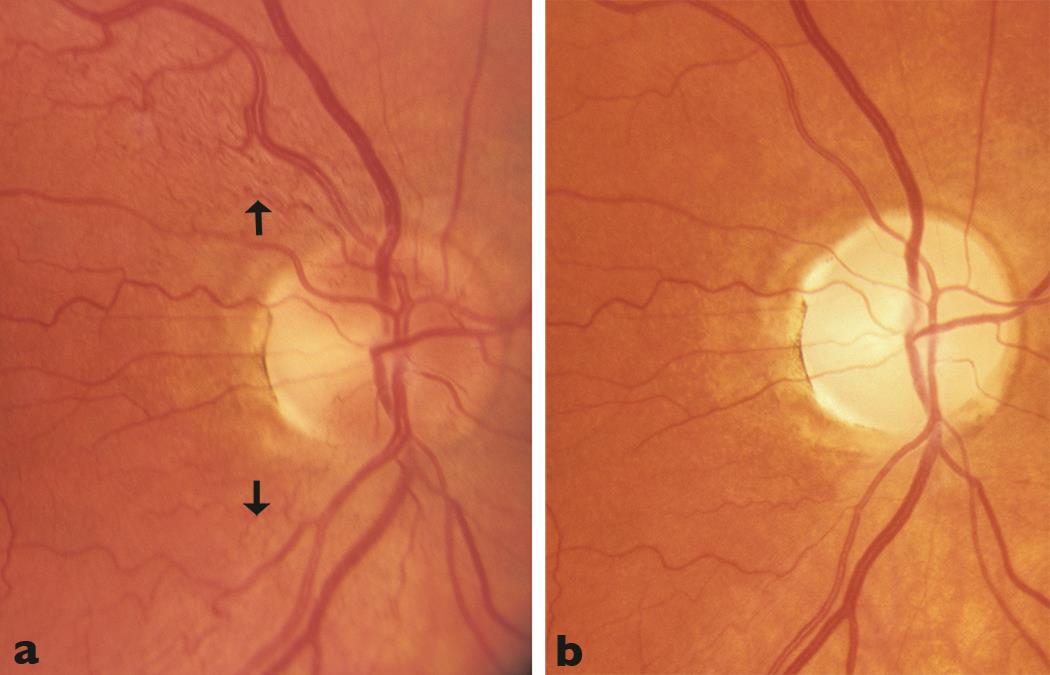
5. Fundus Examination: Examination of the fundus (the interior surface of the eye) can reveal swelling of the optic nerve head (papillitis) or pseudoedema of the optic disc, particularly in the early stages of the disease.
By putting the pieces of the puzzle together, clinicians can diagnose LHON and initiate the best possible management plan to support patients on their journey with this condition.
Treatment and Management of LHON
Navigating the complexities of LHON treatment requires a multifaceted approach that incorporates current interventions, supportive and symptomatic management, as well as a keen eye on emerging therapies.
Current Treatments and Interventions for LHON
Despite significant advancements in medical science, a definitive cure for LHON remains elusive. Treatment is thus largely focused on supportive care and symptom management, aiming to maximize the quality of life for patients and reduce the impact of vision loss.
A promising intervention that has come to light in recent years is idebenone, a synthetic antioxidant. Idebenone works by bypassing the defective mitochondrial complex I – the biochemical root of LHON – to enhance cellular energy production. Several studies have suggested that idebenone may improve vision or halt further vision loss in some people with LHON, making it a beacon of hope in the treatment landscape
Supportive and Symptomatic Management of LHON
Supportive care for LHON takes a holistic approach, addressing not just the physical, but also the psychological and emotional aspects of the disease. Key components of supportive care include:
● Visual aids: Devices such as magnifiers, large-print devices, and electronic reading aids can help patients optimize their remaining vision.
● Occupational therapy: Occupational therapists can assist patients in adapting to vision loss, teaching them new skills to manage daily activities and maintain independence.
● Low-vision rehabilitation services: These services offer specialized support, including guidance on lighting and contrast enhancement techniques, mobility training, and counseling to help patients cope with their vision loss.
Emerging Therapies and Potential Future Treatments for LHON
As researchers continue to unravel the genetic intricacies of LHON, several promising therapies are on the horizon:
● Gene Therapy: This involves introducing a healthy copy of the gene into the patient's cells, thereby compensating for the defective gene. Several preclinical and clinical trials are underway to evaluate the safety and efficacy of gene therapy in LHON.
● Stem Cell Therapy: Stem cells have the potential to regenerate or repair the damaged optic nerve cells, offering another promising approach. While still in the experimental stages, stem cell therapy could potentially change the course of treatment for LHON in the future.
Can LHON Be Prevented?
While LHON can't be prevented in the traditional sense, there are strategies to manage risk and potentially delay or mitigate the onset of symptoms.
● Genetic counseling and testing for LHON
● For families with a history of LHON, genetic counseling plays a pivotal role in managing the disease. Genetic testing can identify carriers of LHON mutations, offering them a clear understanding of their risk profile and the chances of passing the condition to their children. Moreover, it provides an opportunity for carriers to make informed decisions about family planning and lifestyle modifications.
● Lifestyle modifications
● Given the potential for certain environmental factors to trigger the onset of symptoms in carriers of LHON mutations, specific lifestyle modifications are recommended. These include:
● Avoiding smoking: Tobacco smoke is a known mitochondrial toxin that can exacerbate the dysfunction caused by LHON mutations.
● Limiting alcohol consumption: Excessive alcohol can have a similar detrimental effect on mitochondrial health.
● Maintaining a balanced diet and regular exercise: Good overall health can support mitochondrial function and potentially delay the onset of symptoms.
In the grand scheme of LHON management, understanding the disease, adopting supportive care strategies, staying updated with emerging therapies, and embracing proactive preventive measures can make a world of difference for those living with this condition.
Conclusion
In this odyssey through the complex world of Leber's Hereditary Optic Neuropathy, we've shone a light on the genetic origins, the signs and symptoms, the diagnostic procedures, and the current state of treatment and management. As we continue our journey in understanding and treating this condition, it's clear that the path ahead is as illuminating as it is challenging. But, as they say, every challenge offers an opportunity - and in the case of LHON, the opportunity is nothing less than the chance to rewrite a patient's story from sudden darkness to a gradual return of light.
(1).jpg)