Exploring the Causes, Symptoms and Treatment of Endophthalmitis
What Is Endophthalmitis?
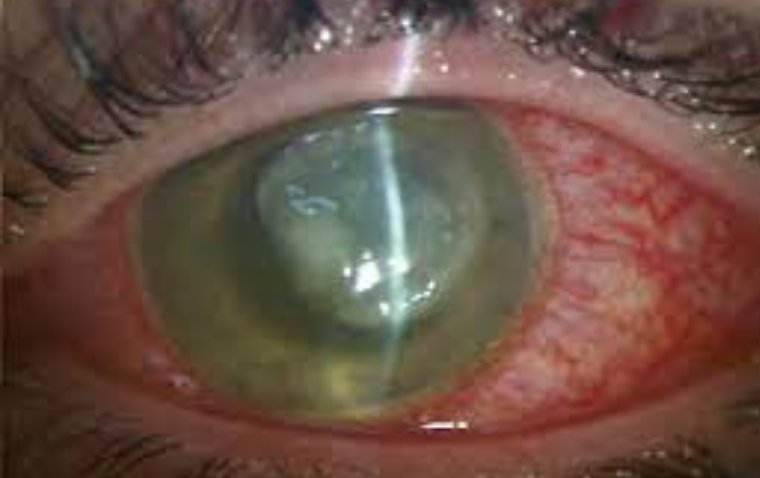
Endophthalmitis is a rare but serious eye condition that can lead to vision loss if not promptly treated. This infection targets the interior structures of the eye, causing inflammation and potential damage. Understanding the symptoms, causes, treatment options, and prevention strategies is crucial for maintaining optimal eye health and preventing severe complications.
Types of Endophthalmitis
There are primarily two main types of endophthalmitis: exogenous and endogenous. These categories are based on the source and route of infection:
1. Exogenous Endophthalmitis
Exogenous endophthalmitis occurs when an infection originates from an external source and enters the eye. This type of endophthalmitis is often associated with surgery or trauma.
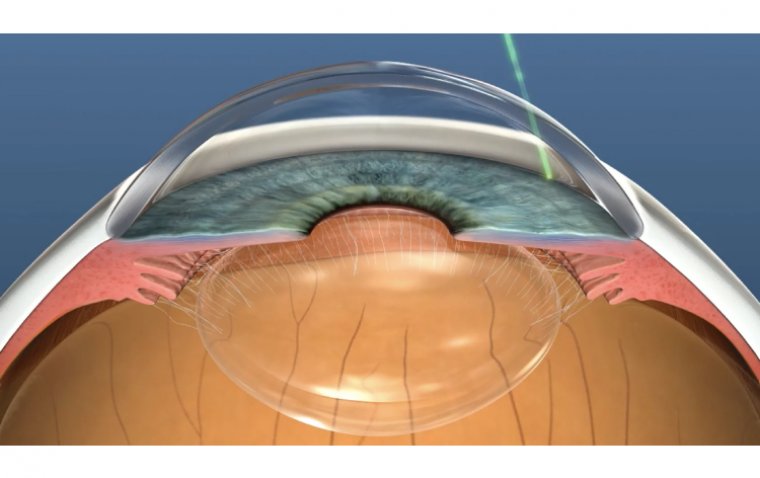
● Postoperative Endophthalmitis: This occurs as a complication of eye surgery, such as cataract surgery or vitrectomy. Bacteria or fungi may enter the eye during the surgical procedure, leading to infection.
● Traumatic Endophthalmitis: Trauma to the eye, such as from accidents, penetrating injuries, or foreign body entry, can introduce infectious agents into the eye's interior, triggering an infection.
2. Endogenous Endophthalmitis
Endogenous endophthalmitis arises when the infection originates from a distant source within the body and spreads to the eye through the bloodstream. This type is less common but can be more challenging to diagnose and treat.
● Hematogenous Spread: In this case, the infection travels from another part of the body (e.g., from an abscess, dental infection, or urinary tract infection) through the bloodstream to the eye. The infection may settle in the eye's interior structures, causing endophthalmitis.
● Systemic Infections: Conditions such as bacterial endocarditis, septicemia, or intravenous drug use can lead to systemic infections that have the potential to cause endogenous endophthalmitis.
3. Chronic Endophthalmitis
Chronic endophthalmitis is characterized by a slower onset and a milder form of infection. It can result from low-grade, indolent infections that gradually affect the eye's interior structures. This type may not present with as acute or severe symptoms as acute endophthalmitis.
4. Acute Endophthalmitis
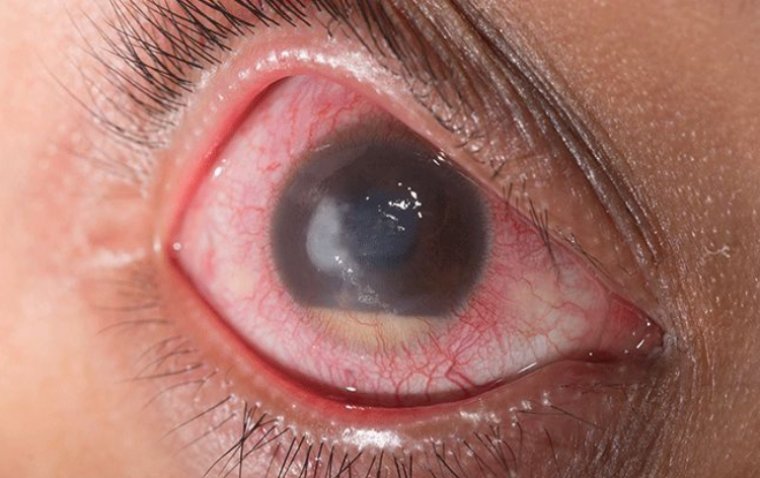
Acute endophthalmitis refers to a sudden and severe onset of infection within the eye's interior structures. It is typically associated with symptoms like pain, redness, and rapid vision loss. Acute endophthalmitis requires urgent medical attention and intervention.
The classification of endophthalmitis into these types helps guide diagnosis and treatment approaches based on the origin of the infection. Regardless of the type, early detection and prompt medical intervention are essential for minimizing the risk of vision loss and achieving the best possible outcomes.
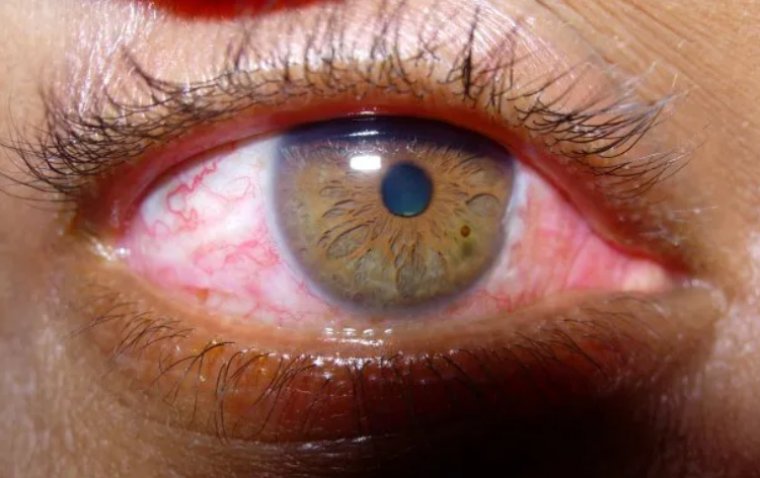
Endophthalmitis Symptoms
The symptoms of endophthalmitis can be alarming and should never be ignored. Individuals may experience redness, pain, and irritation in the affected eye. Blurred or reduced vision, along with increased sensitivity to light, are also common. In severe cases, patients might notice floaters or dark spots in their field of vision. If any of these symptoms arise, seeking immediate medical attention is imperative.,
What Causes Endophthalmitis?
Endophthalmitis is primarily caused by the introduction of infectious agents, such as bacteria or fungi, into the eye's interior. Understanding the causes and risk factors associated with endophthalmitis is crucial for preventing its occurrence and ensuring timely intervention when necessary.
1. Post-Surgery Infection: Endophthalmitis can develop after eye surgeries, including cataract surgery and vitrectomy. Bacteria or fungi can enter the eye during the surgical procedure, leading to infection. Despite stringent sterile protocols, there is always a minimal risk of introducing pathogens during surgery.
2. Trauma: Trauma to the eye, particularly if it involves penetration or foreign body entry, can provide a route for bacteria to enter the eye's internal structures. Any breach in the eye's protective layers increases the risk of infection.
3. Bacterial Spread: In rare cases, endophthalmitis can result from bacterial infections originating in other parts of the body and spreading to the eye through the bloodstream. This can occur in individuals with weakened immune systems or those with existing systemic infections.
4. Contaminated Instruments or Solutions: Improper sterilization of surgical instruments, equipment, or solutions used during eye surgery can introduce infectious agents into the eye. Ensuring thorough sterilization procedures is vital to prevent post-operative infections.
What Are The Risk Factors of Endophthalmitis?
● Recent Eye Surgery: Individuals who have undergone recent eye surgery are at a higher risk due to the potential introduction of pathogens during the surgical process.
● Compromised Immune System: People with weakened immune systems, such as those with HIV/AIDS or undergoing immunosuppressive therapy, have reduced defense mechanisms against infections.
● Pre-existing Eye Conditions: Certain eye conditions, like diabetic retinopathy or uveitis, can weaken the eye's defenses and make it more susceptible to infections.
● Age: The elderly population has a higher risk of developing endophthalmitis due to age-related changes in the eye's structures and immune responses.
● Contact Lens Wear: Improper hygiene and extended contact lens wear can lead to corneal damage, providing an entry point for infections.
● Systemic Health Issues: Conditions such as diabetes and autoimmune disorders can compromise the body's ability to fight infections, increasing the risk of endophthalmitis.
● Poor Hygiene: Not adhering to proper eye hygiene practices can increase the likelihood of bacterial colonization on the eye's surface.
Diagnosis and Medical Evaluation
Prompt and accurate diagnosis is essential for effective treatment. Ophthalmologists perform a thorough visual examination and might use imaging tests such as ultrasound or optical coherence tomography (OCT) to assess the severity of the infection. Vitreous fluid analysis, obtained through a minimally invasive procedure, helps identify the specific bacteria or pathogens responsible for the infection. This information guides treatment decisions.
Treatment Options for Endophthalmitis
Endophthalmitis, an infection affecting the eye's internal structures, requires immediate and targeted treatment to prevent vision loss and severe complications. The treatment approach depends on the severity of the infection and the causative organism. Here are the primary treatment options for endophthalmitis:
1. Intravitreal Antibiotics
Intravitreal antibiotics involve the injection of antibiotics directly into the vitreous cavity of the eye. This approach ensures high concentrations of antibiotics reach the infection site quickly. Intravitreal antibiotics are effective for treating both bacterial and fungal endophthalmitis. The choice of antibiotic depends on the identified pathogen's susceptibility. Intravitreal injections may need to be repeated, especially in severe cases.
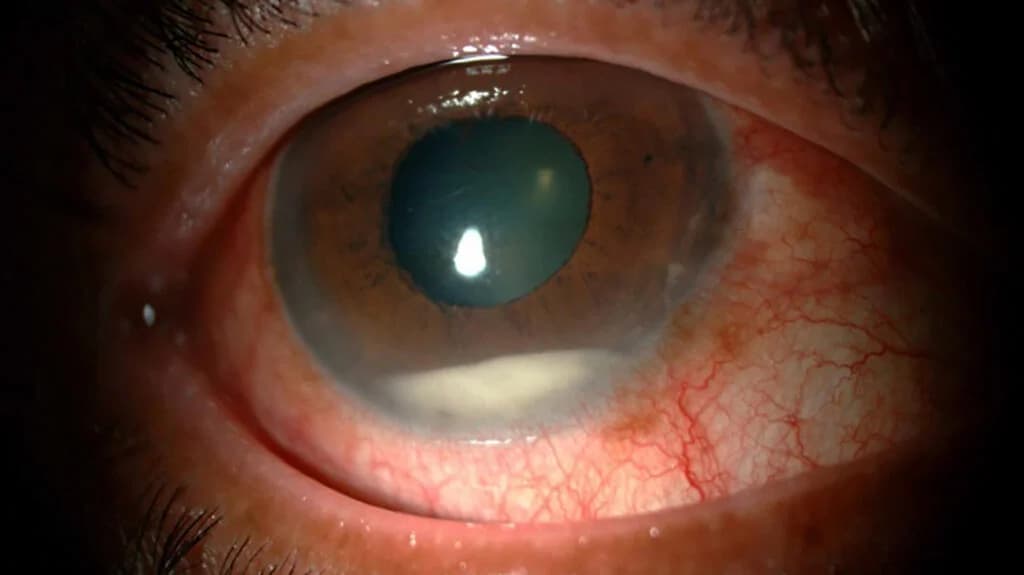
2. Vitrectomy
A vitrectomy is a surgical procedure performed to remove the infected vitreous humor from the eye. This procedure is typically reserved for cases of severe endophthalmitis that do not respond well to intravitreal antibiotics. During the vitrectomy, the vitreous is replaced with a sterile solution, effectively eliminating the source of infection. This procedure aids in reducing inflammation and preventing the spread of infection to other eye structures.
3. Adjunctive Therapy
Adjunctive therapies, such as systemic antibiotics and oral antifungal medications, may be used in combination with intravitreal antibiotics or vitrectomy. Systemic medications help target the infection systemically, reducing the risk of systemic spread of infection.
4. Anti-Inflammatory Agents
Inflammation is a significant concern in endophthalmitis, as it can contribute to vision loss and complications. Anti-inflammatory medications, such as corticosteroids, may be prescribed to reduce inflammation and prevent damage to the retina and other structures.
5. Personalized Treatment Plans
The treatment plan for endophthalmitis is highly individualized, considering factors such as the patient's overall health, the severity of infection, the identified pathogen, and the response to initial treatments. Ophthalmologists work closely with patients to tailor the treatment approach to their specific needs.
6. Supportive Care
Beyond medical interventions, patients are advised to follow strict post-operative care instructions. This may include the use of prescribed eye drops, maintaining good hygiene, and avoiding activities that could strain the eyes during the recovery period.
Is Endophthalmitis Preventable?
Preventing endophthalmitis is a combination of cautious surgical practices and patient awareness. Surgeons must adhere to strict sterile techniques during eye surgeries to minimize the risk of infection. Pre-operative assessments should identify any underlying risk factors in patients. Following eye surgery, regular follow-up appointments enable early detection of potential complications. General health maintenance is also essential, as a strong immune system can aid in preventing infections.
Complications and Prognosis
Endophthalmitis can lead to various complications, including retinal detachment and permanent vision loss. However, the prognosis greatly improves with early detection and swift treatment. Timely intervention can prevent the infection from spreading and causing further damage to the eye's delicate structures. Adherence to post-treatment care instructions is vital to ensure a successful recovery.
Summary
Endophthalmitis is a rare but potentially sight-threatening eye condition that demands prompt attention. Recognizing the symptoms, understanding the causes and risk factors, knowing the treatment options, and implementing prevention strategies can make a significant difference in preserving eye health and preventing long-term complications. If you suspect endophthalmitis or experience any concerning eye symptoms, consult an eye care professional without delay. Your vision is too valuable to take chances with.
(1).jpg)