The ABCs of Hypopyon: Causes, Symptoms, and Treatments
What is Hypopyon?
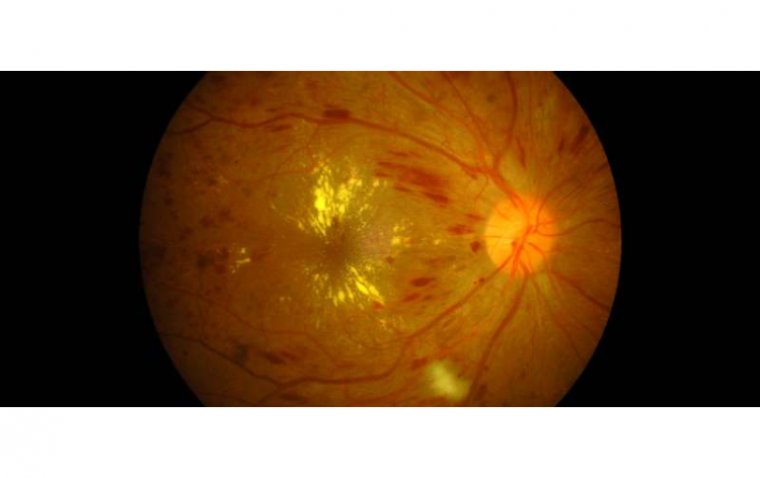
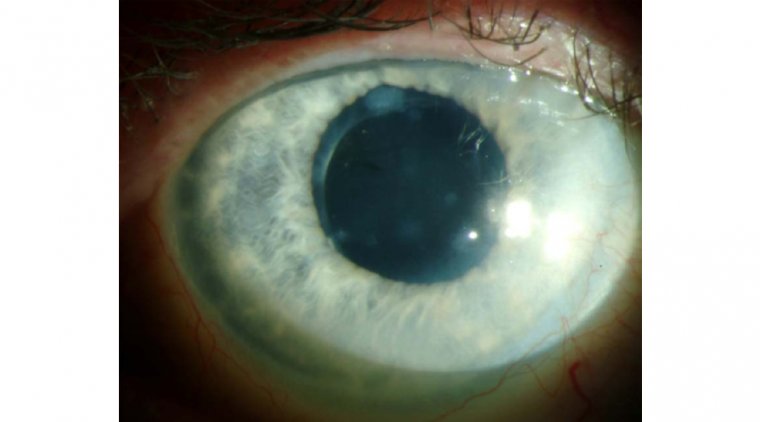
Hypopyon is a medical condition often associated with the eye, characterized by the accumulation of white blood cells or pus in the anterior chamber of the eye, which is the fluid-filled space between the cornea and the iris. This condition is a sign of inflammation and is not a disease in itself but a symptom of underlying eye diseases. Understanding hypopyon is crucial for early detection and treatment to prevent potential complications, including vision loss.
What Causes Hypopyon?
Hypopyon is primarily caused by inflammation in the eye, which can result from various conditions. The most common causes include uveitis (inflammation of the uveal tract), infections (such as endophthalmitis, which is an inflammation of the interior of the eye caused by infection), injuries, and surgeries that lead to eye trauma. Autoimmune diseases, such as Behçet's disease, can also lead to hypopyon. The underlying mechanism involves the body's immune response, leading to the accumulation of immune cells in the anterior chamber, manifesting as hypopyon.
Signs and Symptoms of Hypopyon
● Visible Presence of Hypopyon: A noticeable white or yellow layer at the bottom of the eye's anterior chamber, easily observed by the patient or healthcare provider.
● Redness: The eye may appear redder than usual, indicating inflammation or irritation.
● Pain: Discomfort or pain in the affected eye, ranging from mild to severe.
● Sensitivity to Light (Photophobia): Increased discomfort or pain in the eye when exposed to light.
● Blurred Vision: Visual clarity may be compromised, leading to fuzzy or unclear vision.
● Decreased Visual Acuity: A reduction in the sharpness of vision, making it difficult to see fine details.
The severity and combination of these symptoms can vary based on the underlying cause of the inflammation.
.jpg)
How to Diagnose Hypopyon
Diagnosing hypopyon typically involves a series of steps to accurately identify the presence of pus or white blood cells in the anterior chamber of the eye and to determine the underlying cause:
1. Slit Lamp Examination: A detailed inspection of the eye using a slit lamp microscope to visualize the anterior chamber and assess the presence and severity of hypopyon.
2. Medical History Review: Gathering detailed patient history to identify potential causes, including previous eye surgeries, trauma, systemic diseases, or symptoms of infection or inflammation.
3. Blood Tests: Conducting blood tests to detect signs of systemic infections or autoimmune conditions that could contribute to eye inflammation.
4. Imaging Studies:
● Ultrasound Biomicroscopy: To examine the interior structures of the eye in detail, helping to identify abnormalities or foreign bodies.
● Optical Coherence Tomography (OCT): May also be used to assess the retina and choroid for any signs of disease that could be related to hypopyon.
5. Aqueous Humor Analysis: Extracting a small sample of aqueous humor from the eye for laboratory analysis to identify infectious agents such as bacteria or fungi.
Hyphema vs Hypopyon?
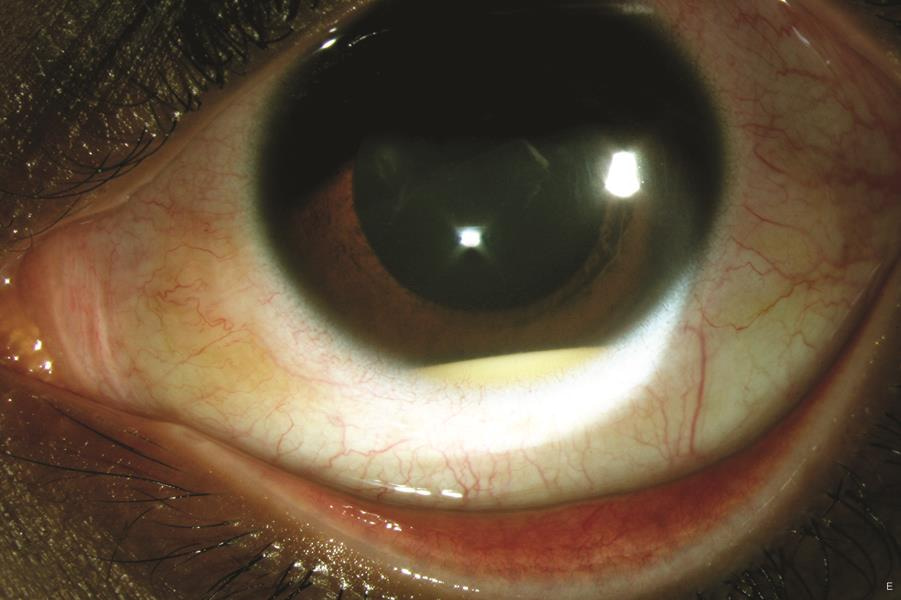
Hyphema and hypopyon are both eye conditions that manifest in the anterior chamber, the space between the cornea and the iris, but they differ significantly in their causes and the substances that accumulate. Hyphema is characterized by the presence of blood in the anterior chamber, typically resulting from trauma to the eye, surgeries, or less commonly, vascular abnormalities and certain eye diseases. It appears as a visible layer of blood or a blood-filled space and can vary in severity from a small spot to filling the entire anterior chamber.

Hyphema
On the other hand, hypopyon involves the accumulation of pus or white blood cells in the anterior chamber, indicative of inflammation, usually due to infections, autoimmune disorders, or post-surgical complications. Unlike the red or dark appearance of blood in hyphema, hypopyon is seen as a white or yellowish layer at the bottom of the anterior chamber. Both conditions require medical attention, as they can lead to vision impairment if left untreated, but their treatments differ, focusing on the underlying cause of the blood or pus accumulation.
Hypopyon
What Are the Complications of Hypopyon?
If hypopyon is not promptly and effectively treated, the condition can escalate, leading to several severe eye complications that significantly impact vision quality and health. Here’s a closer look at these potential complications:
1. Glaucoma: Hypopyon can contribute to the development of glaucoma, a group of eye conditions that damage the optic nerve, which is vital for good vision. This damage is often caused by abnormally high pressure in the eye. In the context of hypopyon, inflammation can lead to increased intraocular pressure, either through direct blockage of the eye's drainage channels or by causing scar tissue that interferes with aqueous humor outflow. Glaucoma resulting from hypopyon can be painful and lead to loss of vision if not treated promptly.
2. Corneal Edema: Corneal edema involves swelling of the cornea, the clear, dome-shaped surface that covers the front of the eye. This swelling can occur when inflammation from hypopyon interferes with the cornea's ability to maintain its normal fluid balance. The result is a hazy or cloudy appearance of the cornea, leading to blurred vision and halos around lights. Persistent corneal edema can damage the corneal cells, making recovery more difficult and potentially leading to permanent vision impairment.
3. Scarring: The inflammatory processes associated with hypopyon can lead to scarring of the eye's tissues, including the cornea and the uvea (the middle layer of the eye that includes the iris). Scarring can cause permanent alterations in the structure and function of the eye, leading to a range of visual disturbances. For instance, corneal scarring can obstruct light from entering the eye properly, reducing visual clarity and acuity. Similarly, scarring in the uvea can impair the eye's ability to regulate light entry and focus, further diminishing vision quality.
Treatment Options for Hypopyon
● Corticosteroids: Used to reduce inflammation in the eye. These can be administered as eye drops, oral medications, or injections, depending on the severity of the inflammation.
● Antibiotics or Antifungal Medications: Prescribed to treat infections that may cause hypopyon. The choice between antibiotics or antifungal medications depends on the type of infection identified through diagnostic tests.
● Immunosuppressive Drugs: Utilized for cases where hypopyon is related to autoimmune diseases. These drugs help manage the immune system's response, reducing inflammation and preventing further damage to the eye.
● Treatment for Eye Trauma or Surgery-Related Cases: In situations where hypopyon arises from eye trauma or post-surgical complications, specific treatments are tailored to heal the eye and prevent infection. This may include the use of antibiotic eye drops, protective eye wear, or additional surgical procedures to repair any damage.
The selection of a treatment regimen is carefully determined based on the underlying cause of the hypopyon and the overall health and needs of the patient. It is crucial to address both the symptom (hypopyon) and its root cause to ensure effective resolution and prevent recurrence.
Can Hypopyon Cause Blindness?
While hypopyon itself does not cause blindness, the conditions that lead to its development can impair vision if not treated appropriately. Severe inflammation, if unchecked, can damage vital structures of the eye, leading to vision loss. Therefore, addressing hypopyon and its underlying cause is crucial in preventing blindness.
Summary
Hypopyon is a significant indicator of inflammation within the eye that requires prompt medical attention. Recognizing the signs and symptoms of this condition can lead to early diagnosis and treatment, thereby preventing potential complications that could impair vision. With appropriate medical intervention, most individuals with hypopyon can recover without lasting damage to their eyesight. If you experience any symptoms of hypopyon, consult with an eye care professional immediately to protect your vision and health.
References:
(1).jpg)