An Asymmetrical Gaze: A Closer Look at Relative Afferent Pupillary Defect
Get ready to dive into the "pupil"-lating world of the 'Relative Afferent Pupillary Defect' (RAPD). But don't let the term "defect" have you "seeing double" with concern. In the vast cosmos of ophthalmology, it's merely another star, albeit one that blinks a bit asymmetrically, shedding light on the complexities of our field. So, let's reflect together, illuminating this fascinating topic from all angles. Puns aside, it's time for a closer examination of this intriguing phenomenon and what it means in our day-to-day practice. Brace yourselves; it's going to be an "eye-opening" journey!
What Is Relative Afferent Pupillary Defect?
Relative Afferent Pupillary Defect (RAPD), also known as Marcus Gunn pupil, is a fascinating physiological anomaly that sheds light on the intricate interplay between light, vision, and our nervous system. It's a condition that spotlights the subtleties of ocular examinations and reaffirms the interconnected nature of visual pathways.
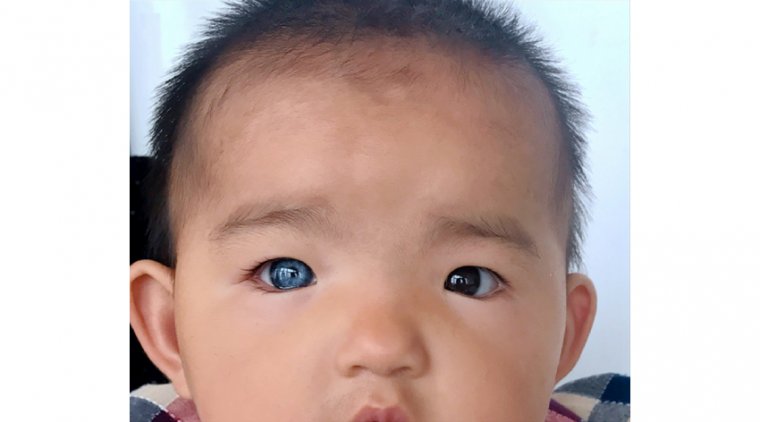
So, what exactly is RAPD? In simple terms, it's an abnormal pupillary response to light stimuli. In a normal eye, direct light exposure induces an equal constriction in both pupils, a reaction known as the direct and consensual light reflex. However, in RAPD, the affected pupil exhibits a paradoxical response—it dilates when directly illuminated, even as the other eye maintains normal constriction.
This abnormal reaction to light is not a standalone condition but a revealing symptom of a deeper issue—optic nerve dysfunction or asymmetrical impairment in the visual pathway. RAPD is typically an indication of unilateral or asymmetric damage to the retina, optic nerve, or optic tract. It is essentially a game of imbalance, where one side's visual signals fail to match the strength and speed of the other.
Causes and Risk Factors of Relative Afferent Pupillary Defect
Relative Afferent Pupillary Defect (RAPD) essentially manifests as a sign rather than a standalone disease, highlighting an underlying imbalance in the visual afferent pathways. This intriguing phenomenon can occur due to a multitude of causes and risk factors, all of which impact the optic nerve or the visual pathway in some way.
1. Underlying Causes: The most common causes of RAPD are conditions that lead to asymmetric or unilateral optic nerve damage or impairment. These include:
2. Optic Neuropathies: This includes conditions like ischemic optic neuropathy, optic neuritis, Leber's Hereditary Optic Neuropathy, or glaucoma. Each of these conditions can affect the optic nerve's ability to transmit visual information, leading to RAPD.
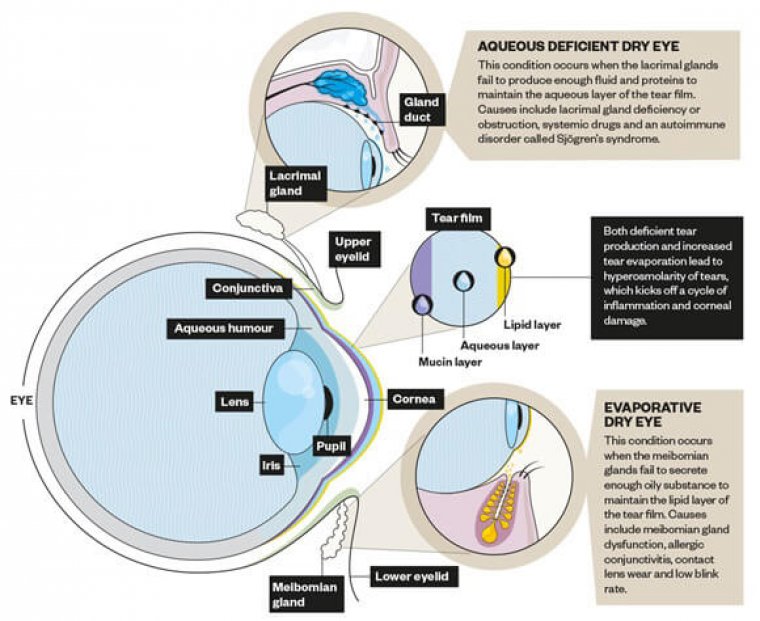
3. Retinal Diseases: Certain conditions affecting the retina, such as retinal detachment, retinal vascular occlusions, or severe macular degeneration, can also result in RAPD.
4. Lesions Affecting the Visual Pathway: Any severe or asymmetrical lesion along the optic tract, lateral geniculate body, or optic radiations can result in RAPD.
Risk Factors
Several risk factors can predispose an individual to the conditions causing RAPD. These include:
● Traumatic Injury: Any traumatic injury to the eye or optic nerve can potentially lead to RAPD.
● Autoimmune Conditions: Conditions like multiple sclerosis, which can cause optic neuritis, are potential risk factors.
● Vascular Risk Factors: Conditions such as hypertension or diabetes can predispose to ischemic optic neuropathy.
● Age and Genetics: Age-related macular degeneration or genetically-linked conditions like Leber's Hereditary Optic Neuropathy can also be risk factors for RAPD.
Signs and Symptoms of Relative Afferent Pupillary Defect
Relative Afferent Pupillary Defect (RAPD) is a curious condition that offers a unique display of visual physiology. Its signs are subtle, and while its symptoms may often be silent, it is a beacon pointing towards more profound ocular or neurological issues.
While RAPD itself does not cause symptoms and is typically discovered during a clinical examination, it is indicative of underlying conditions that may manifest various symptoms. These might include:
1. Reduced Visual Acuity: Some patients may notice a decrease in sharpness or clarity of vision, depending on the underlying cause.
2. Visual Field Defects: Patients may experience defects in their visual field. This could range from blind spots to more extensive field loss, such as tunnel vision or hemianopia.
3. Color Vision Abnormalities: Depending on the extent and location of the optic nerve damage, there may be an alteration in color perception.
4. Pain or Discomfort: Some conditions that result in RAPD, such as optic neuritis, may also present with eye pain or discomfort, particularly with eye movement.
How to Diagnose Relative Afferent Pupillary Defect
Diagnosing Relative Afferent Pupillary Defect (RAPD) requires a blend of keen observation, technical expertise, and a thoughtful understanding of the visual pathway. While the steps involved are simple, the diagnosis offers crucial insights into potentially serious ocular and neurological conditions.
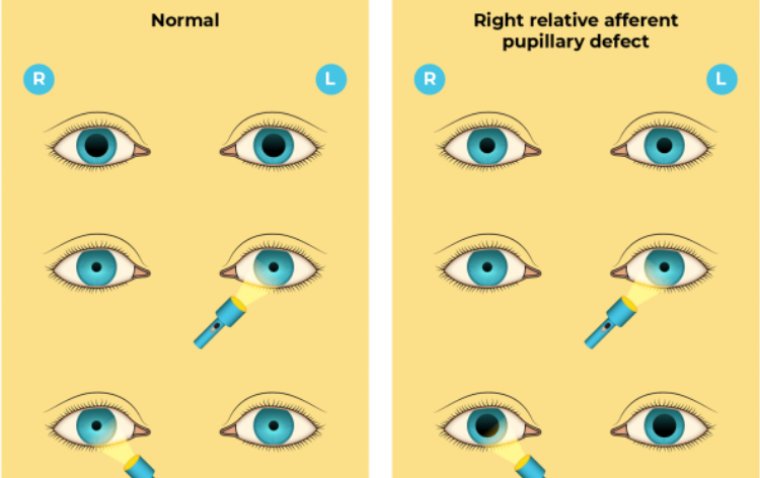
The cornerstone of RAPD diagnosis is the swinging flashlight test, a straightforward yet elegant examination of the pupillary light reflex. Here's how it works:
1. Dim the room lights to encourage pupillary dilation, thus making changes in pupil size easier to observe.
2. Shine a penlight into one eye and observe both pupils constrict (direct and consensual response).
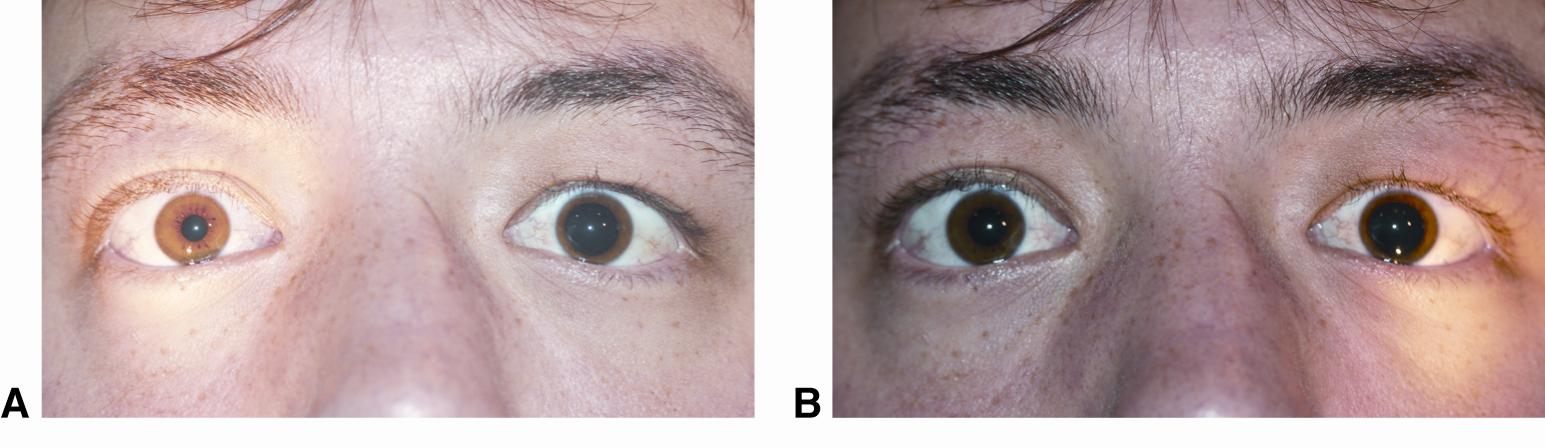
3. Then, swiftly swing the light to illuminate the other eye. In a normal response, both pupils should remain constricted. However, in RAPD, the affected eye's pupil will paradoxically dilate or show less constriction when the light is swung to it.
This test relies on the principle of comparing pupillary responses between the affected and unaffected eyes. It can usually be performed with a simple penlight, but pupillometers, which offer a more precise measurement of pupillary reactions, can also be employed in certain settings.
The diagnostic journey doesn't stop at detecting RAPD. It's crucial to carry out a differential diagnosis to distinguish RAPD from other causes of pupillary abnormalities or optic nerve dysfunction. These could include physiological anisocoria, Adie's tonic pupil, or pharmacological causes, where the use of certain drugs can lead to an abnormal pupillary response.
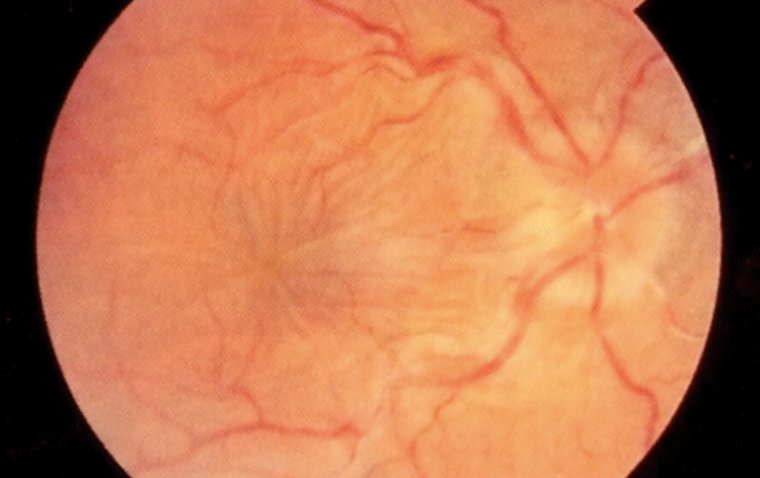
Moreover, once RAPD is identified, further investigations are warranted to uncover the underlying condition causing it. These might include fundus examination, visual field testing, color vision testing, and potentially neuroimaging studies.
Underlying Conditions and Treatment
Relative Afferent Pupillary Defect (RAPD) is like a canary in the coal mine, its presence a clear indication that something is amiss within the visual pathway. To manage RAPD effectively, we must first understand and address its root causes.
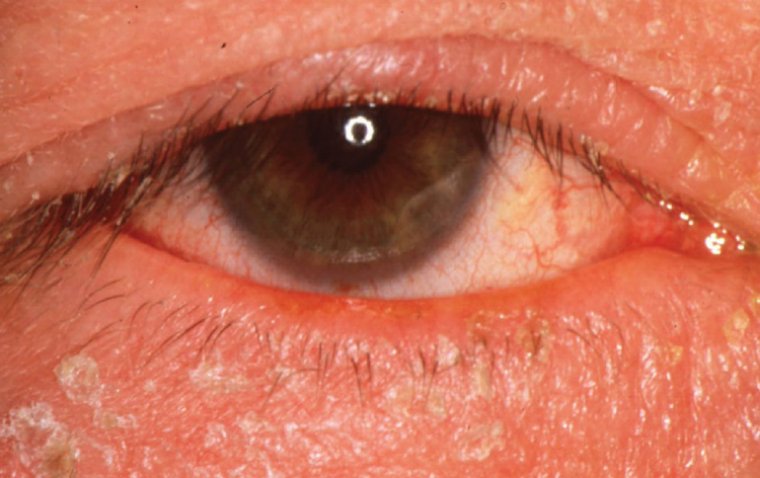
RAPD is typically associated with a multitude of underlying conditions that cause unilateral or asymmetric optic nerve damage or visual pathway impairment. These include retinal detachment, retinal vascular occlusions, optic neuritis, ischemic optic neuropathy, severe glaucoma, and even central nervous system lesions such as stroke, multiple sclerosis, or brain tumors.
The treatment of RAPD is inherently tied to the management of these underlying conditions. The primary goal is to prevent further damage, preserve existing vision, and, where possible, improve visual function.
Depending on the specific condition contributing to RAPD, potential treatments might include:
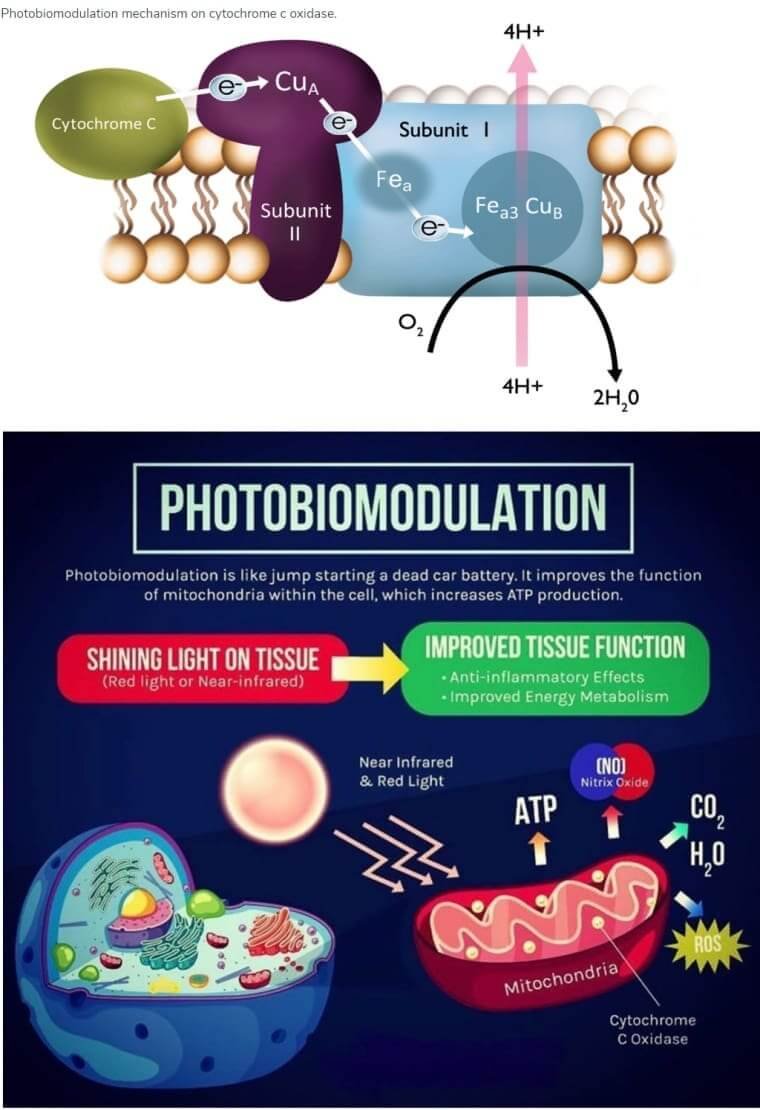
● Optic Nerve Rehabilitation: In cases of optic neuropathy, strategies to rehabilitate the optic nerve might be employed. This could include therapies targeting intraocular pressure control in glaucoma or improving optic nerve blood flow in ischemic conditions.
● Anti-Inflammatory Medications: For optic neuritis, often associated with autoimmune conditions like multiple sclerosis, corticosteroids or other immunosuppressive agents might be prescribed to reduce inflammation.
● Surgery: In cases where RAPD is associated with retinal detachment or certain tumors, surgical intervention might be necessary to repair the retina or remove the tumor.
● Vascular Risk Factor Management: For vascular conditions like diabetes or hypertension that could lead to retinal vascular occlusions or ischemic optic neuropathy, managing these risk factors is paramount.
● Neuroprotective Agents: Emerging research suggests potential roles for various neuroprotective agents in preserving optic nerve function, particularly in glaucoma.
Management and Prognosis
Managing Relative Afferent Pupillary Defect (RAPD) is an enduring process, extending far beyond initial diagnosis and treatment. It involves continuous monitoring, timely intervention, and long-term strategies tailored to each patient's unique circumstances.
Long-term management is largely contingent on the nature of the underlying condition causing RAPD. In general, it involves regular ophthalmological follow-ups to monitor the progress of the condition, adjust treatment regimens as necessary, and detect any new developments early.
In cases where RAPD is associated with chronic conditions like glaucoma, diabetes, or multiple sclerosis, management will include regular evaluations of these conditions, ensuring they are optimally controlled, and coordinating with other specialists as needed. Additionally, patients may require lifestyle modifications, adherence to medication regimens, or regular visual field and acuity testing.
Moreover, patient education plays a vital role in long-term management. It is crucial for patients to understand their condition, recognize any changes in vision or ocular comfort, and promptly report these changes to their healthcare provider.
The prognosis of RAPD depends significantly on the underlying cause and its response to treatment. Some conditions, like optic neuritis, may have a good prognosis with appropriate treatment, while others, like advanced glaucoma or ischemic optic neuropathy, might carry a more guarded prognosis.
Prognosis also hinges on the timing of diagnosis and intervention. Early detection and treatment generally lead to better outcomes. Therefore, prompt recognition of RAPD and initiation of appropriate management strategies are crucial.
To Conclude...
Relative Afferent Pupillary Defect (RAPD), also known as Marcus Gunn pupil, is a condition characterized by an abnormal pupillary light reflex due to optic nerve dysfunction or asymmetrical visual pathway impairment. Its causes include a variety of conditions such as optic nerve damage, retinal diseases, or lesions affecting the visual pathway.
Signs of RAPD primarily involve an abnormal pupillary response when light is shone into the affected eye compared to the healthy one. This anomaly, known as the Marcus Gunn sign, can be detected using the swinging flashlight test. Other associated symptoms, such as reduced visual acuity, visual field defects, or color vision abnormalities, might be present depending on the underlying cause.
Diagnosis of RAPD involves the swinging flashlight test and differentiation from other causes of pupillary abnormalities or optic nerve dysfunction. Further investigations are often required to identify the root cause of RAPD, which may involve fundus examination, visual field testing, color vision testing, and possibly neuroimaging studies.
Management and treatment of RAPD are tailored to the specific condition contributing to the defect, which can range from optic nerve rehabilitation and anti-inflammatory medications to surgery. Long-term management requires regular monitoring and patient education. Prognosis varies based on the underlying cause and its response to treatment.
In conclusion, RAPD is a significant diagnostic sign indicating underlying optic nerve or visual pathway damage. It serves as a crucial tool for ophthalmologists to uncover and address more serious conditions that might otherwise remain hidden.
(1).jpg)